Back
Poster, Podium & Video Sessions
Moderated Poster
MP30: Global Health/Humanitarian
MP30-15: Association Between Body Mass Index, Metabolic Syndrome, And Urologic Conditions: Results From a Multi-Institutional Database from the United States
Saturday, May 14, 2022
1:00 PM – 2:15 PM
Location: Room 222
Maxwell Towe*, Sirpi Nackeeran, Mohammad Hout, Abhishek Bhat, Ranjith Ramasamy, Hemendra Shah, Miami, FL
- MT
Poster Presenter(s)
Introduction: The link between obesity and metabolic syndrome and poorer health outcomes is well established. We utilized a multi-institutional database and analyzed prevalence rates of several urologic diseases stratified according to body mass index (BMI) and co-occurring metabolic syndrome.
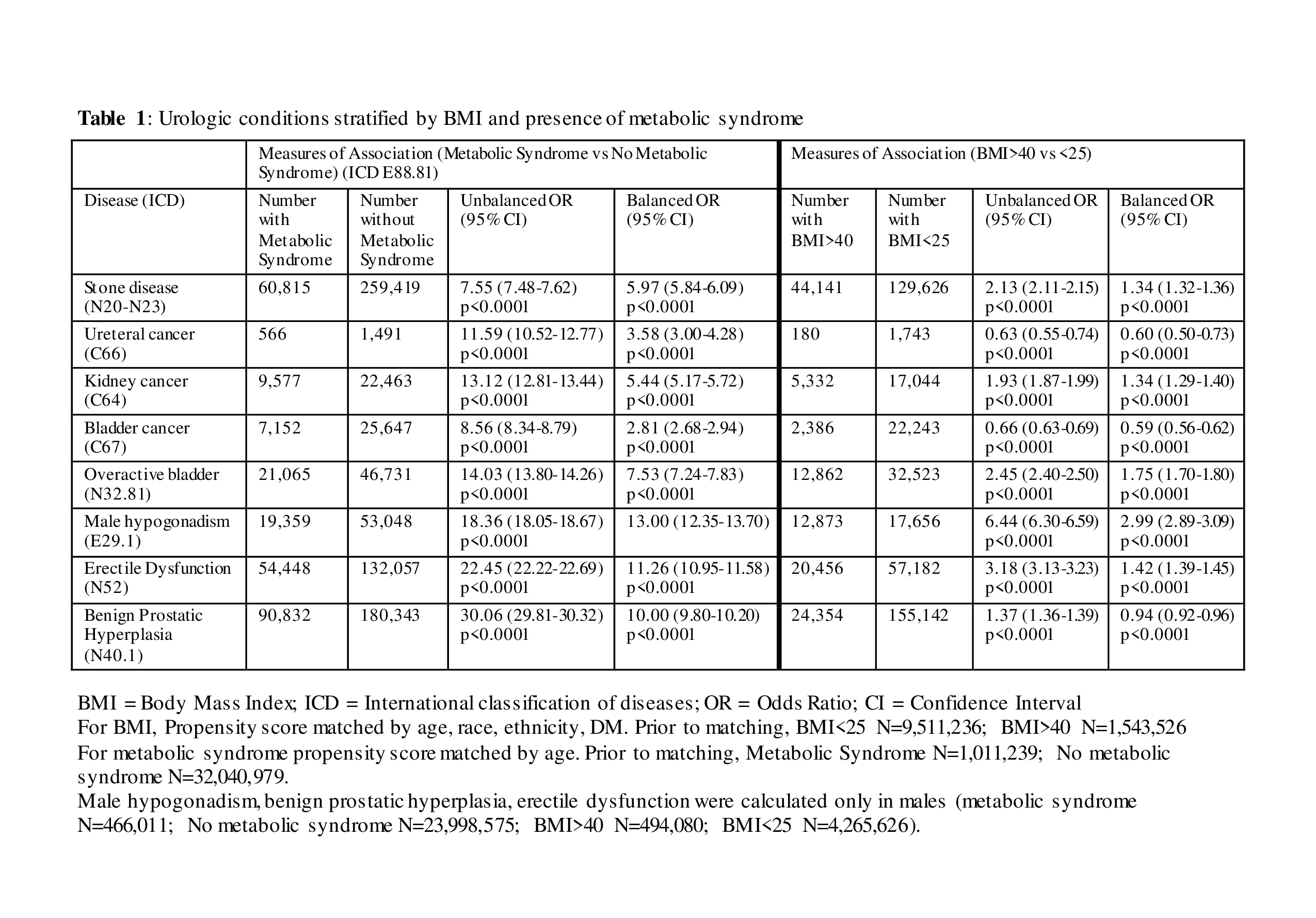
Methods: Using a large multi-center electronic health record network (TRINETx) consisting of 44 healthcare organizations, we conducted a comparative cohort study among individuals stratified by BMI ( <25, 25-30, 30-35, 35-40, >40) and the presence of metabolic syndrome, and determined the prevalence of common urologic conditions among these groups. International classification of diseases codes used to identify urological conditions are detailed in Table 1. Propensity score matching was performed according to age, race, ethnicity, and diabetes mellitus status with both unbalanced and balanced odds ratios (OR) reported.
Results: The total number of individuals aggregated for each BMI cohort are as follows: BMI <25; 9,516,366, BMI 25-30; 6,128,454, BMI 30-35; 3,929,670, BMI 35-40; 1,874,934, and BMI>40; 1,543,526. In general, we found a higher association of multiple urological conditions with increasing BMI. When comparing individuals with BMI <25 vs. >40, there was a much higher prevalence of stone disease (OR: 1.34 [1.32-1.36]; p<0.0001), kidney cancer (OR: 1.34 [1.29-1.40]; p<0.0001), overactive bladder (OR: 1.75 [1.70-1.80]; p<0.0001), hypogonadism (OR: 2.99 [2.89-3.09]; p<0.0001), and erectile dysfunction (OR: 1.42 [1.39-1.45]; p<0.0001) in the morbidly obese group. All urological conditions demonstrated a significant association with co-occurring metabolic syndrome (Table 1).
Conclusions: Higher BMI was associated with increasing prevalence of most urological conditions. Metabolic syndrome proved to be a significant risk factor, with higher ORs reported among individuals with this comorbidity. Interventions aimed at reducing BMI and improving metabolic parameters could play a vital role in reducing the prevalence of these urological conditions and become part of the treatment pathway in the future.
Source of Funding: Research was supported by Acerus Pharmaceuticals in the form of an educational grant used to access the TriNetX database. Acerus Pharmaceuticals was not involved in the planning, design, writing or any other aspect of this project.
This work was also supported by National Institutes of Health Grant R01 DK130991 and Clinician Scientist Development Grant from the American Cancer Society to Ranjith Ramasamy.
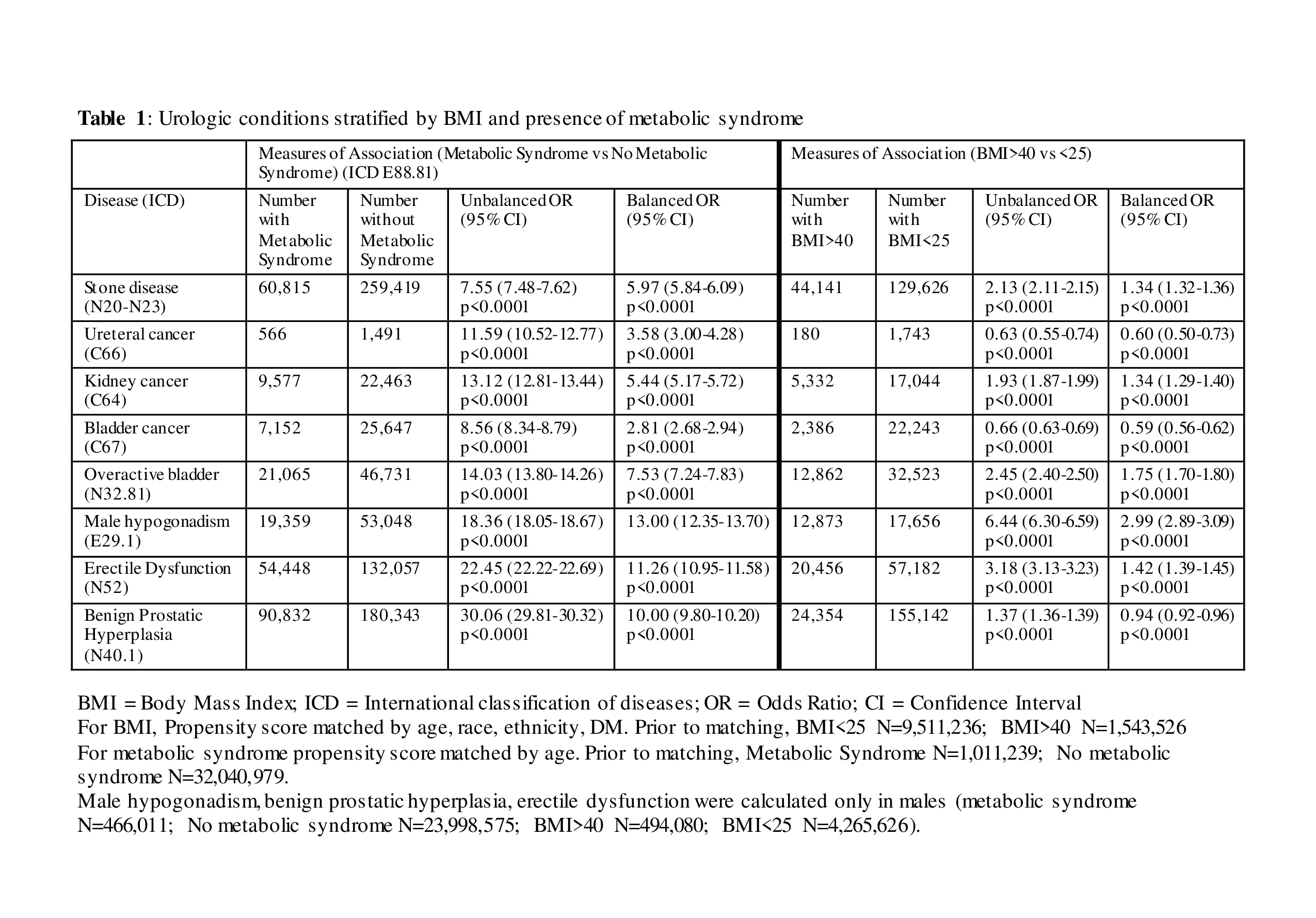
Methods: Using a large multi-center electronic health record network (TRINETx) consisting of 44 healthcare organizations, we conducted a comparative cohort study among individuals stratified by BMI ( <25, 25-30, 30-35, 35-40, >40) and the presence of metabolic syndrome, and determined the prevalence of common urologic conditions among these groups. International classification of diseases codes used to identify urological conditions are detailed in Table 1. Propensity score matching was performed according to age, race, ethnicity, and diabetes mellitus status with both unbalanced and balanced odds ratios (OR) reported.
Results: The total number of individuals aggregated for each BMI cohort are as follows: BMI <25; 9,516,366, BMI 25-30; 6,128,454, BMI 30-35; 3,929,670, BMI 35-40; 1,874,934, and BMI>40; 1,543,526. In general, we found a higher association of multiple urological conditions with increasing BMI. When comparing individuals with BMI <25 vs. >40, there was a much higher prevalence of stone disease (OR: 1.34 [1.32-1.36]; p<0.0001), kidney cancer (OR: 1.34 [1.29-1.40]; p<0.0001), overactive bladder (OR: 1.75 [1.70-1.80]; p<0.0001), hypogonadism (OR: 2.99 [2.89-3.09]; p<0.0001), and erectile dysfunction (OR: 1.42 [1.39-1.45]; p<0.0001) in the morbidly obese group. All urological conditions demonstrated a significant association with co-occurring metabolic syndrome (Table 1).
Conclusions: Higher BMI was associated with increasing prevalence of most urological conditions. Metabolic syndrome proved to be a significant risk factor, with higher ORs reported among individuals with this comorbidity. Interventions aimed at reducing BMI and improving metabolic parameters could play a vital role in reducing the prevalence of these urological conditions and become part of the treatment pathway in the future.
Source of Funding: Research was supported by Acerus Pharmaceuticals in the form of an educational grant used to access the TriNetX database. Acerus Pharmaceuticals was not involved in the planning, design, writing or any other aspect of this project.
This work was also supported by National Institutes of Health Grant R01 DK130991 and Clinician Scientist Development Grant from the American Cancer Society to Ranjith Ramasamy.

.jpg)
.jpg)