Back
Poster, Podium & Video Sessions
Moderated Poster
MP34: Infertility: Therapy
MP34-06: Predictors of success after bilateral vasoepididymostomy performed during vasectomy reversal: a multi-institutional analysis
Saturday, May 14, 2022
4:30 PM – 5:45 PM
Location: Room 225
Joshua White, Jesse Ory, Halifax, Canada, Sirpi Nackeeran*, Miami, FL, Udi Blankstein, Hamilton, Canada, Justin Dubin, Chicago, MI, Aditya Sathe, Memphis, TN, Ethan Grober, Toronto, Canada, Sheldon Marks, Tuscon, AZ, Ranjith Ramasamy, Miami, FL
- SN
Sirpi Nackeeran, BA
University of Miami, Miller School of Medicine
Poster Presenter(s)
Introduction: Vasectomy reversal (VR) is an excellent option for paternity in men who desire to expand their family following vasectomy. Traditional VR via vasovasostomy has a success rate upwards of 90%, but is sometimes not possible, and a vasoepididymostomy (VE) must be performed instead. There is a paucity of literature evaluating predictors of success following VE. Our objective was to use a multi-institutional database to determine factors influencing success after bilateral VE.
Methods: A multi-institutional, prospectively maintained database with data from the USA and Canada was used to identify men who underwent bilateral VE at time of VR. Data were collected from 2008 to 2020. Pre, intra and postoperative clinical and surgical data were collected. Possible predictors of success included time since vasectomy, patient age, and intraoperative epididymal fluid/sperm characteristics. Success was defined as motile sperm in any post-operative semen analyses. VE in both centers was performed using two 10-0 sutures in an intussusception technique. Multivariable logistic regression was used to identify predictors of success.
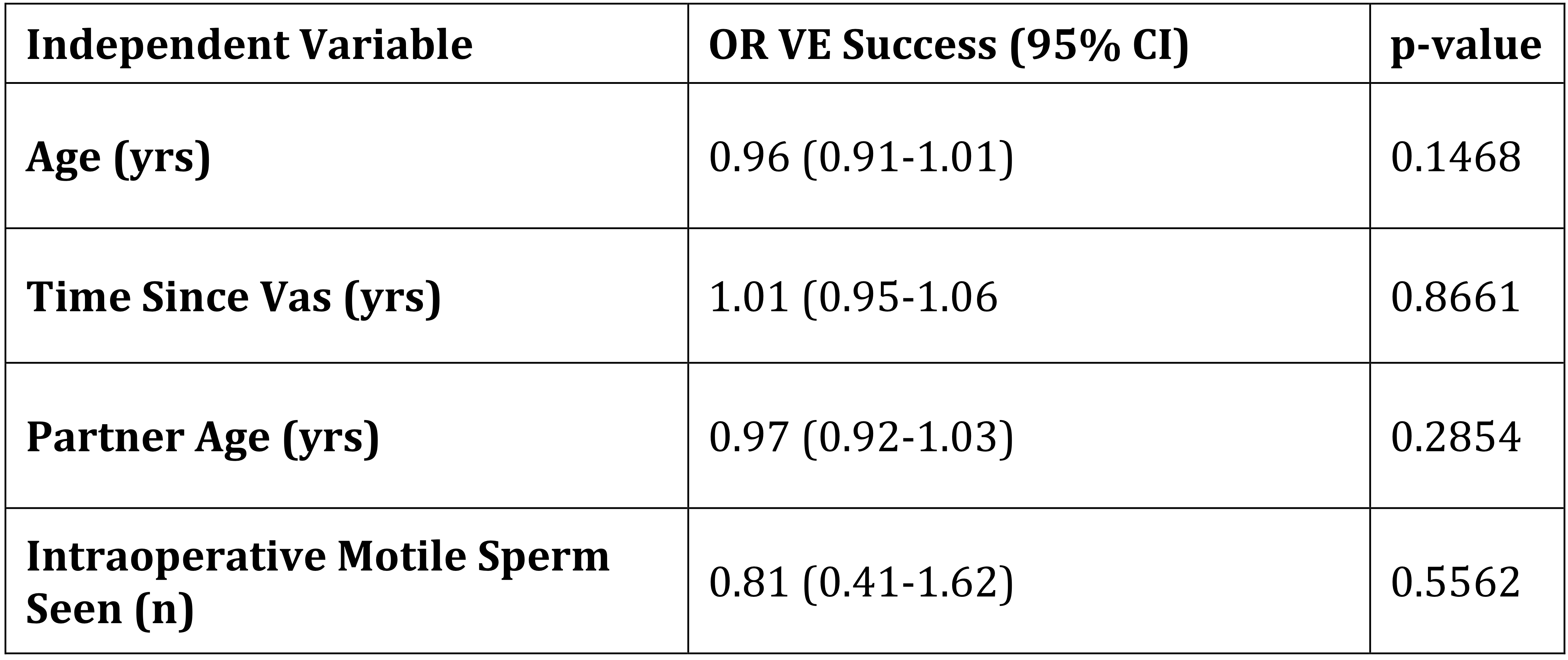
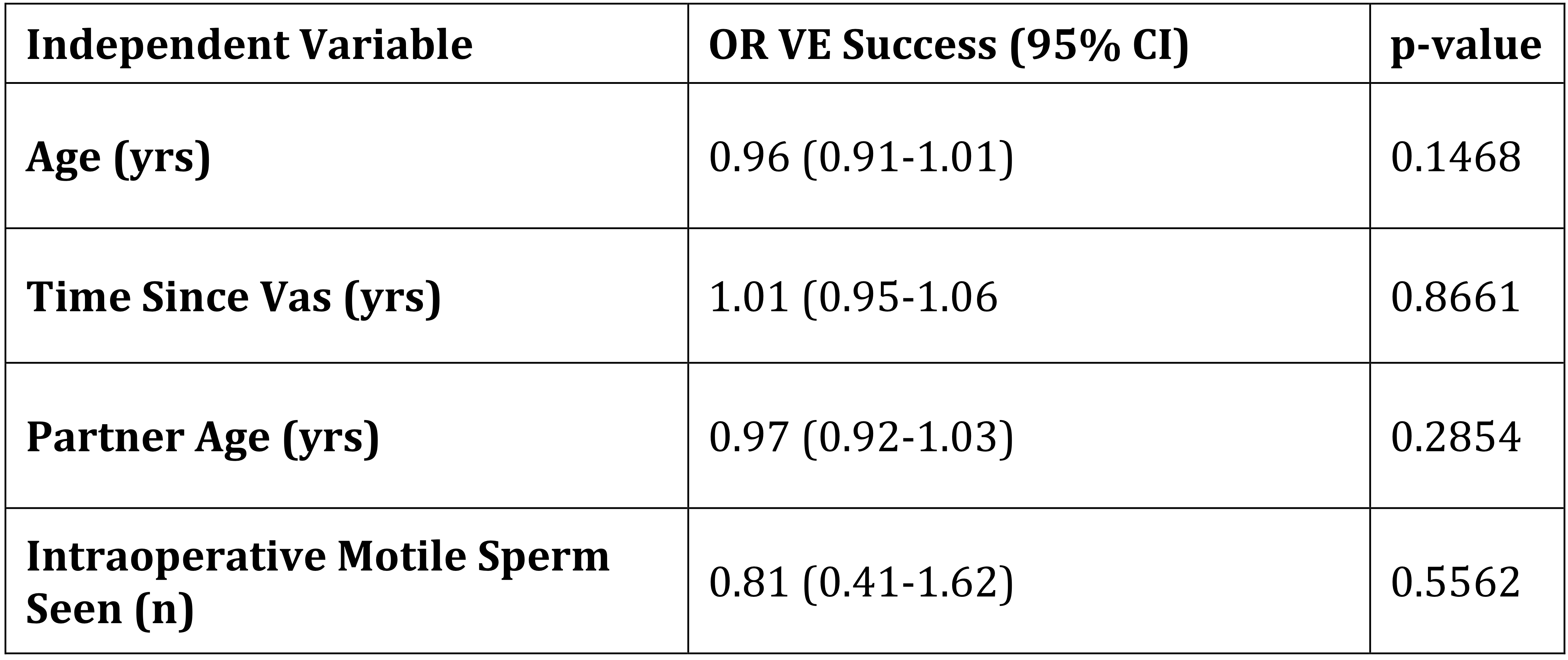
Results: A total of 191 men were included in the analysis. Average age was 45.8 years. Median time elapsed between vasectomy and VE was 14 years [IQR 10-18]. The longest time elapsed for a successful VE was 34 years. Overall success rate was 50%. 77.0% of all men had motile sperm in epidydimal fluid intraoperatively, at time of VE. On multiple logistic regression, neither years since vasectomy (OR 1.01, CI 0.95-1.06), age (OR 0.96, 0.91-1.01), intraoperative presence of motile sperm (OR 0.81, CI 0.41-1.62) nor any epidydimal fluid characteristics (clear vs. cloudy, copious vs. scant) predicted success.
Conclusions: Bilateral VE at time of vasectomy reversal is successful in 50% of cases in a multi-institutional, North American cohort. Microsurgeons can be reassured that neither time elapsed nor epididymal fluid characteristics negatively impact success rates. This knowledge can allow surgeons to avoid a laborious search during VE for the ideal tubule and multiple epididymal punctures. Features associated with vasovasostomy failure (time since vasectomy, intraoperative semen quality) do not apply to VE success.
Source of Funding: This work was supported by the National Institutes of Health Grant R01 DK130991 and Clinician Scientist Development Grant from the American Cancer Society to RR
Methods: A multi-institutional, prospectively maintained database with data from the USA and Canada was used to identify men who underwent bilateral VE at time of VR. Data were collected from 2008 to 2020. Pre, intra and postoperative clinical and surgical data were collected. Possible predictors of success included time since vasectomy, patient age, and intraoperative epididymal fluid/sperm characteristics. Success was defined as motile sperm in any post-operative semen analyses. VE in both centers was performed using two 10-0 sutures in an intussusception technique. Multivariable logistic regression was used to identify predictors of success.
Results: A total of 191 men were included in the analysis. Average age was 45.8 years. Median time elapsed between vasectomy and VE was 14 years [IQR 10-18]. The longest time elapsed for a successful VE was 34 years. Overall success rate was 50%. 77.0% of all men had motile sperm in epidydimal fluid intraoperatively, at time of VE. On multiple logistic regression, neither years since vasectomy (OR 1.01, CI 0.95-1.06), age (OR 0.96, 0.91-1.01), intraoperative presence of motile sperm (OR 0.81, CI 0.41-1.62) nor any epidydimal fluid characteristics (clear vs. cloudy, copious vs. scant) predicted success.
Conclusions: Bilateral VE at time of vasectomy reversal is successful in 50% of cases in a multi-institutional, North American cohort. Microsurgeons can be reassured that neither time elapsed nor epididymal fluid characteristics negatively impact success rates. This knowledge can allow surgeons to avoid a laborious search during VE for the ideal tubule and multiple epididymal punctures. Features associated with vasovasostomy failure (time since vasectomy, intraoperative semen quality) do not apply to VE success.
Source of Funding: This work was supported by the National Institutes of Health Grant R01 DK130991 and Clinician Scientist Development Grant from the American Cancer Society to RR

.jpg)
.jpg)