Back
Poster, Podium & Video Sessions
Moderated Poster
MP31: Health Services Research: Quality Improvement & Patient Safety II
MP31-09: Decreased Ureteral Stent Duration After Radical Cystectomy and Ileal Conduit Urinary Diversion Is Associated with Decreased Rate of 30 and 90-day Complications
Saturday, May 14, 2022
2:45 PM – 4:00 PM
Location: Room 228
David Miller*, Danielle Sharbaugh, Cameron Jones, John Myrga, Jennifer Mihalo, Michelle Yu, Tatum Tarin, Robert Turner, Bishoy Gayed, Benjamin Davies, Bruce Jacobs, Pittsburgh, PA

David Miller, MD
University of Miami
Poster Presenter(s)
Introduction: The rate of complications for patients who undergo radical cystectomy and ileal conduit urinary diversion remains among the highest of all oncologic surgeries. An effort to reduce complication rates is decreased duration of indwelling ureteral stents after urinary diversion. Our objective was to examine the association of stent duration on 30 and 90-day complication and readmission rates among patients with bladder cancer undergoing radical cystectomy and ileal conduit urinary diversion.
Methods: We identified patients who underwent radical cystectomy and ileal conduit diversion for bladder cancer at our institution from February of 2020 to July of 2021. Variation in stent duration within our cohort reflects surgeon practice in addition to initiation of a bladder cancer care protocol for patients undergoing radical cystectomy. Stent duration was stratified into three groups: =10 days, <10 days, and no stents. 30 and 90-day readmissions and complications were recorded including urine leak, pyelonephritis, urosepsis, ileus, small bowel obstruction, and other. Kruskal-Wallis, Chi-square and Fisher’s exact tests were used to assess differences between groups.
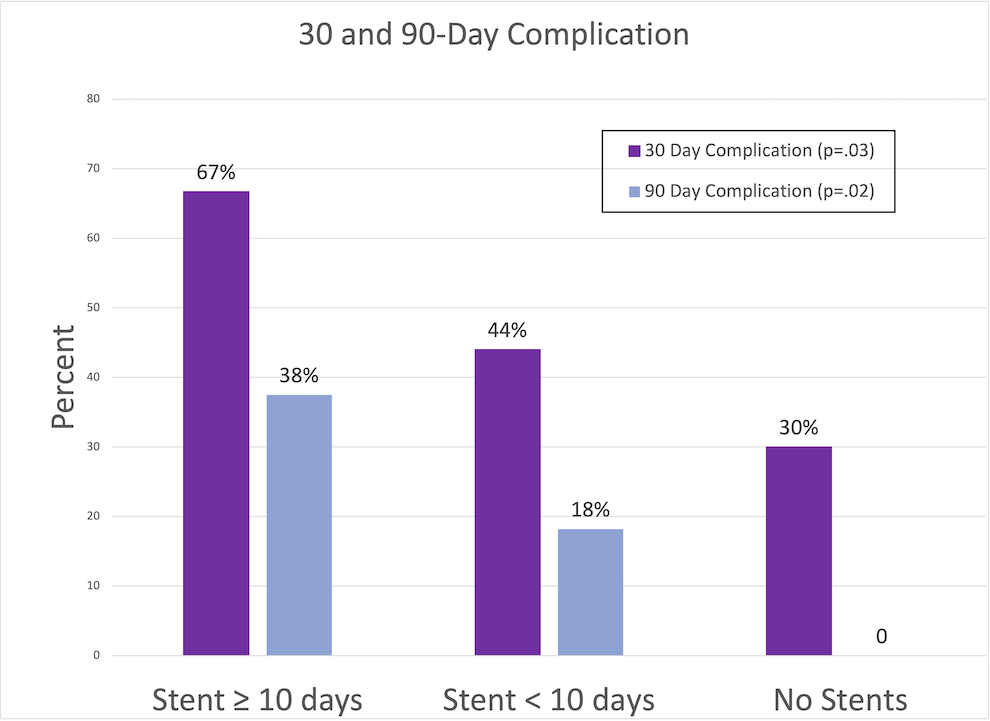
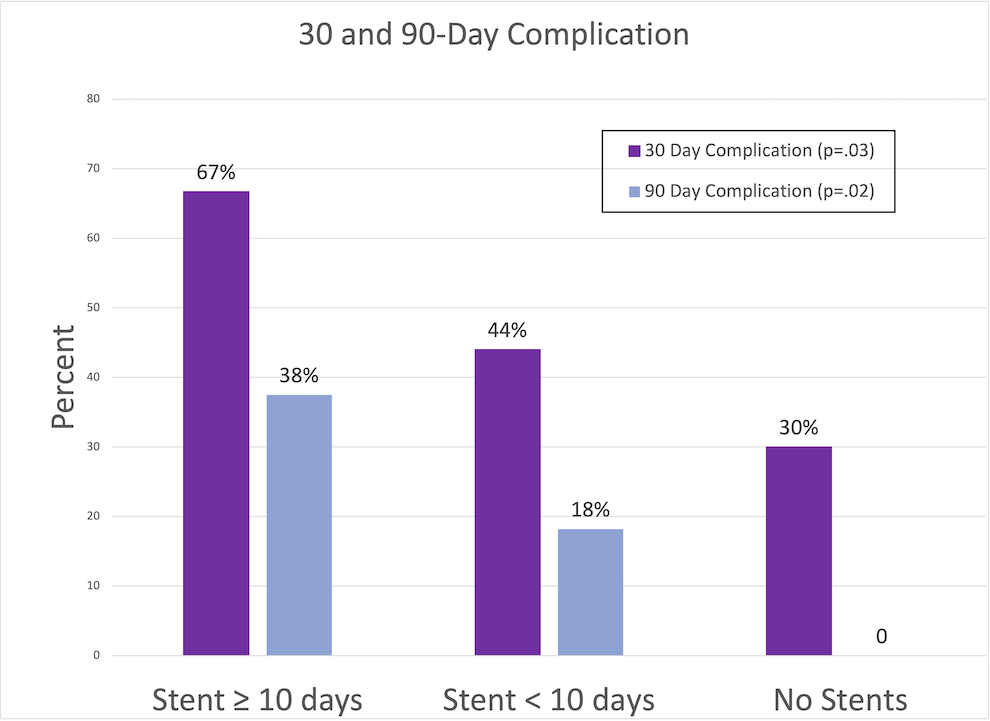
Results: We identified 128 patients with bladder cancer who underwent radical cystectomy with ileal conduit urinary diversion, 45 patients were in the =10-day group, 73 in the <10 days group, and 10 in the no stents group. No significant difference in hospital length of stay was seen (p=.34). There was a significant decrease in overall 30-day complication rate (p=.03) and 90-day complication rate (p=.02) as time of stent duration decreased. Specifically. there was a significant decrease in the development of urosepsis (p=.02) and pyelonephritis (p=.05) as duration of stent decreased. There was a significant decrease in the rate of urine leak by stent duration between groups (p=.01), this is explained by ureteral stents remaining in place if a urine leak is identified. No significant differences in rate of the other complications nor rate of readmissions were seen between the groups.
Conclusions: Decreased time of indwelling ureteral stents resulted in significantly decreased overall 30 and 90-day complications. Further research is needed to assess differences in long term complications.
Source of Funding: Bruce Jacobs is supported in part by the Shadyside Hospital Foundation
Methods: We identified patients who underwent radical cystectomy and ileal conduit diversion for bladder cancer at our institution from February of 2020 to July of 2021. Variation in stent duration within our cohort reflects surgeon practice in addition to initiation of a bladder cancer care protocol for patients undergoing radical cystectomy. Stent duration was stratified into three groups: =10 days, <10 days, and no stents. 30 and 90-day readmissions and complications were recorded including urine leak, pyelonephritis, urosepsis, ileus, small bowel obstruction, and other. Kruskal-Wallis, Chi-square and Fisher’s exact tests were used to assess differences between groups.
Results: We identified 128 patients with bladder cancer who underwent radical cystectomy with ileal conduit urinary diversion, 45 patients were in the =10-day group, 73 in the <10 days group, and 10 in the no stents group. No significant difference in hospital length of stay was seen (p=.34). There was a significant decrease in overall 30-day complication rate (p=.03) and 90-day complication rate (p=.02) as time of stent duration decreased. Specifically. there was a significant decrease in the development of urosepsis (p=.02) and pyelonephritis (p=.05) as duration of stent decreased. There was a significant decrease in the rate of urine leak by stent duration between groups (p=.01), this is explained by ureteral stents remaining in place if a urine leak is identified. No significant differences in rate of the other complications nor rate of readmissions were seen between the groups.
Conclusions: Decreased time of indwelling ureteral stents resulted in significantly decreased overall 30 and 90-day complications. Further research is needed to assess differences in long term complications.
Source of Funding: Bruce Jacobs is supported in part by the Shadyside Hospital Foundation

.jpg)
.jpg)