Back
Poster, Podium & Video Sessions
Moderated Poster
MP33: Uroradiology I
MP33-08: Deep Learning Renal Volume Analysis to Predict Long-Term Renal Function after Partial and Radical Nephrectomy
Saturday, May 14, 2022
4:30 PM – 5:45 PM
Location: Room 228
Abhinav Khanna*, Vidit Sharma, Adriana Gregory, Christine Lohse, Harrison C. Gottlich, Theodora Potretzke, R. Houston Thompson, Stephen A. Boorjian, Bradley Leibovich, Timothy Kline, Aaron Potretzke, Rochester, MN
- AK
Abhinav Khanna, MD
Mayo Clinic
Poster Presenter(s)
Introduction: Post-operative renal function (PORF) following extirpative renal surgery is largely dependent upon pre-operative renal function and the amount of renal parenchyma spared. The latter is often difficult to quantify. Some authors have suggested that renal volume on cross-sectional imaging may correlate with PORF. However, the calculation of renal volume is resource-intensive and does not translate readily into clinical practice. We aim to develop a deep learning algorithm capable of automatically calculating renal volume based on pre-operative MRI images.
Methods: We identified patients undergoing partial nephrectomy (PN) or radical nephrectomy (RN) at our tertiary referral center with accessible pre-operative MRI images. We developed a novel deep learning algorithm using U-Net architecture to identify kidneys on T2-weighted MRI and quantify non-neoplastic renal parenchymal volume (RV). The cohort was divided into a 74/13/13% split of training/validation/test subsets. Model development was carried out using a 5-fold cross validation technique. An ensemble of the three best performing models on the training and validation subsets was implemented to generate a more robust prediction segmentation. The associations between height-normalized pre-operative RV and PORF were assessed using generalized linear mixed effect models, adjusted for known clinical factors associated with PORF (age, diabetes, preoperative eGFR, proteinuria, tumor size, time from surgery).
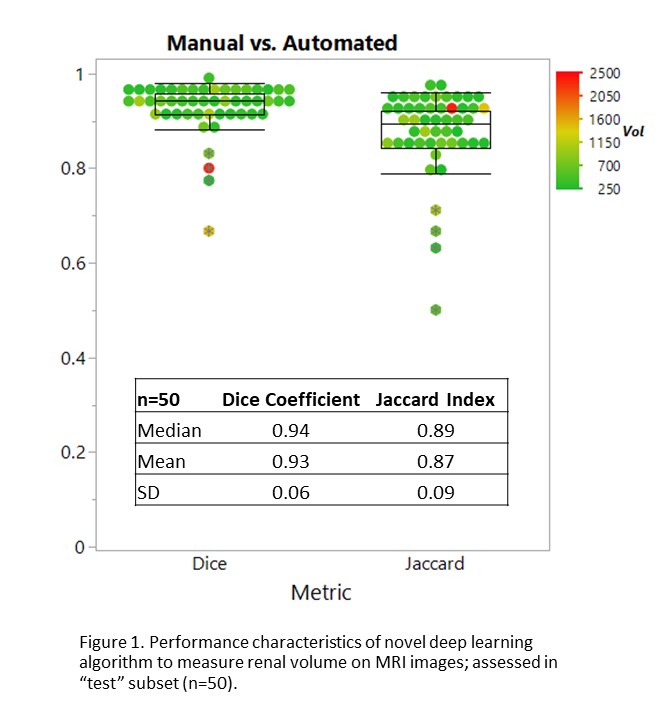
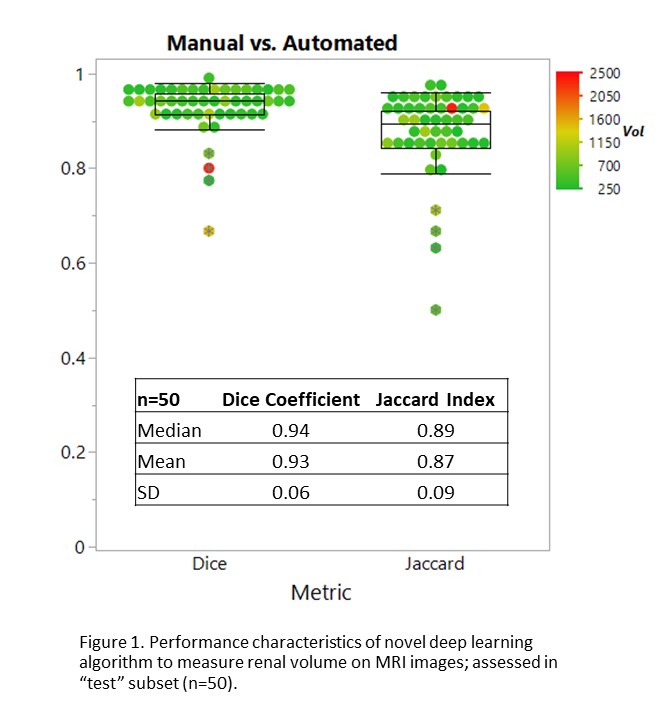
Results: MRI images from from 330 patients, including 208 PN and 122 RN were used to develop a deep learning algorithm with a final Dice coefficient of 0.93 and Jaccard index of 0.87 compared to manual segmentations (Figure 1). On unadjusted analyses, RV was associated with PORF following PN and RN (p < 0.001 and p=0.008, respectively). When added to existing multivariable models to predict PORF, the associations between RV and PORF remained statistically significant (p < 0.001 and p=0.05, respectively).
Conclusions: Pre-operative non-neoplastic renal volume is associated with long-term renal function following PN and RN, even after adjusting for a previously validated clinical prediction model. We developed a deep learning tool to facilitate automated RV assessment, which may promote integration of RV measurement into clinical practice.
Source of Funding: None
Methods: We identified patients undergoing partial nephrectomy (PN) or radical nephrectomy (RN) at our tertiary referral center with accessible pre-operative MRI images. We developed a novel deep learning algorithm using U-Net architecture to identify kidneys on T2-weighted MRI and quantify non-neoplastic renal parenchymal volume (RV). The cohort was divided into a 74/13/13% split of training/validation/test subsets. Model development was carried out using a 5-fold cross validation technique. An ensemble of the three best performing models on the training and validation subsets was implemented to generate a more robust prediction segmentation. The associations between height-normalized pre-operative RV and PORF were assessed using generalized linear mixed effect models, adjusted for known clinical factors associated with PORF (age, diabetes, preoperative eGFR, proteinuria, tumor size, time from surgery).
Results: MRI images from from 330 patients, including 208 PN and 122 RN were used to develop a deep learning algorithm with a final Dice coefficient of 0.93 and Jaccard index of 0.87 compared to manual segmentations (Figure 1). On unadjusted analyses, RV was associated with PORF following PN and RN (p < 0.001 and p=0.008, respectively). When added to existing multivariable models to predict PORF, the associations between RV and PORF remained statistically significant (p < 0.001 and p=0.05, respectively).
Conclusions: Pre-operative non-neoplastic renal volume is associated with long-term renal function following PN and RN, even after adjusting for a previously validated clinical prediction model. We developed a deep learning tool to facilitate automated RV assessment, which may promote integration of RV measurement into clinical practice.
Source of Funding: None

.jpg)
.jpg)