Back
Poster, Podium & Video Sessions
Moderated Poster
MP31: Health Services Research: Quality Improvement & Patient Safety II
MP31-04: Passive Opioid Stewardship Initiatives Associated with Significant Change in Opioid Prescribing Following Urologic Surgery
Saturday, May 14, 2022
2:45 PM – 4:00 PM
Location: Room 228
Tudor Borza, Emily Serrell*, Manasa Venkatesh, Jeremy Goodman, Elise Lawson, Sudha Quamme, Kyle Richards, David Jarrard, Madison, WI, Caprice Greenberg, Augusta, GA, Corrine Voils, Jessica Schumacher, Madison, WI

Emily C. Serrell, MD
University of Wisconsin
Poster Presenter(s)
Introduction: Post-operative overprescribing contributes to the opioid epidemic by (i) leading to persistent use and (ii) increasing the supply of opioids available for non-medical use. We evaluate the impact since 2017 of passive stewardship initiatives, where no direct urologist engagement occurred (e.g., Prescription Drug Monitoring Plan (PDMP), continuing medical education, new guidelines), on statewide prescribing patterns following common urologic procedures.
Methods: We used Wisconsin (WI) Health Information Organization data, an all-payer claims database covering 75% of WI population, to identify patients undergoing office (vasectomy), stone (ureteroscopy, ESWL), endoscopic (TURP, TURBT) and major (prostatectomy, nephrectomy) surgery in the one-year period prior to June 30, 2018 and 2020. We captured filled opioid prescriptions within 14 days of discharge and identified dose (median morphine milligram equivalents, MME) and duration (median days) for the initial prescription. We compared prescribing between 2018 and 2020 to assess for change in practice patterns.
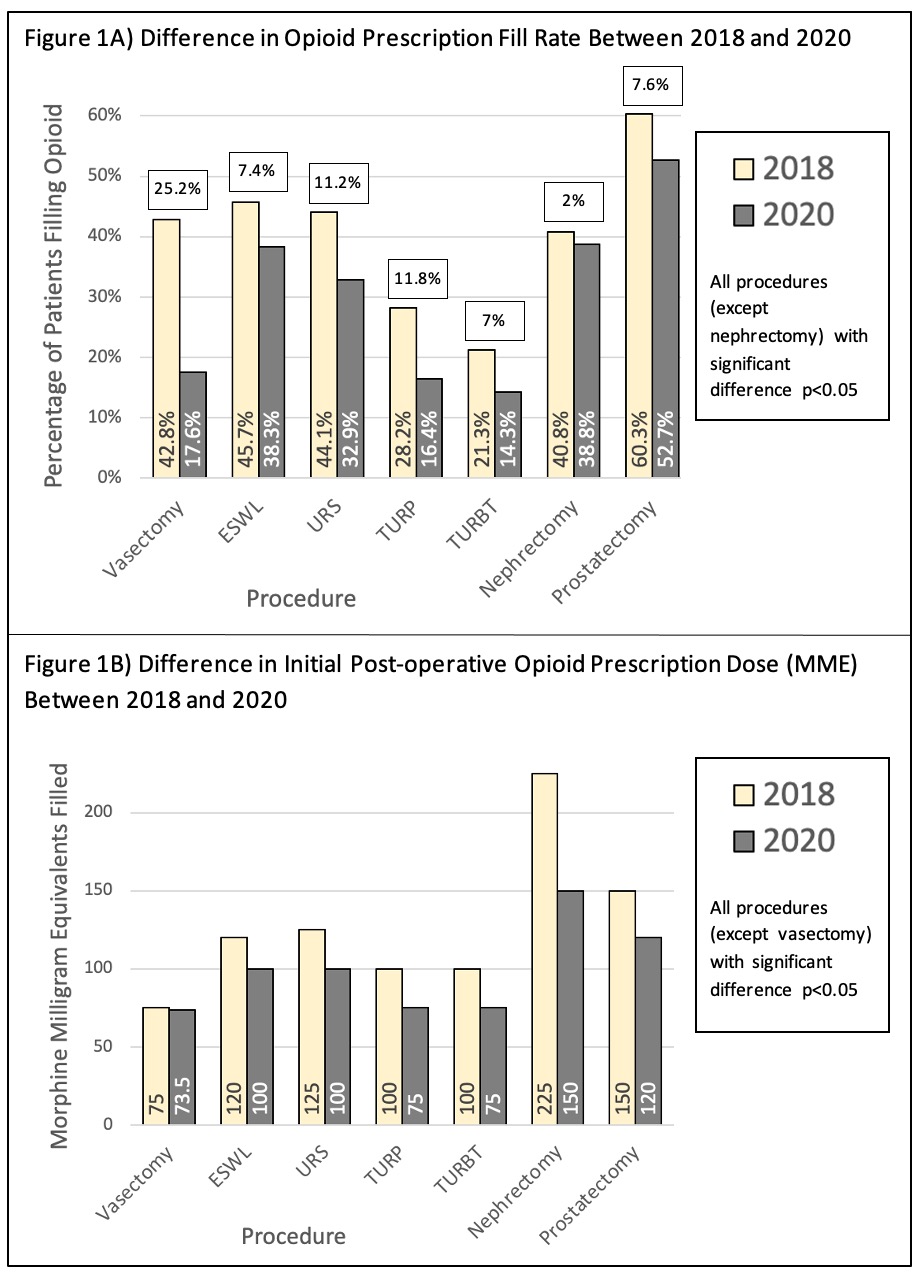
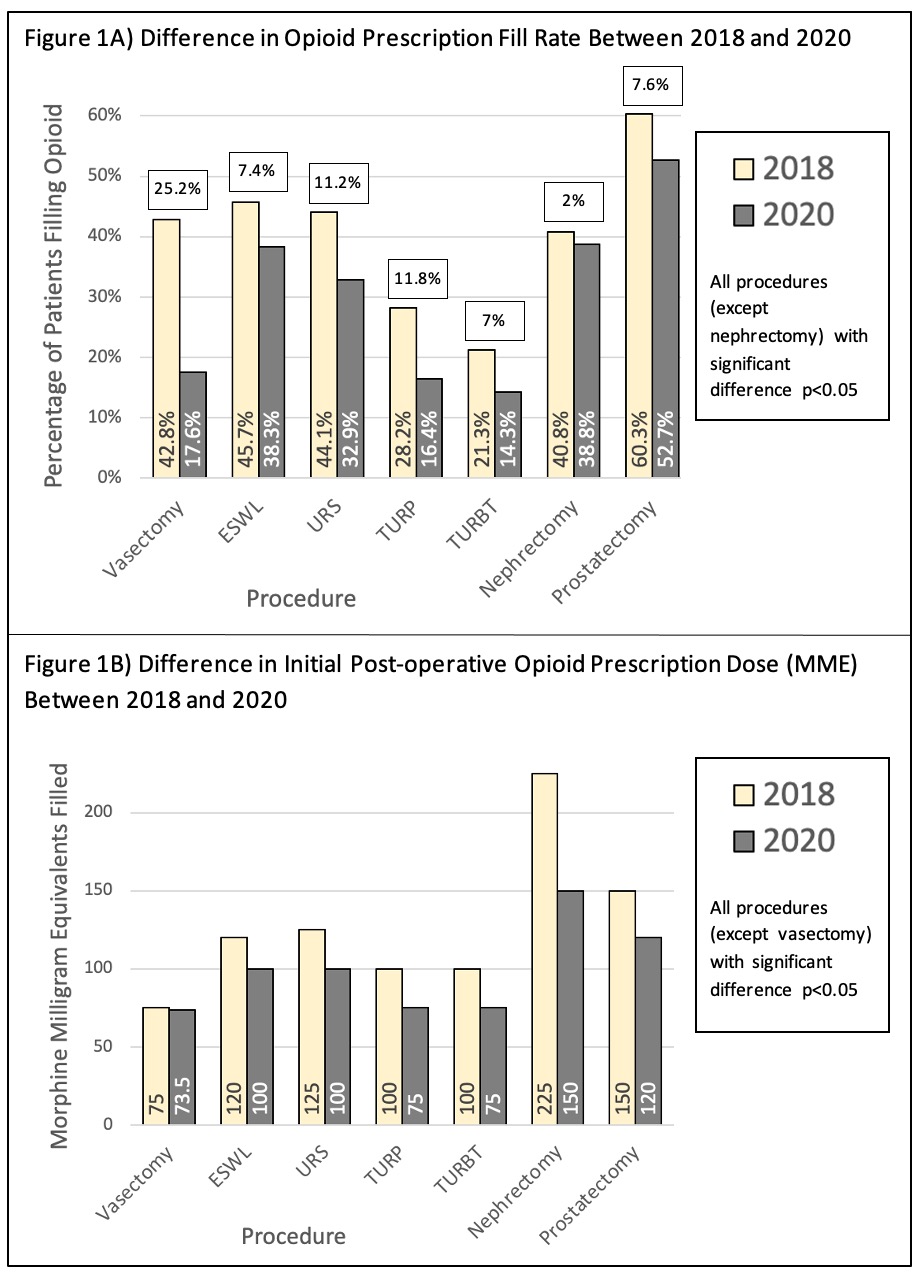
Results: We identified 4,234 patients (1238 vasectomy, 1143 ureteroscopy, 361 ESWL, 432 TURP, 550 TURBT, 292 prostatectomy, 218 nephrectomy) in 2018 and 5,095 patients (1542 vasectomy, 1575 ureteroscopy, 394 ESWL, 482 TURP, 518 TURBT, 357 prostatectomy, 227 nephrectomy) in 2020. Overall, 40.2% and 26.9% (p100% (Fig 1B).
Conclusions: Passive stewardship initiatives in WI led to significant decrease in opioid prescribing. This was driven by decreased fill rates, which captured a combination of decreased prescribing and patients choosing not to fill. Despite the decrease, prescribing remains above recommended levels. Active interventions focused on direct urologist engagement may lead to further improvement in opioid stewardship.
Source of Funding: n/a
Methods: We used Wisconsin (WI) Health Information Organization data, an all-payer claims database covering 75% of WI population, to identify patients undergoing office (vasectomy), stone (ureteroscopy, ESWL), endoscopic (TURP, TURBT) and major (prostatectomy, nephrectomy) surgery in the one-year period prior to June 30, 2018 and 2020. We captured filled opioid prescriptions within 14 days of discharge and identified dose (median morphine milligram equivalents, MME) and duration (median days) for the initial prescription. We compared prescribing between 2018 and 2020 to assess for change in practice patterns.
Results: We identified 4,234 patients (1238 vasectomy, 1143 ureteroscopy, 361 ESWL, 432 TURP, 550 TURBT, 292 prostatectomy, 218 nephrectomy) in 2018 and 5,095 patients (1542 vasectomy, 1575 ureteroscopy, 394 ESWL, 482 TURP, 518 TURBT, 357 prostatectomy, 227 nephrectomy) in 2020. Overall, 40.2% and 26.9% (p100% (Fig 1B).
Conclusions: Passive stewardship initiatives in WI led to significant decrease in opioid prescribing. This was driven by decreased fill rates, which captured a combination of decreased prescribing and patients choosing not to fill. Despite the decrease, prescribing remains above recommended levels. Active interventions focused on direct urologist engagement may lead to further improvement in opioid stewardship.
Source of Funding: n/a

.jpg)
.jpg)