Back
Poster, Podium & Video Sessions
Moderated Poster
MP30: Global Health/Humanitarian
MP30-19: The Rakai Score: A novel tool for pain measurement during early infant male circumcision with the ShangRing
Saturday, May 14, 2022
1:00 PM – 2:15 PM
Location: Room 222
Aaron Brant, Christina Sze, Jeffrey Johnson*, Spyridon Basourakos, Quincy Nang, New York, NY, Stephen Kiboneka, Joseph Kagayi, Kalisizo, Uganda, Alice Christensen, Dar Es Alaam, Tanzania-United Republic, Mark Barone, Marc Goldstein, Kaylee Ho, Karla Ballman, Philip Li, New York, NY, Godfrey Kigozi, Kalisizo, Uganda, Richard Lee, New York, NY
- JJ
Poster Presenter(s)
Introduction: Measurement of pain in infants can be challenging due to an inability to communicate level of discomfort directly. Therefore, providers are forced to rely on secondary proxies for discomfort, resulting in a nonspecific or inaccurate measurement. In this study, we present the use of the novel Rakai scale for the measurement of pain during early infant circumcision (EIMC) using ShangRing (SR) in our recent clinical trials in Uganda, Tanzania, and Kenya.
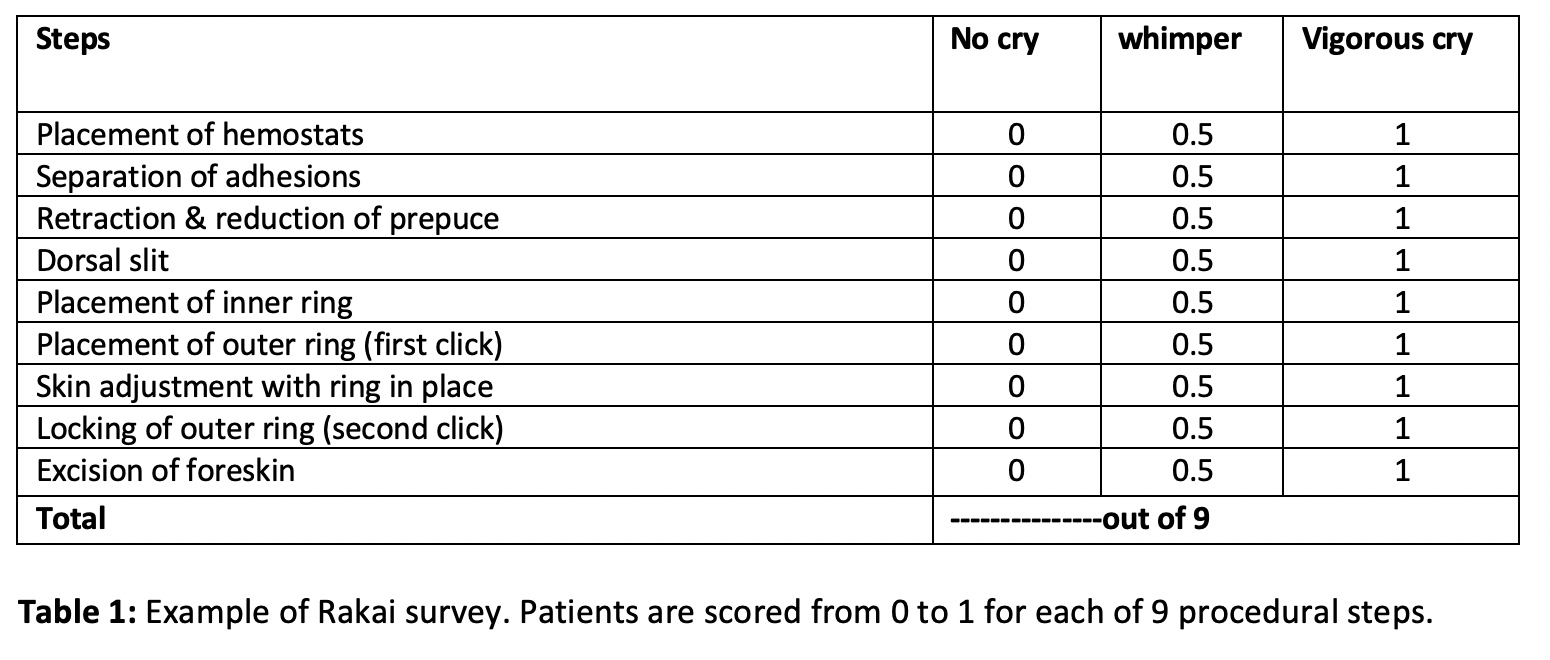
Methods: Male infants aged 0 – 60 days were brought to 14 sites in Kenya, Tanzania, and Uganda by a parent or legally appointed representative for SR EIMC from February to December 2020. Infants with congenital genitourinary anomalies, bleeding diatheses, or allergy to local anesthetics were excluded. Topical anesthesia was administered, with additional local injectable anesthesia given if needed. Infants were scored on both the nine-point Rakai scale during SR placement (Table 1) as well as the seven-point Neonatal Infant Pain Scale (NIPS) post-operatively.
Results: Rakai and NIPS scores were completed for 1,690 of 1,691 infants (99.9%) who underwent SR placement. The mean procedure time was 10.1 minutes (standard deviation (STD): 5.3). Additional injectable anesthesia was needed for 44 infants (2.6%). Mean Rakai Score was 3.6 of 9 (STD: 2.6). The highest scored portion of the procedure was “skin adjustment with the ring in place” (mean 0.52 of 1), and the lowest scored portion was “placement of hemostats” (mean 0.24 of 1). Severe Rakai Score (>6 of 9) was recorded in 303 infants (17.9%). Mean NIPS Score was 0.3 of 7 (STD: 0.8), with “flexed or extended arms” the highest scored portion (mean 0.06 of 1). A severe NIPS score (=5 of 7) was recorded in 8 infants (0.5%).
Conclusions: In a large prospective study of male newborn infants undergoing SR placement, the Rakai Score captured infant pain at each step of the procedure with a higher rate of severe pain detection than the NIPS score administered post-operatively. Thus, the Rakai score may be superior to pre-existing tools such as the NIPS score for pain measurement during SR EIMC due to its detection of intraprocedural pain with more significant detection of severe pain.
Source of Funding: None
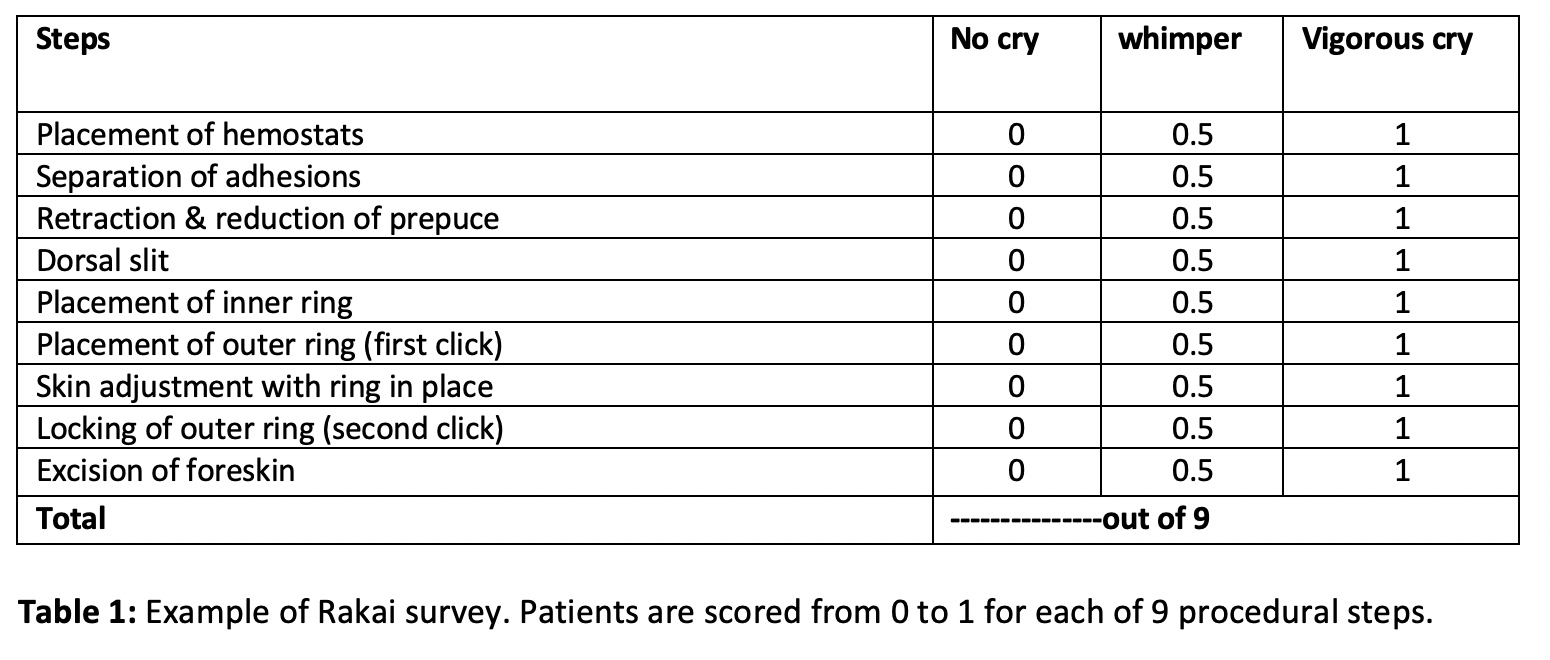
Methods: Male infants aged 0 – 60 days were brought to 14 sites in Kenya, Tanzania, and Uganda by a parent or legally appointed representative for SR EIMC from February to December 2020. Infants with congenital genitourinary anomalies, bleeding diatheses, or allergy to local anesthetics were excluded. Topical anesthesia was administered, with additional local injectable anesthesia given if needed. Infants were scored on both the nine-point Rakai scale during SR placement (Table 1) as well as the seven-point Neonatal Infant Pain Scale (NIPS) post-operatively.
Results: Rakai and NIPS scores were completed for 1,690 of 1,691 infants (99.9%) who underwent SR placement. The mean procedure time was 10.1 minutes (standard deviation (STD): 5.3). Additional injectable anesthesia was needed for 44 infants (2.6%). Mean Rakai Score was 3.6 of 9 (STD: 2.6). The highest scored portion of the procedure was “skin adjustment with the ring in place” (mean 0.52 of 1), and the lowest scored portion was “placement of hemostats” (mean 0.24 of 1). Severe Rakai Score (>6 of 9) was recorded in 303 infants (17.9%). Mean NIPS Score was 0.3 of 7 (STD: 0.8), with “flexed or extended arms” the highest scored portion (mean 0.06 of 1). A severe NIPS score (=5 of 7) was recorded in 8 infants (0.5%).
Conclusions: In a large prospective study of male newborn infants undergoing SR placement, the Rakai Score captured infant pain at each step of the procedure with a higher rate of severe pain detection than the NIPS score administered post-operatively. Thus, the Rakai score may be superior to pre-existing tools such as the NIPS score for pain measurement during SR EIMC due to its detection of intraprocedural pain with more significant detection of severe pain.
Source of Funding: None

.jpg)
.jpg)