Back
Poster, Podium & Video Sessions
Moderated Poster
MP33: Uroradiology I
MP33-18: Association of Patient and Imaging-Related Factors with False Negative Fusion Biopsies of PI-RADS 4 and 5 Lesions on MRI
Saturday, May 14, 2022
4:30 PM – 5:45 PM
Location: Room 228
Miyad Movassaghi*, Firas Ahmed, Hanisha Patel, Lyndon Luk, New York, NY, Elias Hyams, Providence, RI, Sven Wenske, Hiram Shaish, New York, NY

Miyad Movassaghi, MD, MS
Columbia University
Poster Presenter(s)
Introduction: In patients who end up having a negative MRI/TRUS-fusion biopsy (TBx) with positive systematic biopsies in the sextant core corresponding with the targeted area or adjacent sextant cores notable for clinically significant prostate cancer (csPCa), identifying the source of error to rule out missed disease is critical. The goal of this study was to investigate whether specific imaging and patient-related factors, including discrepant US and MRI prostate segmentation volumes, are associated with a false negative (FN) TBx of PI-RADS 4/5 lesions.
Methods: This was a retrospective study of patients with PI-RADS 4 or 5 peripheral zone (PZ) lesions on MRIs performed between 11/2015-12/2020 and subsequent TBx. Biopsied lesions were separated into true positive (TP), false positive (FP) and false negative (FN) using a combination of systematic and fusion biopsy and grade group 2 or higher as the reference standard. FP cases were excluded. FN TBx was defined as negative targeted fusion cores with adjacent positive systematic cores. The impact of patient and imaging-specific factors on the probability of a FN fusion biopsy were tested using logistic regression.
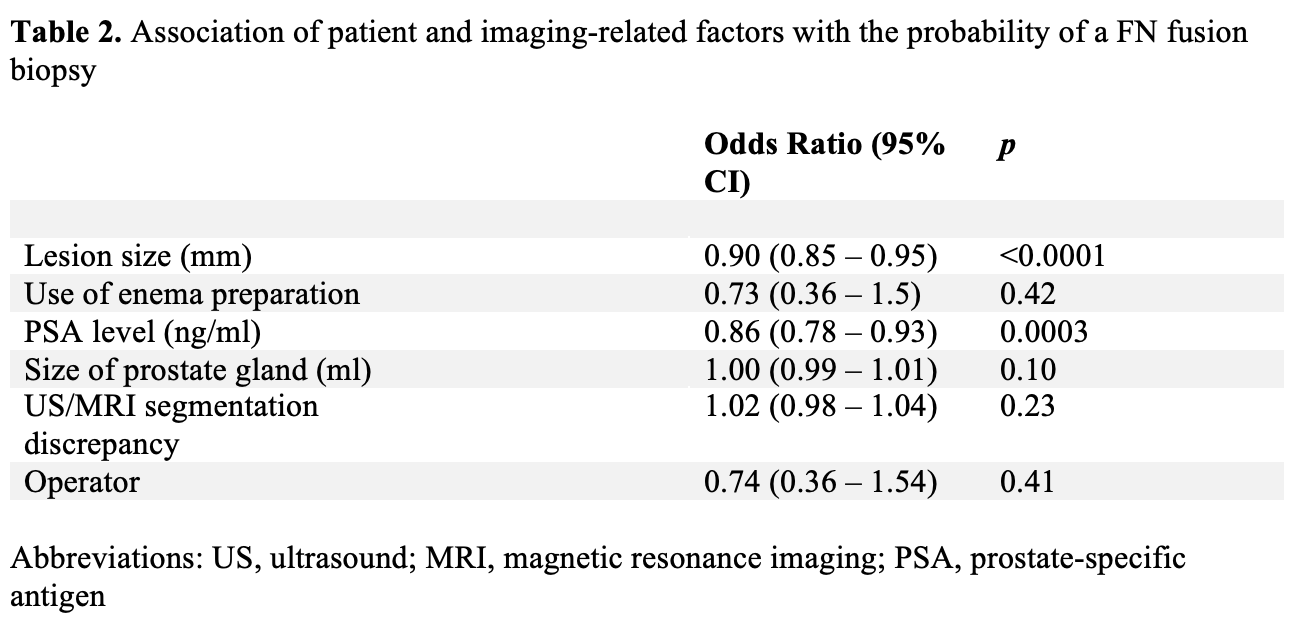
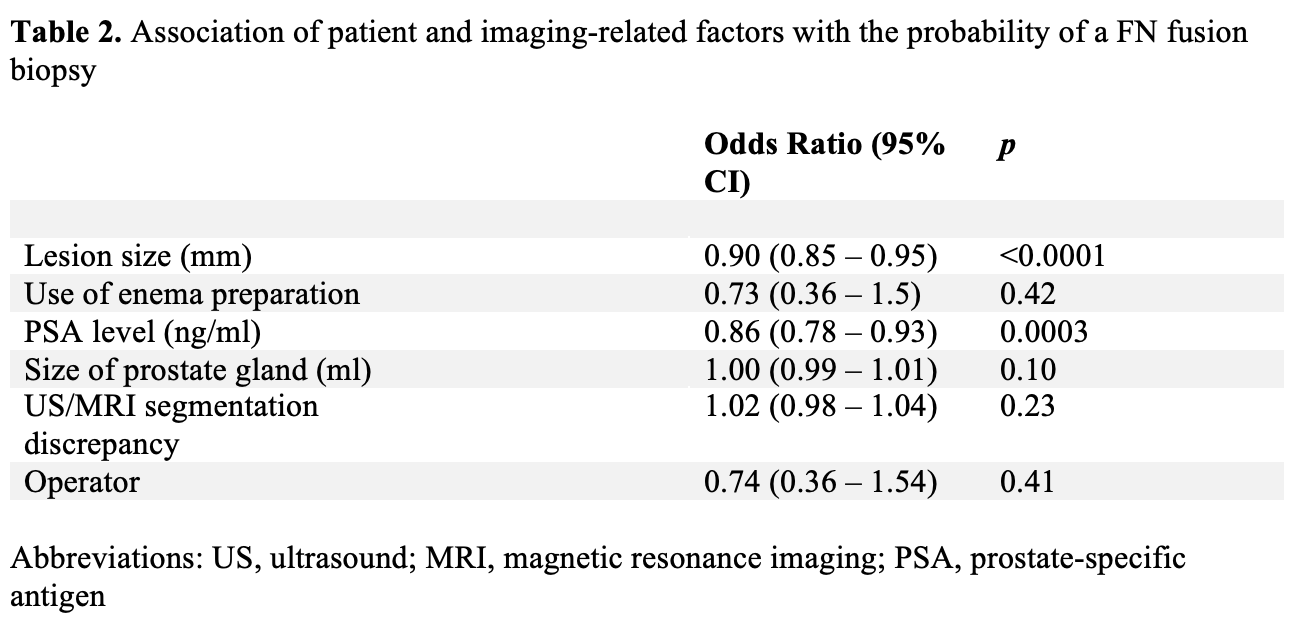
Results: 530 consecutive patients with 685 PI-RADS 4 or 5 PZ lesions on MRI and subsequent TBx were retrospectively collected. 361 lesions in 304 patients (median age 69 years, IQR 63-75, median PSA 6.5 ng/ml, IQR 4.7-9.3), including 67 (19%) FN and 294 TP (81%) were included. There was a significant inverse association between lesion size and probability of FN biopsy (odds ratio (OR): 0.90, 95% CI: 0.85 - 0.95, p-value: <0.0001). Similarly, PSA level was inversely associated with a FN biopsy (OR: 0.86, 95%CI: 0.77 - 0.93, p-value: 0.0003). The probability of a FN TBx was not associated with use of an enema prep before MRI, size of prostate gland, discrepancy between US and MRI segmented prostate volume or the operator (p-value>0.05).
Conclusions: Among men undergoing TBx, lower PSA values and smaller PI-RADS 4/5 lesions are associated with FN fusion biopsies. Discrepant US and MRI prostate segmentation volumes derived as part of fusion biopsy were not associated with a FN biopsy. Our data support a biopsy strategy for select men, especially those with smaller PI-RADS 4/5 lesions, that includes a concomitant SBx at the time of TBx.
Source of Funding: None
Methods: This was a retrospective study of patients with PI-RADS 4 or 5 peripheral zone (PZ) lesions on MRIs performed between 11/2015-12/2020 and subsequent TBx. Biopsied lesions were separated into true positive (TP), false positive (FP) and false negative (FN) using a combination of systematic and fusion biopsy and grade group 2 or higher as the reference standard. FP cases were excluded. FN TBx was defined as negative targeted fusion cores with adjacent positive systematic cores. The impact of patient and imaging-specific factors on the probability of a FN fusion biopsy were tested using logistic regression.
Results: 530 consecutive patients with 685 PI-RADS 4 or 5 PZ lesions on MRI and subsequent TBx were retrospectively collected. 361 lesions in 304 patients (median age 69 years, IQR 63-75, median PSA 6.5 ng/ml, IQR 4.7-9.3), including 67 (19%) FN and 294 TP (81%) were included. There was a significant inverse association between lesion size and probability of FN biopsy (odds ratio (OR): 0.90, 95% CI: 0.85 - 0.95, p-value: <0.0001). Similarly, PSA level was inversely associated with a FN biopsy (OR: 0.86, 95%CI: 0.77 - 0.93, p-value: 0.0003). The probability of a FN TBx was not associated with use of an enema prep before MRI, size of prostate gland, discrepancy between US and MRI segmented prostate volume or the operator (p-value>0.05).
Conclusions: Among men undergoing TBx, lower PSA values and smaller PI-RADS 4/5 lesions are associated with FN fusion biopsies. Discrepant US and MRI prostate segmentation volumes derived as part of fusion biopsy were not associated with a FN biopsy. Our data support a biopsy strategy for select men, especially those with smaller PI-RADS 4/5 lesions, that includes a concomitant SBx at the time of TBx.
Source of Funding: None

.jpg)
.jpg)