Back
Poster, Podium & Video Sessions
Moderated Poster
MP39: Health Services Research: Value of Care: Cost and Outcomes Measures
MP39-02: Long Term Cost Comparisons of Radical Cystectomy versus Trimodal Therapy for Muscle-Invasive Bladder Cancer
Sunday, May 15, 2022
8:45 AM – 10:00 AM
Location: Room 228
Vishnukamal Golla*, Durham, NC, Yong Shan, Elias Farran, Courtney Stewart, Kevin Vu, Alexander Yu, Galveston, TX, Ali Raza Khaki, Stanford, CA, Kirk Keegan, Nashville, TN, Ashish Kamat, Houston, TX, Douglas S. Tyler, Galveston, TX, Stephen J. Freedland, Los Angeles, CA, Stephen B. Williams, Galveston, TX
- VG
Vishnukamal Golla, MD, MPH
Duke University
Poster Presenter(s)
Introduction: Earlier studies on the cost of muscle-invasive bladder cancer treatments are limited to short-term periods of cost. Our study objective is to compare the 2- and 5-year costs associated with trimodal therapy (TMT) versus radical cystectomy (RC) benchmarked against costs for patients who received no curative treatment.
Methods: This cohort study used the Surveillance, Epidemiology, and End Results (SEER)-Medicare database. Medicare expenditures were summed from inpatient, outpatient, and physician services within 2 and 5 years of diagnosis to determine total costs Total Medicare costs at 2-and 5-years following TMT versus RC were compared using inverse probability of treatment-weighted (IPTW) propensity score models.
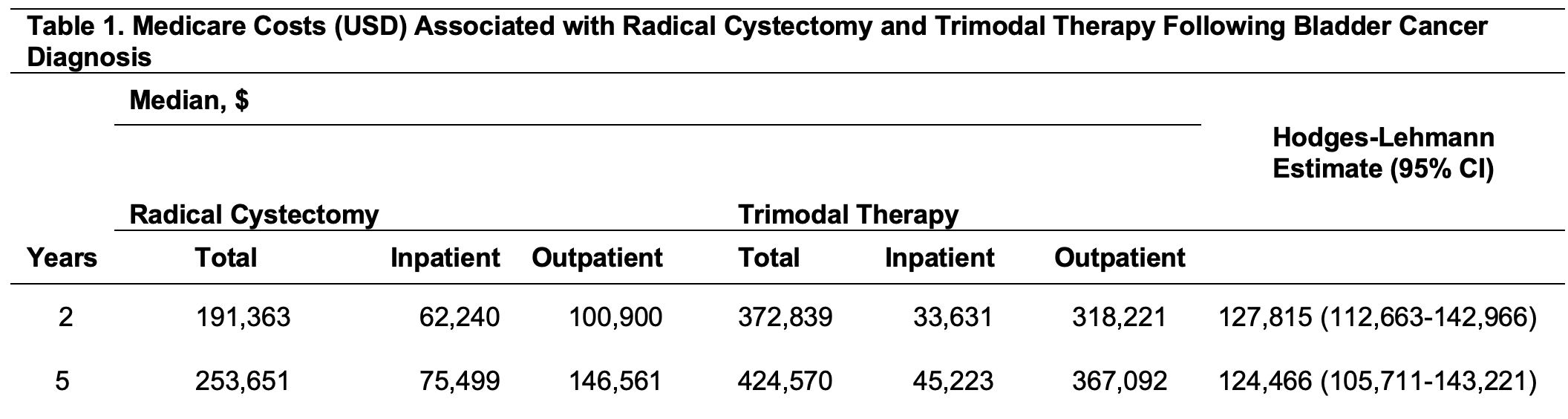
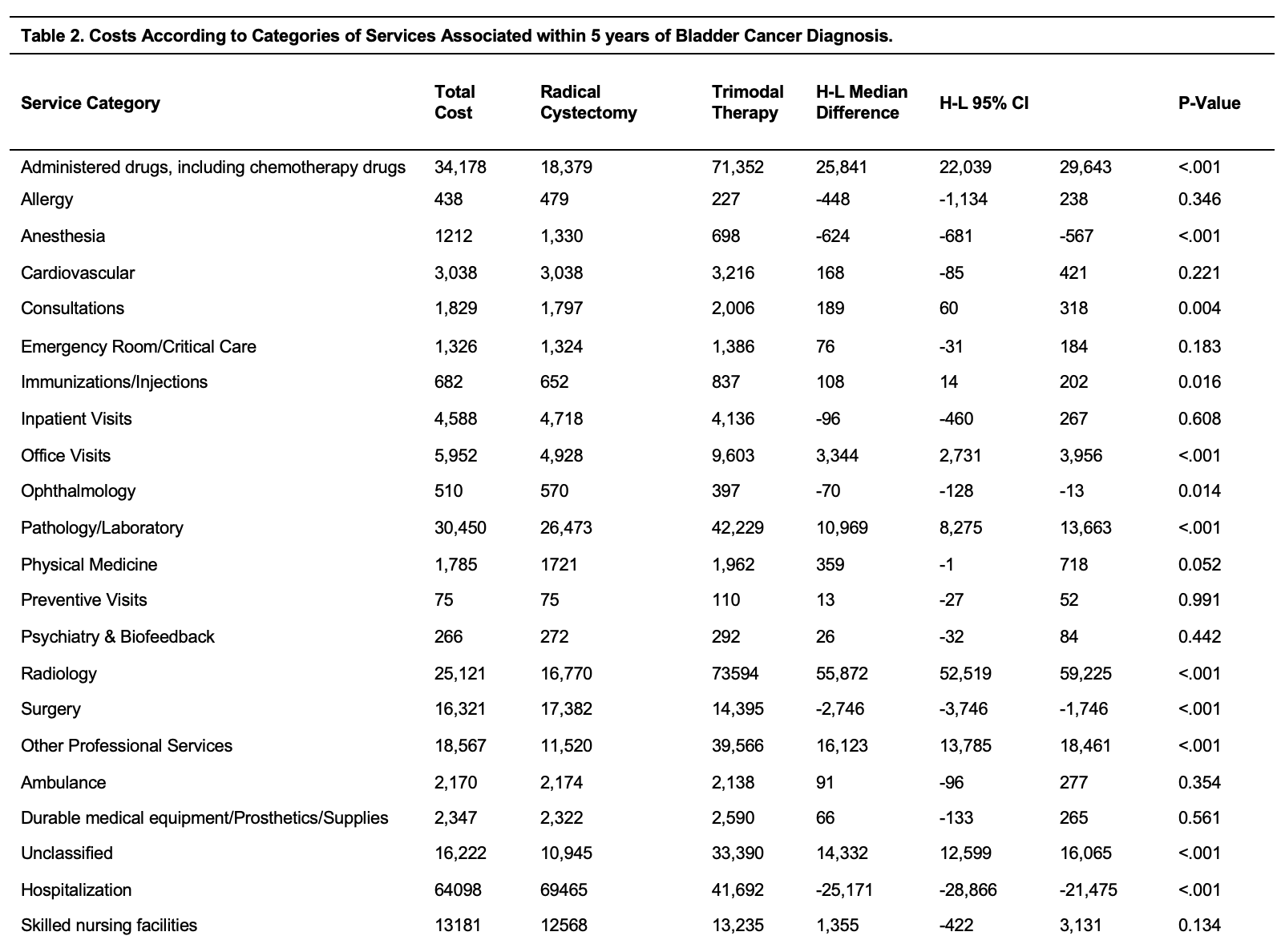
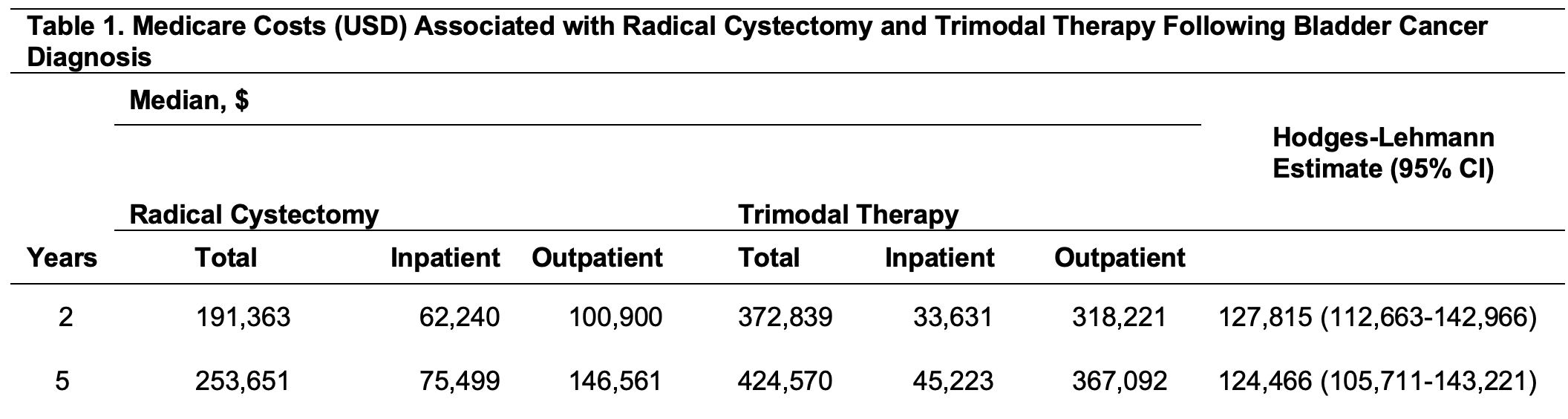
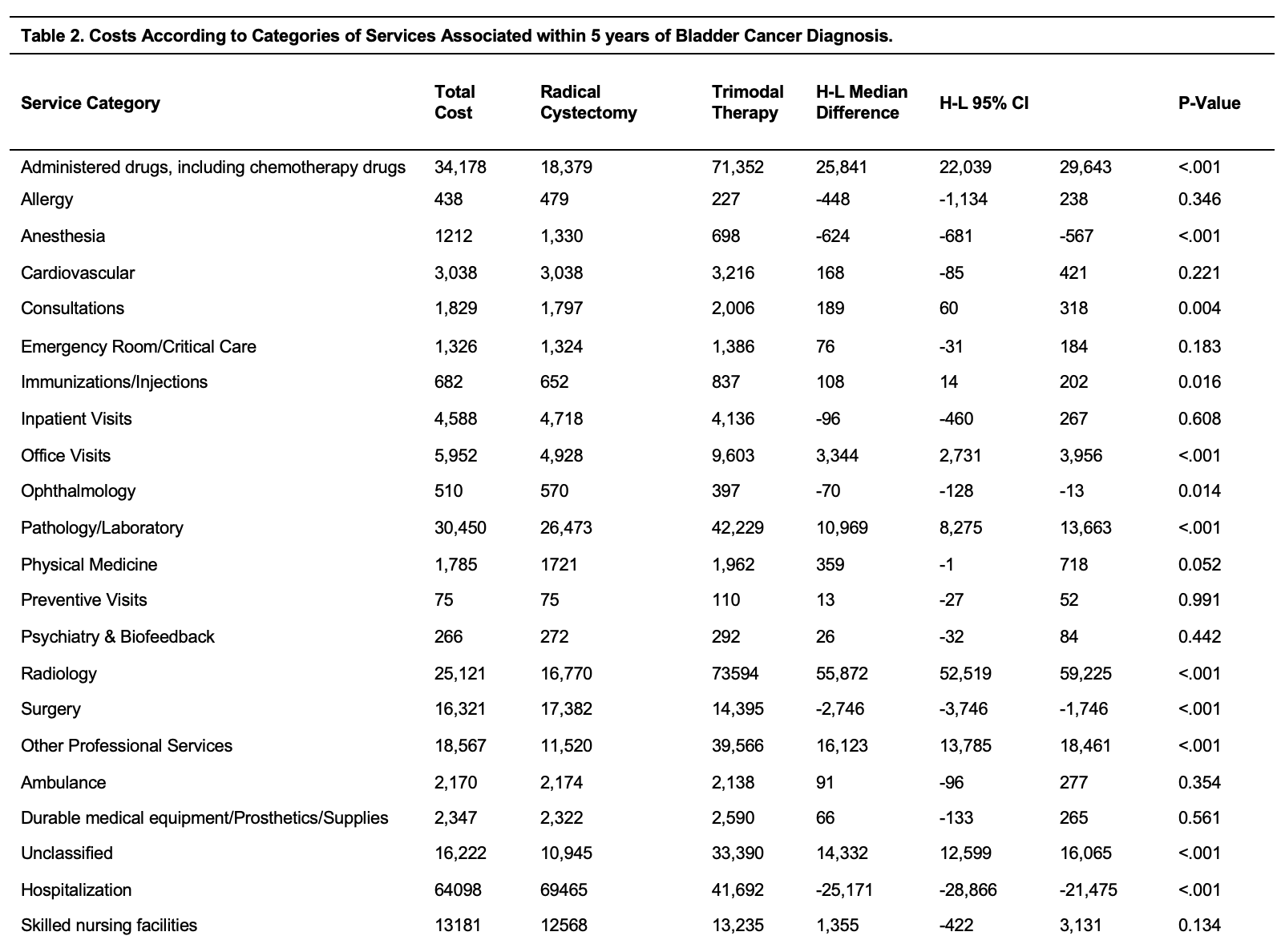
Results: A total of 2,537 patients aged 66-85 years diagnosed with clinical stage T2-4a muscle-invasive bladder cancer from January 1, 2002 through December 31, 2009. Total median costs for patients that received no definitive/systemic treatments (RC, TMT, radiotherapy alone, or chemotherapy alone) were $73,780 vs. $88,275 at 2-and 5-years respectively. Total median costs were significantly higher for TMT than RC at 2-years ($372,839 vs. $191,363, p<0.001) and 5-years ($424,570 vs. $253,651, p<0.001), respectively. TMT had higher outpatient median costs than RC (2-yr: $318,221 vs. $100,900; 5-yr: $367,092 vs. $146,561) with significantly higher costs largely associated with radiology, medications, pathology/laboratory, and other professional services. Out-of-pocket prescription drug costs within 5 years of diagnosis were not significantly different for RC vs. TMT (median, $732 vs. $822; H-L Median, $-17; 95% CI, -$213 to $178).
Conclusions: TMT vs. RC was associated with higher long-term costs among patients with muscle-invasive bladder cancer largely driven by outpatient expenditures. Reduction in costs associated with radiology, medications, pathology/laboratory, and other professional services may improve the value of TMT.
Source of Funding: DOD PRCRP CDA
Methods: This cohort study used the Surveillance, Epidemiology, and End Results (SEER)-Medicare database. Medicare expenditures were summed from inpatient, outpatient, and physician services within 2 and 5 years of diagnosis to determine total costs Total Medicare costs at 2-and 5-years following TMT versus RC were compared using inverse probability of treatment-weighted (IPTW) propensity score models.
Results: A total of 2,537 patients aged 66-85 years diagnosed with clinical stage T2-4a muscle-invasive bladder cancer from January 1, 2002 through December 31, 2009. Total median costs for patients that received no definitive/systemic treatments (RC, TMT, radiotherapy alone, or chemotherapy alone) were $73,780 vs. $88,275 at 2-and 5-years respectively. Total median costs were significantly higher for TMT than RC at 2-years ($372,839 vs. $191,363, p<0.001) and 5-years ($424,570 vs. $253,651, p<0.001), respectively. TMT had higher outpatient median costs than RC (2-yr: $318,221 vs. $100,900; 5-yr: $367,092 vs. $146,561) with significantly higher costs largely associated with radiology, medications, pathology/laboratory, and other professional services. Out-of-pocket prescription drug costs within 5 years of diagnosis were not significantly different for RC vs. TMT (median, $732 vs. $822; H-L Median, $-17; 95% CI, -$213 to $178).
Conclusions: TMT vs. RC was associated with higher long-term costs among patients with muscle-invasive bladder cancer largely driven by outpatient expenditures. Reduction in costs associated with radiology, medications, pathology/laboratory, and other professional services may improve the value of TMT.
Source of Funding: DOD PRCRP CDA

.jpg)
.jpg)