Back
Poster, Podium & Video Sessions
Moderated Poster
MP34: Infertility: Therapy
MP34-14: Effects of radiation therapy on microsurgical testicular sperm extraction for men with non-obstructive azoospermia
Saturday, May 14, 2022
4:30 PM – 5:45 PM
Location: Room 225
Aaron Brant*, Nahid Punjani, Peter Schlegel, New York, NY

Aaron Brant, MD
New York-Presbyterian/Weill Cornell
Poster Presenter(s)
Introduction: Men who survive cancer as children or young adults may have severe spermatogenic impairment with azoospermia requiring surgical sperm retrieval and assisted reproductive technologies for fertility treatment. We assessed treatment outcomes from a large series of cancer patients with prior radiation therapy.
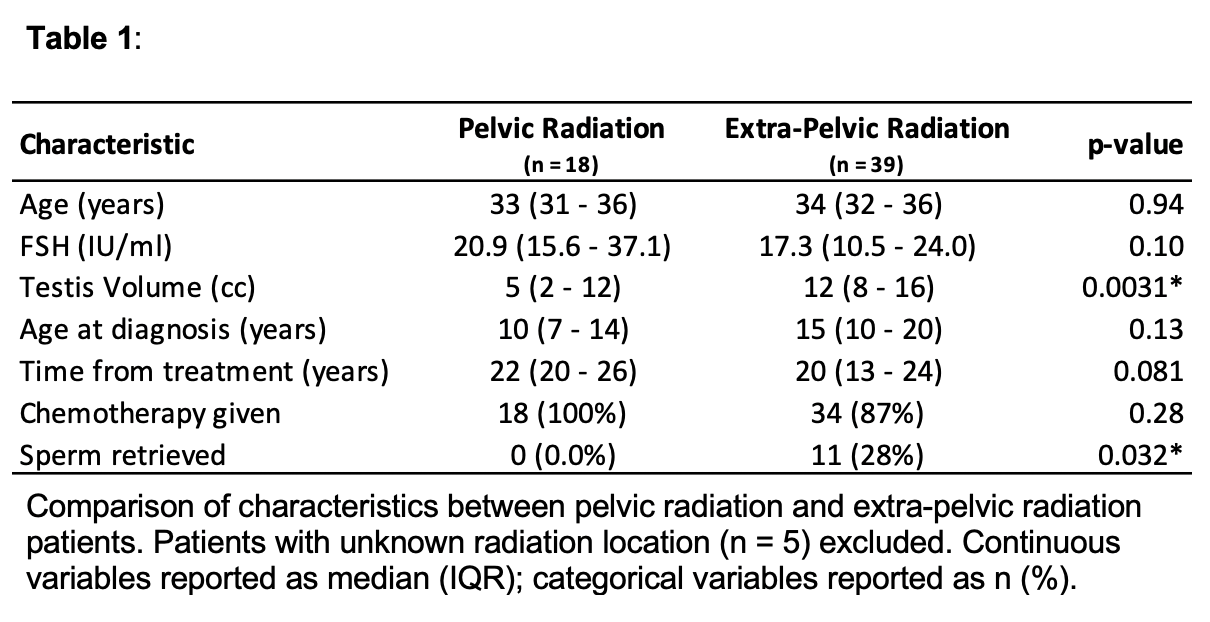
Methods: Men who underwent microsurgical testicular sperm extraction (mTESE) between 1995 and 2020 from a high-volume surgeon at a single institution were reviewed. Men with a diagnosis of non-obstructive azoospermia (NOA) and history of malignancy treated by radiation therapy were included. Men with history of prior sperm retrieval attempts at other centers were excluded. Reported outcomes included sperm retrieval, pregnancy, and testicular histopathology. Comparisons were made between patients with pelvic and extra-pelvic radiation therapy.
Results: A total of 62 men with NOA and history of radiation who underwent initial mTESE were identified. The median male age was 34 years (IQR 30-37), and median partner age was 31 years (IQR 28-34). Median testis volume was 11 cc (IQR 5-14), and median FSH level was 18.3 IU/ml (IQR 13.0-25.6). A total of 57 men (92%) received chemotherapy. The most common testicular histopathology was Sertoli cell only (SCO), observed in 49 of 55 (89%) biopsies. Sperm was retrieved in 12 men on initial mTESE (19%), and pregnancy with retrieved sperm occurred in 9 of these couples (75%). None of the 18 patients who received radiation to the pelvis had successful sperm retrieval, compared to 28% of patients with extra-pelvic radiation (p=0.032).
Conclusions: Sperm retrieval is negligible in NOA men with a history of malignancy and concomitant pelvic radiation therapy. These men should be counseled appropriately on the poor prognosis for sperm retrieval.
Source of Funding: Nahid Punjani was supported by the Theresa and Wallace Fund of the New York Community Trust
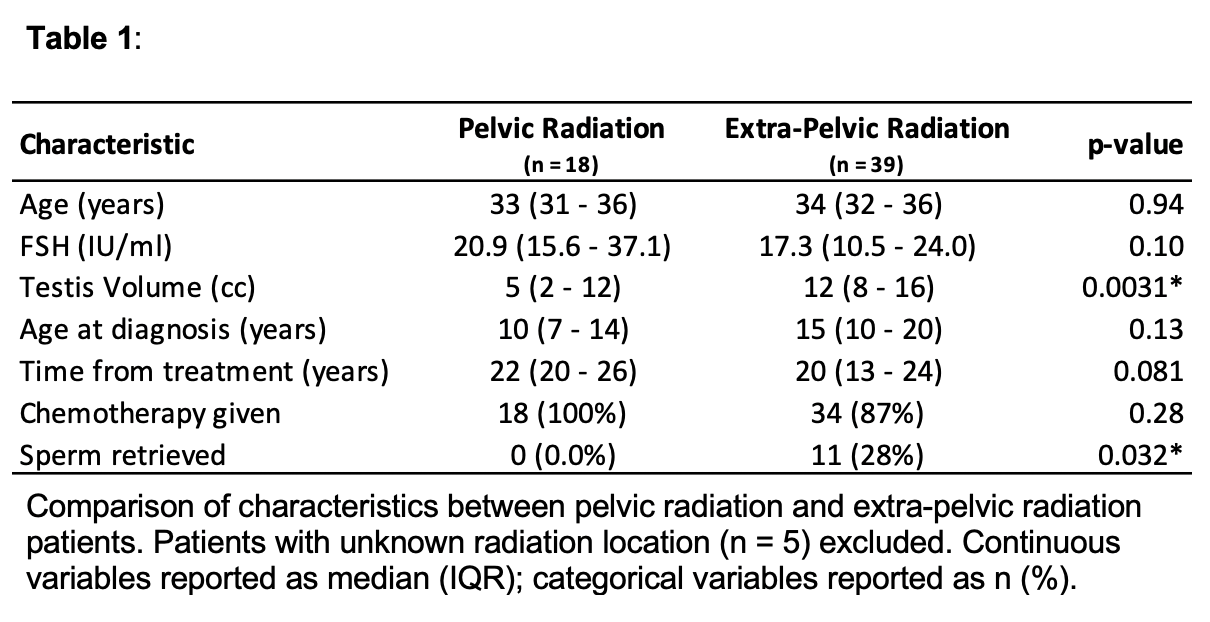
Methods: Men who underwent microsurgical testicular sperm extraction (mTESE) between 1995 and 2020 from a high-volume surgeon at a single institution were reviewed. Men with a diagnosis of non-obstructive azoospermia (NOA) and history of malignancy treated by radiation therapy were included. Men with history of prior sperm retrieval attempts at other centers were excluded. Reported outcomes included sperm retrieval, pregnancy, and testicular histopathology. Comparisons were made between patients with pelvic and extra-pelvic radiation therapy.
Results: A total of 62 men with NOA and history of radiation who underwent initial mTESE were identified. The median male age was 34 years (IQR 30-37), and median partner age was 31 years (IQR 28-34). Median testis volume was 11 cc (IQR 5-14), and median FSH level was 18.3 IU/ml (IQR 13.0-25.6). A total of 57 men (92%) received chemotherapy. The most common testicular histopathology was Sertoli cell only (SCO), observed in 49 of 55 (89%) biopsies. Sperm was retrieved in 12 men on initial mTESE (19%), and pregnancy with retrieved sperm occurred in 9 of these couples (75%). None of the 18 patients who received radiation to the pelvis had successful sperm retrieval, compared to 28% of patients with extra-pelvic radiation (p=0.032).
Conclusions: Sperm retrieval is negligible in NOA men with a history of malignancy and concomitant pelvic radiation therapy. These men should be counseled appropriately on the poor prognosis for sperm retrieval.
Source of Funding: Nahid Punjani was supported by the Theresa and Wallace Fund of the New York Community Trust

.jpg)
.jpg)