Back
Poster, Podium & Video Sessions
Moderated Poster
MP33: Uroradiology I
MP33-06: Predicting Renal Tumor Growth in von Hippel-Lindau (VHL) Patients from Magnetic Resonance Imaging (MRI) Features: A Pilot Study of the Kidney Imaging Surveillance Scoring System (KISSS)
Saturday, May 14, 2022
4:30 PM – 5:45 PM
Location: Room 228
Nikhil Gopal*, Pouria Yazdian, Aditi Chaurasia, Maria Antony, Safa Samimi, Rabindra Gautam, Elizabeth Jones, Mark Ball, W. Marston Linehan, Evrim Turkbey, Ashkan Malayeri, Bethesda, MD

Nikhil Gopal, MD
Clinical Fellow - Urologic Oncology Branch - National Cancer Institute
National Cancer Institute - Urologic Oncology Branch
Poster Presenter(s)
Introduction: VHL disease is characterized by multifocal, bilateral clear cell renal tumors with variable growth. We determined the reliability and preliminary efficacy of an image-based scoring system utilizing qualitative tumor features from a single MRI study, with the aim of predicting renal tumor growth rate and thus tailoring surveillance imaging frequency.
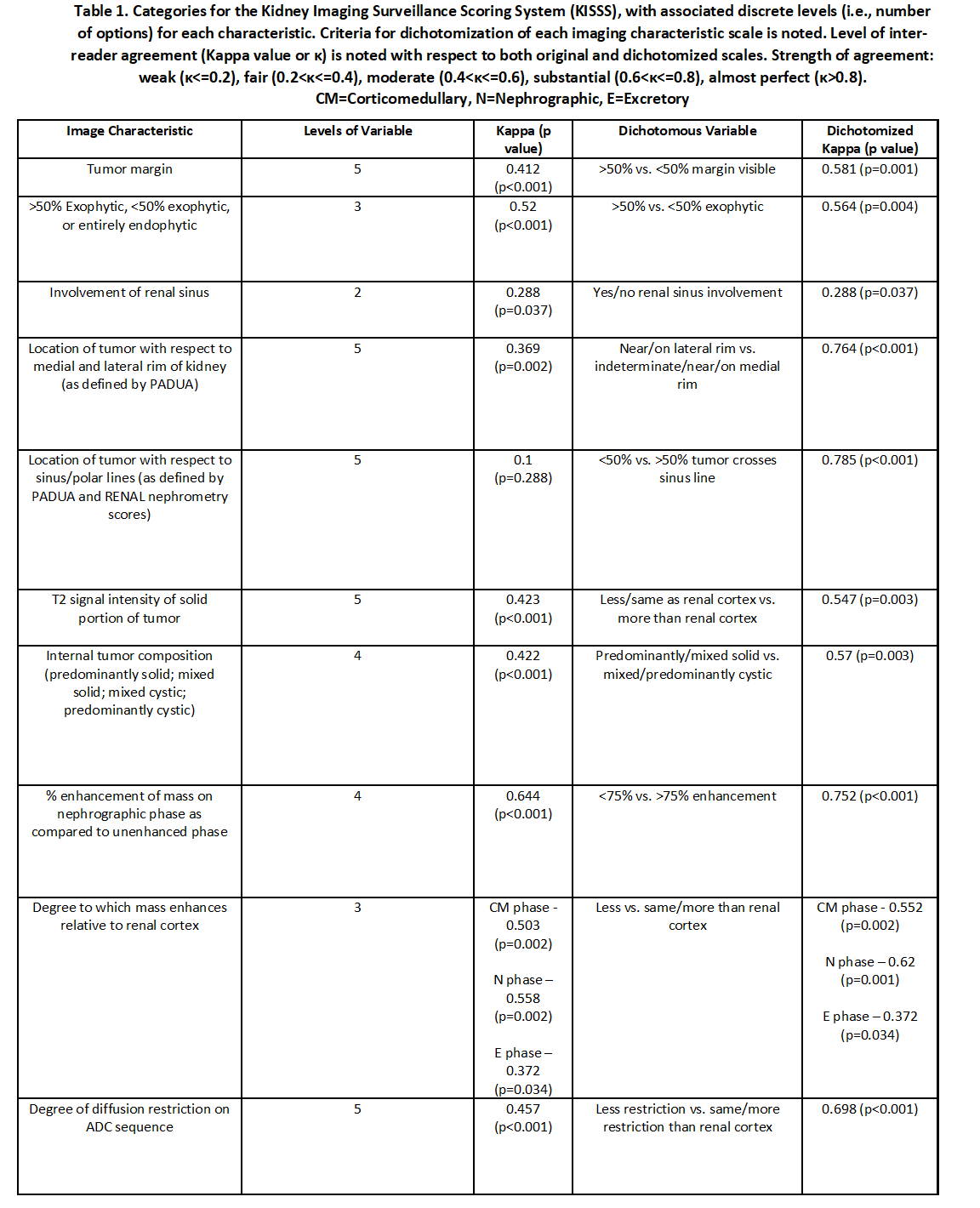
Methods: We collected records of VHL patients on an IRB approved protocol who underwent renal surgery from 2015-2020 at the National Cancer Institute, with at least two preoperative MRIs. A subset of these 79 patients with 253 tumors was considered for our pilot study. Two fellowship trained body radiologists, blinded to growth rate information, answered questions about tumor features (Table 1) based on the earlier preoperative MRI.
Inter-reader reliability was done using Cohen’s kappa (?). Growth rate was calculated as the change in maximum single tumor dimension over time. Scales for each question were dichotomized, with cutoffs based on maximum reliability. Mann-Whitney U test was used to compare growth rates between groups. P <= 0.05 was significant. Analysis was done using SPSS version 26.0.0.
Results: 15 patients (30 tumors) were studied. Mean tumor size was 2.4 cm (1.3 – 4.0 cm). There was an average of 1.1 years between MRIs. Mean tumor growth rate was 0.45 cm/year (0-2.32 cm/year).
Moderate inter-radiologist agreement (?>0.40) was noted for two thirds of imaging characteristics. With dichotomized scales, reliability improved, with moderate agreement for 83% and substantial agreement (?>0.60) for 42% of imaging features. Faster mean growth rates (MGR) were seen in masses scored as reduced T2 intensity (Reader 1 MGR 0.61 vs. 0.23 cm/yr, p=0.028; Reader 2 MGR 0.58 vs. 0.37 cm/yr, p=0.030) and reduced enhancement on delayed contrast phase (Reader 1 MGR 0.62 vs. 0.17 cm/yr, p=0.006; Reader 2 MGR 0.52 vs. 0.16 cm/yr; p=0.054).
Conclusions: In this preliminary scoring system assessment, moderate reliability was noted for most MRI measures that improved with dichotomization of scales. The relationship of faster renal tumor growth with T2 hypointensity and T1 hypoenhancement on delayed phase of a single MRI is novel and will be validated in our full study.
Source of Funding: This study has received funding by Intramural Research programs of The Center for Cancer Research –National Cancer Institute and the National Institutes of Health Clinical Center, Bethesda, Maryland, USA
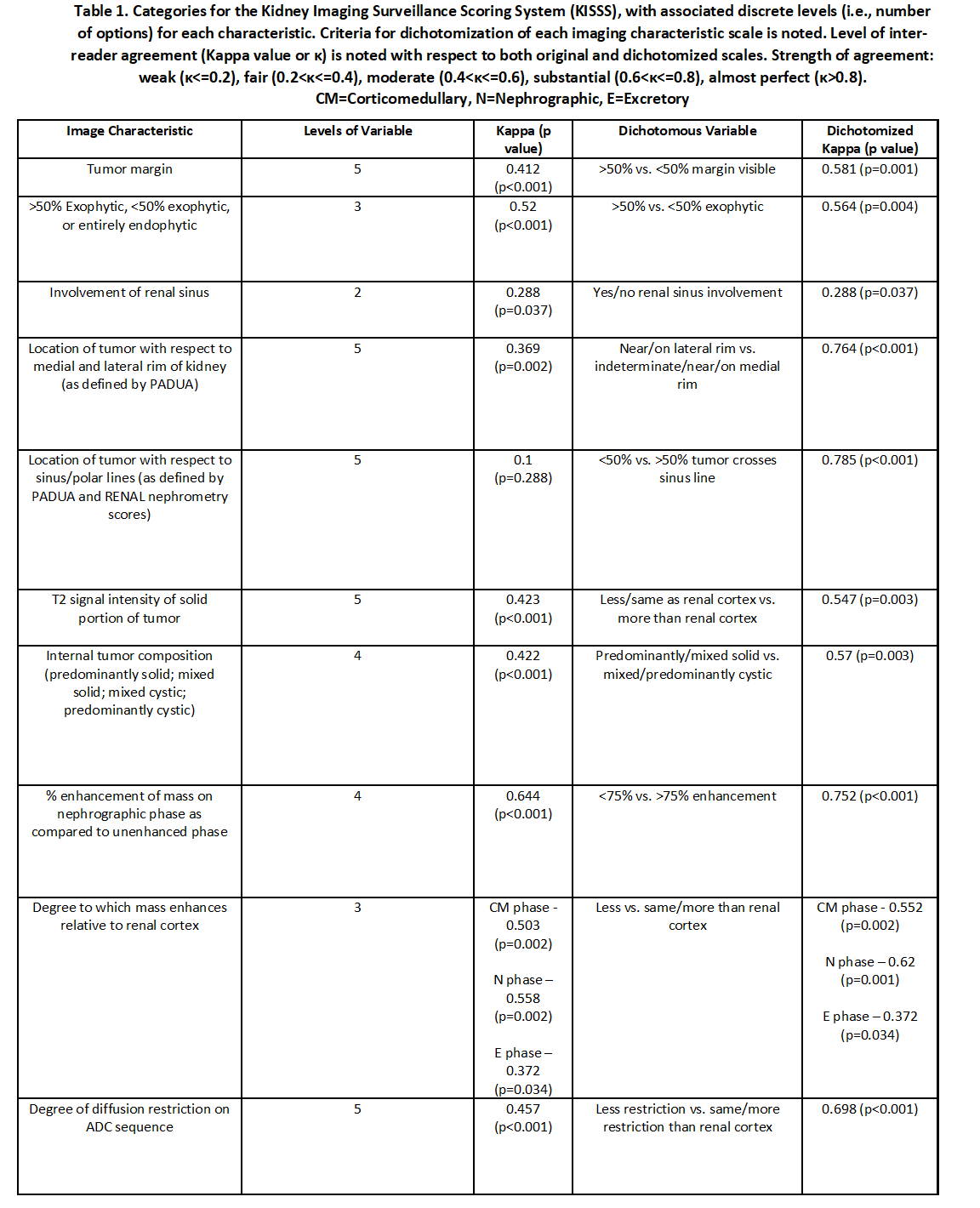
Methods: We collected records of VHL patients on an IRB approved protocol who underwent renal surgery from 2015-2020 at the National Cancer Institute, with at least two preoperative MRIs. A subset of these 79 patients with 253 tumors was considered for our pilot study. Two fellowship trained body radiologists, blinded to growth rate information, answered questions about tumor features (Table 1) based on the earlier preoperative MRI.
Inter-reader reliability was done using Cohen’s kappa (?). Growth rate was calculated as the change in maximum single tumor dimension over time. Scales for each question were dichotomized, with cutoffs based on maximum reliability. Mann-Whitney U test was used to compare growth rates between groups. P <= 0.05 was significant. Analysis was done using SPSS version 26.0.0.
Results: 15 patients (30 tumors) were studied. Mean tumor size was 2.4 cm (1.3 – 4.0 cm). There was an average of 1.1 years between MRIs. Mean tumor growth rate was 0.45 cm/year (0-2.32 cm/year).
Moderate inter-radiologist agreement (?>0.40) was noted for two thirds of imaging characteristics. With dichotomized scales, reliability improved, with moderate agreement for 83% and substantial agreement (?>0.60) for 42% of imaging features. Faster mean growth rates (MGR) were seen in masses scored as reduced T2 intensity (Reader 1 MGR 0.61 vs. 0.23 cm/yr, p=0.028; Reader 2 MGR 0.58 vs. 0.37 cm/yr, p=0.030) and reduced enhancement on delayed contrast phase (Reader 1 MGR 0.62 vs. 0.17 cm/yr, p=0.006; Reader 2 MGR 0.52 vs. 0.16 cm/yr; p=0.054).
Conclusions: In this preliminary scoring system assessment, moderate reliability was noted for most MRI measures that improved with dichotomization of scales. The relationship of faster renal tumor growth with T2 hypointensity and T1 hypoenhancement on delayed phase of a single MRI is novel and will be validated in our full study.
Source of Funding: This study has received funding by Intramural Research programs of The Center for Cancer Research –National Cancer Institute and the National Institutes of Health Clinical Center, Bethesda, Maryland, USA

.jpg)
.jpg)