Back
Poster, Podium & Video Sessions
Moderated Poster
MP37: Infections/Inflammation/Cystic Disease of the Genitourinary Tract: Prostate & Genitalia
MP37-11: Whole Exome Sequencing Identifies a Rare Mutation in NACAD as a Possible Cause of COVID Orchitis in Brothers
Sunday, May 15, 2022
7:00 AM – 8:15 AM
Location: Room 225
Rohit Reddy*, Efimenko Iakov, Kajal Khodamoradi, Willy Chertman, Himanshu Arora, Parris Diaz, Ranjith Ramasamy, Miami, FL

Rohit Reddy, MD, BA
Temple University Hospital
Poster Presenter(s)
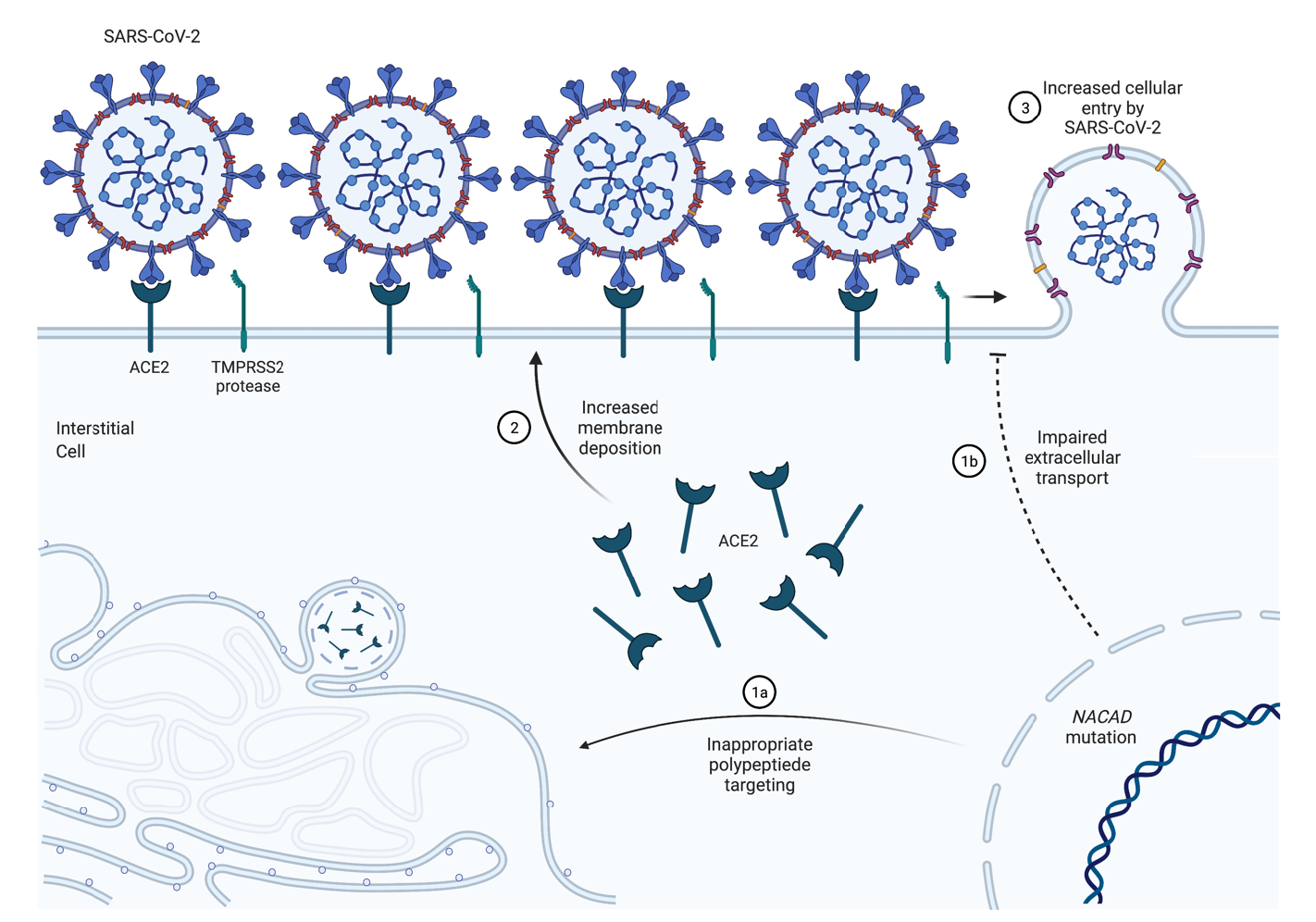
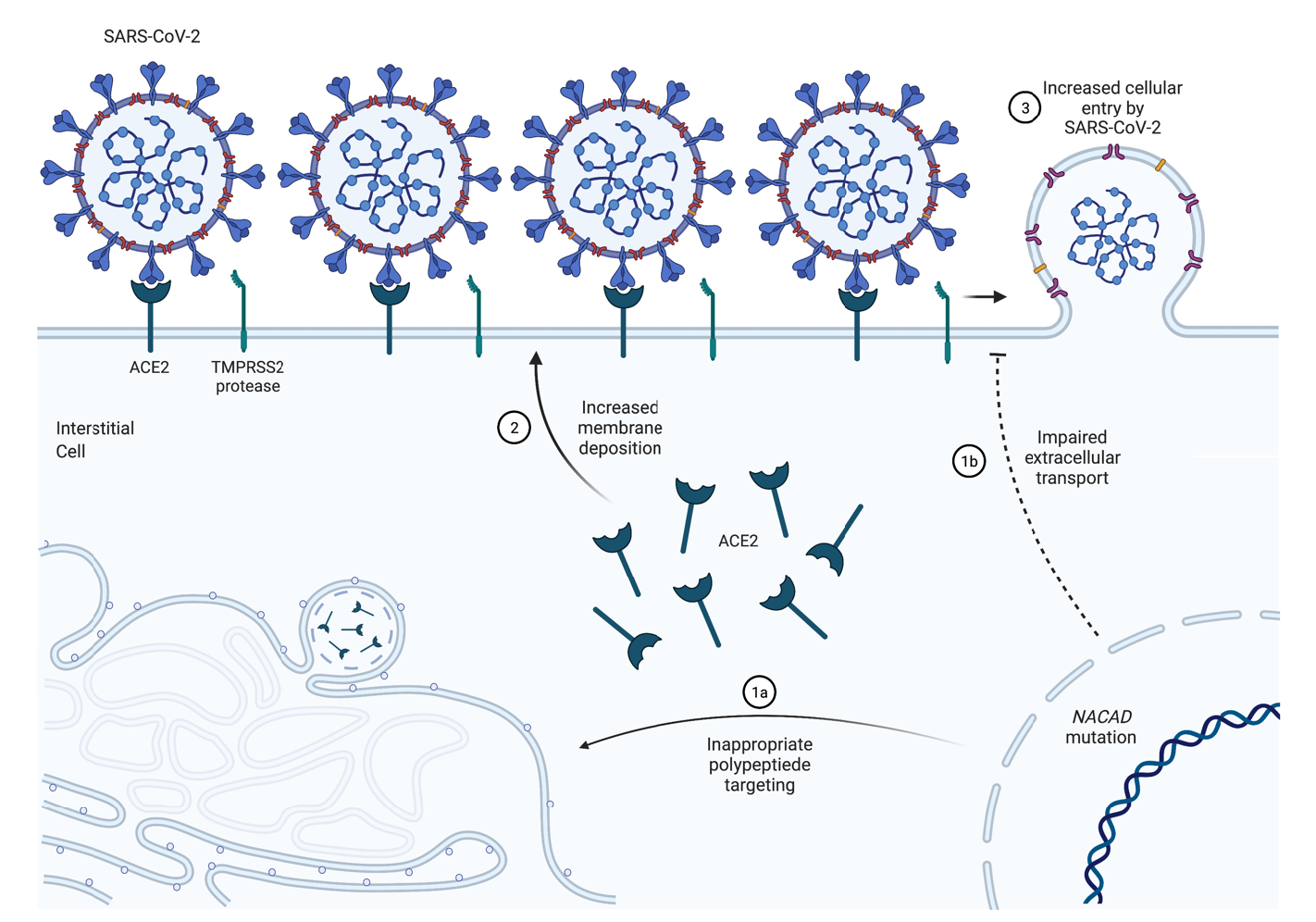
Introduction: SARS-CoV-2 orchitis (testicular pain) is reported in 10-15% of men with long COVID. Our goal was to identify genetic variants associated with COVID orchitis in a group of patients, aided by whole-exome sequencing and protein phenotyping of affected patients.
Methods: We identified and examined six COVID-19 patients confirmed with polymerase chain reaction (PCR), including three COVID-19 (+) men without orchitis (controls) and three COVID (+) men with orchitis (bilateral testicular pain for at least 5 days around the time of testing PCR positive). Of note, among the three men with COVID-19 who had orchitis, two of them were siblings. DNA extraction and whole exome sequencing results from samples were prioritized by being shared between the three patients affected with orchitis, absent in controls. Based on WES findings, DuoSet® Human ACE2 reagent kit was used to measure the level of soluble ACE2 in the plasma samples.
Results: A list of 16 variants was generated that found to be shared between the two siblings with COVID orchitis along with the unrelated subject with COVID orchitis, and not present in the two controls. Among the 16 variants, a non-synonymous non-frameshift deletion in NACAD variant on chromosome 7 with a frequency of 3.9% prevalence in ExAC was prioritized based on known involvement in the ACE2 pathway, read depth, and genotype quality. Phenotypically, we found that circulating levels of soluble ACE2 was 3.50 ng/ml among men who had COVID orchitis and lower than men who developed COVID without orchitis (4.30 ng/mL, P < .05).
Conclusions: We observed a rare deletion on NACAD in the 2 brothers and 1 unrelated man who developed COVID orchitis. Interestingly, circulating ACE2 levels were decreased in men with COVID orchitis. NACAD, when involved with cellular ability to shuttle out ACE2, becomes critical for COVID symptomatology. With decreased transcellular and extracellular transport of ACE2 being possible in subjects with the gene mutation, it can be postulated more ACE2 will be found intracellularly leading to increased cellular entry of SARS CoV-2 and possibility of orchitis sequelae. Ultimately, the combination of our genetic analysis and differing ACE2 levels between the groups suggests a possible mechanism for COVID-19 orchitis that warrants further investigation.
Source of Funding: This work was supported by National Institutes of Health Grant R01 DK130991 and Clinician Scientist Development Grant from the American Cancer Society to RR.
Methods: We identified and examined six COVID-19 patients confirmed with polymerase chain reaction (PCR), including three COVID-19 (+) men without orchitis (controls) and three COVID (+) men with orchitis (bilateral testicular pain for at least 5 days around the time of testing PCR positive). Of note, among the three men with COVID-19 who had orchitis, two of them were siblings. DNA extraction and whole exome sequencing results from samples were prioritized by being shared between the three patients affected with orchitis, absent in controls. Based on WES findings, DuoSet® Human ACE2 reagent kit was used to measure the level of soluble ACE2 in the plasma samples.
Results: A list of 16 variants was generated that found to be shared between the two siblings with COVID orchitis along with the unrelated subject with COVID orchitis, and not present in the two controls. Among the 16 variants, a non-synonymous non-frameshift deletion in NACAD variant on chromosome 7 with a frequency of 3.9% prevalence in ExAC was prioritized based on known involvement in the ACE2 pathway, read depth, and genotype quality. Phenotypically, we found that circulating levels of soluble ACE2 was 3.50 ng/ml among men who had COVID orchitis and lower than men who developed COVID without orchitis (4.30 ng/mL, P < .05).
Conclusions: We observed a rare deletion on NACAD in the 2 brothers and 1 unrelated man who developed COVID orchitis. Interestingly, circulating ACE2 levels were decreased in men with COVID orchitis. NACAD, when involved with cellular ability to shuttle out ACE2, becomes critical for COVID symptomatology. With decreased transcellular and extracellular transport of ACE2 being possible in subjects with the gene mutation, it can be postulated more ACE2 will be found intracellularly leading to increased cellular entry of SARS CoV-2 and possibility of orchitis sequelae. Ultimately, the combination of our genetic analysis and differing ACE2 levels between the groups suggests a possible mechanism for COVID-19 orchitis that warrants further investigation.
Source of Funding: This work was supported by National Institutes of Health Grant R01 DK130991 and Clinician Scientist Development Grant from the American Cancer Society to RR.

.jpg)
.jpg)