Back
Poster, Podium & Video Sessions
Moderated Poster
MP36: Renal Transplantation & Vascular Surgery
MP36-15: Robotic Single-Port versus Laparoscopic Donor Nephrectomy: An Institutional Analysis
Sunday, May 15, 2022
7:00 AM – 8:15 AM
Location: Room 228
Chih Peng Chin*, Evan Garden, Micah Levy, Krishna Ravivarapu, Osama Al-Alao, Joseph Sewell Araya, Sander Florman, Antonios Arvelakis, Daniel Herron, Edward Chin, Michael Palese, New York, NY
- CC
Poster Presenter(s)
Introduction: Single-port robotic donor nephrectomy (SP RDN) with the da Vinci SP Surgical System is a novel minimally invasive surgical option for kidney donors that can offer comparable surgical outcomes to laparoscopic donor nephrectomy (LDN). Here, we evaluate the largest case series to date comparing SP RDN to LDN.
Methods: Patient demographics, operative details, and postoperative outcomes were retrospectively collected from patients undergoing SP RDN and LDN at a single academic hospital from 9/2020 to 8/2021. Outcomes included pain scores (scale of 1-10), inpatient opioid use (converted to oral morphine milligram equivalent [MME]), renal function, and Clavien-Dindo complications.
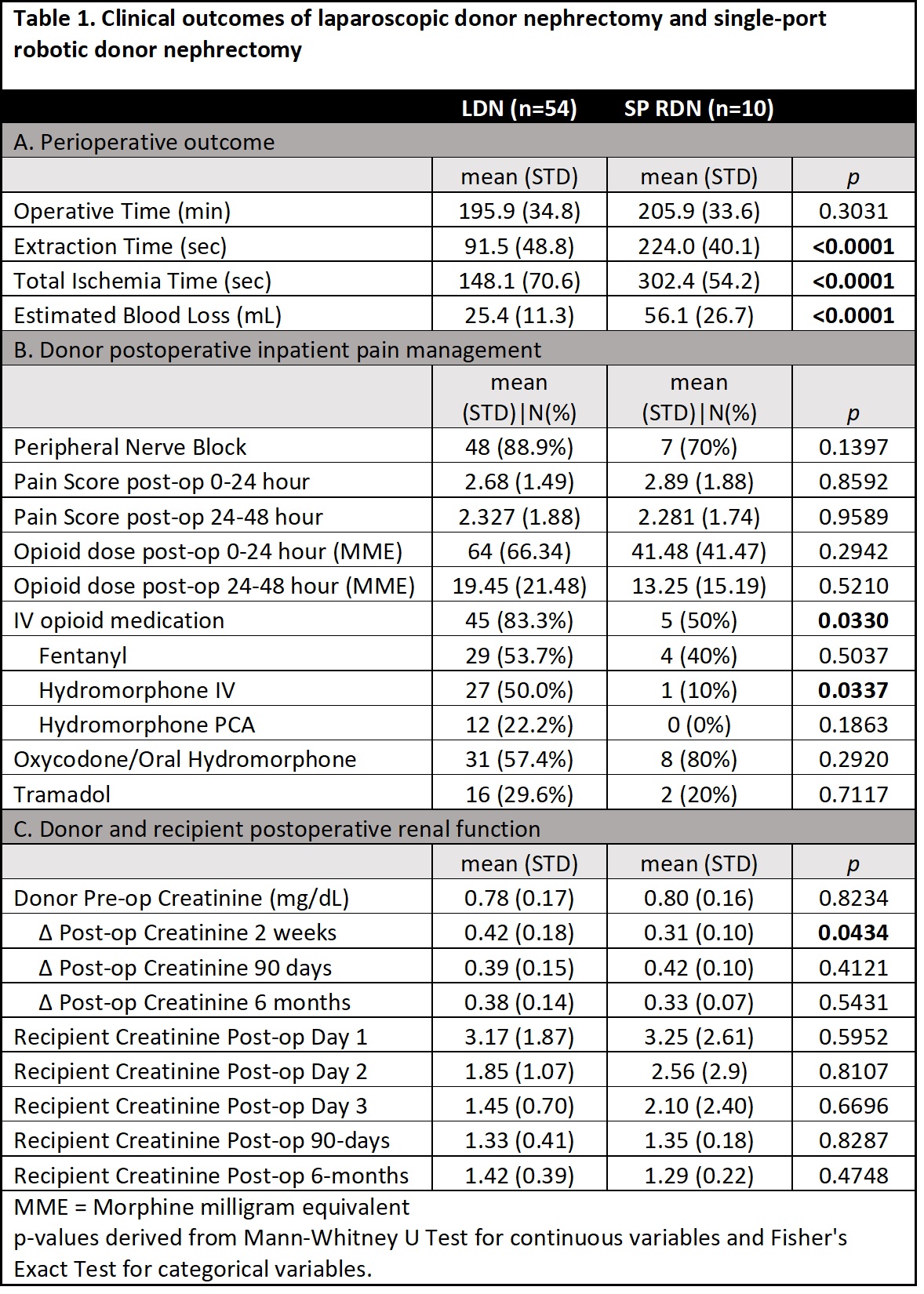
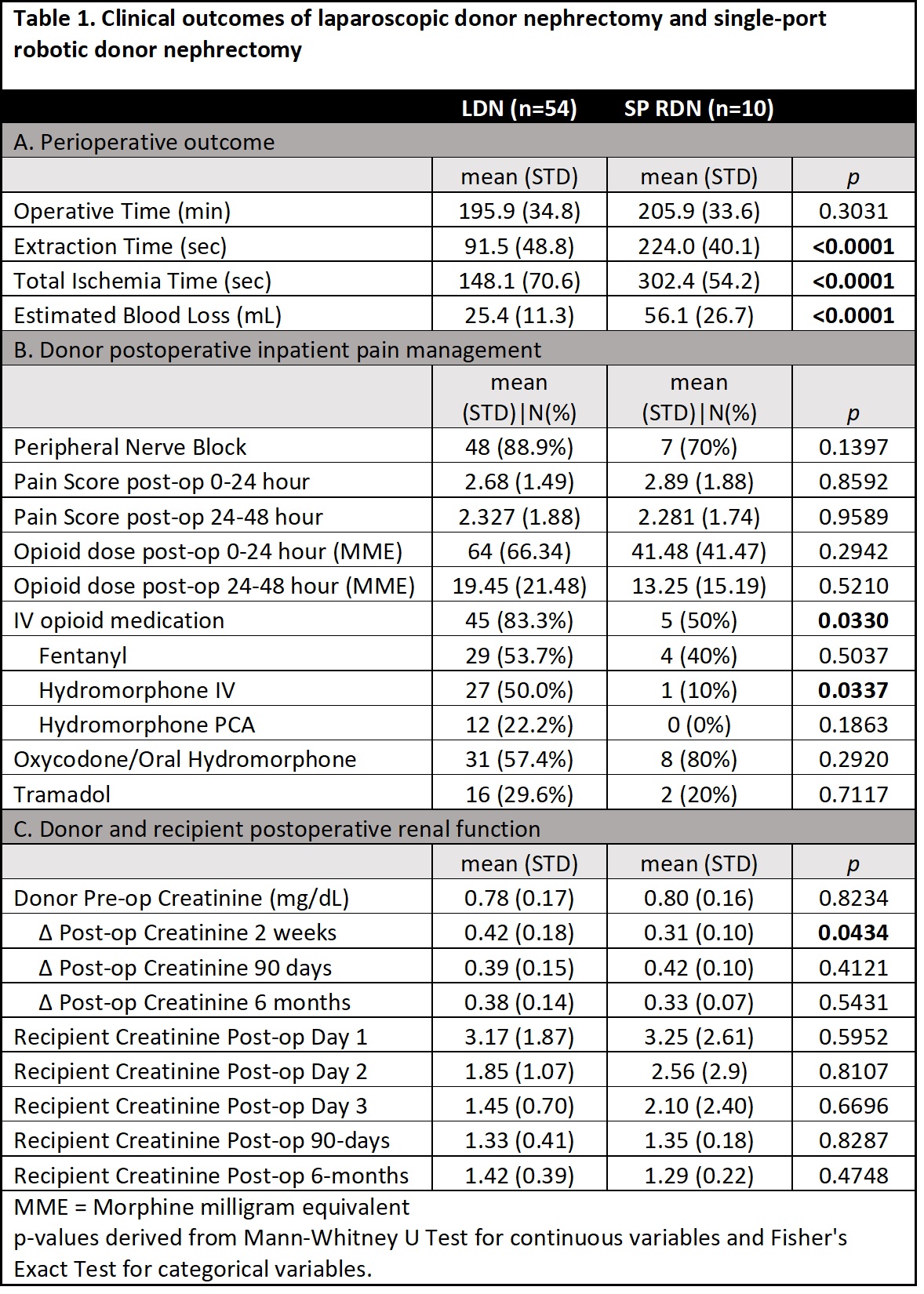
Results: 54 and 10 patients underwent LDN and SP RDN, respectively. 41 (76%) LDN and 8 (80%) SP RDN involved the left kidney. There were no differences between groups in donor age, BMI, ASA status, or preoperative creatinine (all p >0.05). SP RDN and LDN had similar operative times (206 min vs 196 min, p=0.30); however, extraction (3.7 min vs 1.5 min, p<0.01) and warm ischemia times (5.0 min vs 2.5 min, p<0.01) were longer for SP RDN (Table 1a). SP RDN had greater estimated blood loss and greater decrease in hematocrit (SP RDN -9.0% vs LDN -7.1%, p<0.01) in the immediate postoperative period. Postoperative patient pain scores and inpatient MME requirements at 24 and 48 hours were similar (Table 1b). Significantly fewer SP RDN patients required postoperative intravenous opioids than LDN patients (SP RDN 50.0% vs LDN 83.3%, p=0.03). 35.2% of LDN and 50% of SP RDN patients were discharged at postoperative day 2 or later due to medical reasons (p=0.48). No difference was observed in recipient creatinine at 1-3 days, 90 days, and 6 months. Changes in donor creatinine at 90 days and 6 months, rates of donor postoperative complication, ER visits, and readmissions were similar between groups (Table 1c). 3 LDN (5.6%) and 2 (10%) SP RDN patients had Clavien-Dindo II complications; no donor from either group had a Clavien-Dindo >III complication.
Conclusions: SP RDN is a safe alternative to LDN, offering similar donor postoperative clinical outcomes and recipient renal function up to 6 months. Further studies are needed to assess the long-term outcomes, postoperative opioid usage, and potential for improved cosmesis of SP RDN compared to other kidney donor surgical modalities.
Source of Funding: None
Methods: Patient demographics, operative details, and postoperative outcomes were retrospectively collected from patients undergoing SP RDN and LDN at a single academic hospital from 9/2020 to 8/2021. Outcomes included pain scores (scale of 1-10), inpatient opioid use (converted to oral morphine milligram equivalent [MME]), renal function, and Clavien-Dindo complications.
Results: 54 and 10 patients underwent LDN and SP RDN, respectively. 41 (76%) LDN and 8 (80%) SP RDN involved the left kidney. There were no differences between groups in donor age, BMI, ASA status, or preoperative creatinine (all p >0.05). SP RDN and LDN had similar operative times (206 min vs 196 min, p=0.30); however, extraction (3.7 min vs 1.5 min, p<0.01) and warm ischemia times (5.0 min vs 2.5 min, p<0.01) were longer for SP RDN (Table 1a). SP RDN had greater estimated blood loss and greater decrease in hematocrit (SP RDN -9.0% vs LDN -7.1%, p<0.01) in the immediate postoperative period. Postoperative patient pain scores and inpatient MME requirements at 24 and 48 hours were similar (Table 1b). Significantly fewer SP RDN patients required postoperative intravenous opioids than LDN patients (SP RDN 50.0% vs LDN 83.3%, p=0.03). 35.2% of LDN and 50% of SP RDN patients were discharged at postoperative day 2 or later due to medical reasons (p=0.48). No difference was observed in recipient creatinine at 1-3 days, 90 days, and 6 months. Changes in donor creatinine at 90 days and 6 months, rates of donor postoperative complication, ER visits, and readmissions were similar between groups (Table 1c). 3 LDN (5.6%) and 2 (10%) SP RDN patients had Clavien-Dindo II complications; no donor from either group had a Clavien-Dindo >III complication.
Conclusions: SP RDN is a safe alternative to LDN, offering similar donor postoperative clinical outcomes and recipient renal function up to 6 months. Further studies are needed to assess the long-term outcomes, postoperative opioid usage, and potential for improved cosmesis of SP RDN compared to other kidney donor surgical modalities.
Source of Funding: None

.jpg)
.jpg)