Back
Poster, Podium & Video Sessions
Moderated Poster
MP39: Health Services Research: Value of Care: Cost and Outcomes Measures
MP39-04: Comparison of One-Year Healthcare Expenditure and Utilizations between Minimally Invasive and Open Surgical Approaches among Patients Undergoing Nephrectomy
Sunday, May 15, 2022
8:45 AM – 10:00 AM
Location: Room 228
Kennedy Okhawere*, New York, NY, Gediwon Milky, I-Fan Shih, Yanli Li, Sunnyvale, CA, Ketan Badani, New York, NY
- KO
Poster Presenter(s)
Introduction: Despite the widespread adoption of minimally invasive surgical approaches for partial and radical nephrectomy, its long-term cost-benefit is still heavily criticized. We aim to compare total health care utilization and costs up to one year after minimally invasive surgery (MIS) and open surgery (OS) for radical (RN) and partial nephrectomy (PN).
Methods: A retrospective cohort study of patients who had nephrectomy for kidney cancer was conducted using the IBM® MarketScan® Databases between 2013 and 2018. Outcomes included length of stay and expenditure for index surgery, post-operative 1-year total healthcare expenditure, healthcare utilizations, and total missed workdays due to healthcare utilization. Inverse probability of treatment weighting (IPTW) based on baseline patient characteristics was applied to compare MIS versus OS.
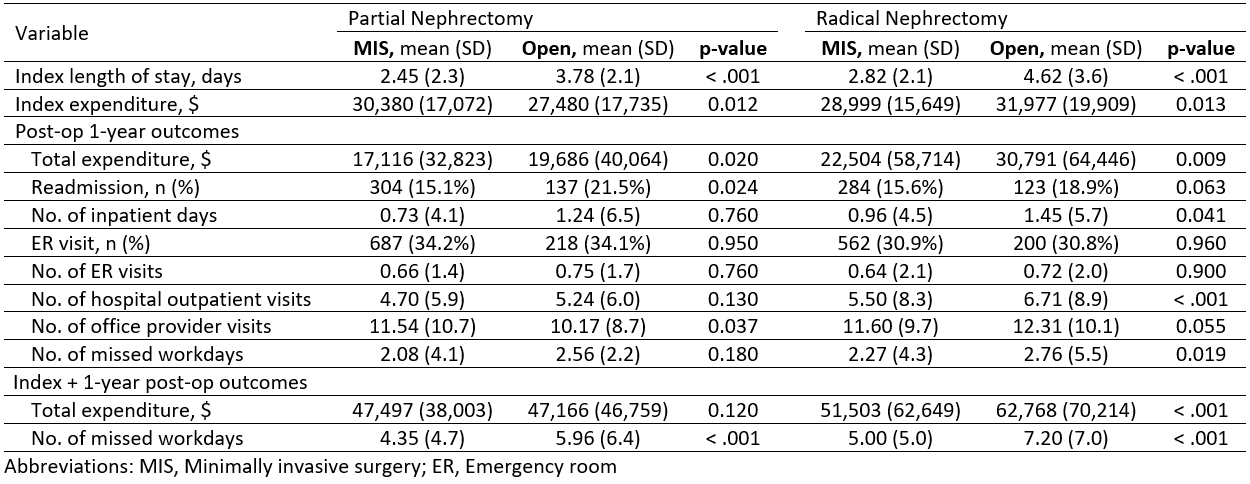
Results: Of 5,104 patients, 2,639 had PN (2,008 MIS vs 631 OS) and 2,465 had RN (1,816 MIS vs 649 OS). MIS patients had lower index length of stay than OS (PN: 2.4 vs 3.8, p < 0.001; and RN: 2.8 vs 4.6, p < 0.001), and lower index expenditure for RN ($28,999 vs $31,977, p = 0.013). For PN, index expenditure was lower for OS ($27,480 vs $30,380 for MIS, p = 0.012). MIS was associated with lower post-operative expenditure than OS (PN: $17,116 vs. $19,686, p = 0.020; and RN: $22,504 vs. $30,791, p = 0.009). MIS patients had lower or comparable readmission rate than OS (PN: 15% vs 21%, p = 0.024; and RN: 15.6% vs 18.9%, p = 0.063). Following RN, MIS patients had fewer resource utilizations than OS (inpatient days: 1.0 vs 1.4 days, p = 0.041; hospital outpatient visits: 5.5 vs 6.7, p < 0.001), translating to fewer missed workdays (2.3 vs. 2.8, p = 0.019).
Conclusions: Irrespective of the cost of the index surgery for both PN and RN, the total cumulative cost in one-year post-discharge was lower for MIS when compared to OS. Several factors might contribute to cost savings after MIS in the post-operative period including reduction in re-admission rate and number of outpatient visits. Our findings suggest that impact on downstream cost and resource utilization should be considered when evaluating surgical approach for both partial and radical nephrectomy.
Source of Funding: Intuitive Surgical Inc.
Methods: A retrospective cohort study of patients who had nephrectomy for kidney cancer was conducted using the IBM® MarketScan® Databases between 2013 and 2018. Outcomes included length of stay and expenditure for index surgery, post-operative 1-year total healthcare expenditure, healthcare utilizations, and total missed workdays due to healthcare utilization. Inverse probability of treatment weighting (IPTW) based on baseline patient characteristics was applied to compare MIS versus OS.
Results: Of 5,104 patients, 2,639 had PN (2,008 MIS vs 631 OS) and 2,465 had RN (1,816 MIS vs 649 OS). MIS patients had lower index length of stay than OS (PN: 2.4 vs 3.8, p < 0.001; and RN: 2.8 vs 4.6, p < 0.001), and lower index expenditure for RN ($28,999 vs $31,977, p = 0.013). For PN, index expenditure was lower for OS ($27,480 vs $30,380 for MIS, p = 0.012). MIS was associated with lower post-operative expenditure than OS (PN: $17,116 vs. $19,686, p = 0.020; and RN: $22,504 vs. $30,791, p = 0.009). MIS patients had lower or comparable readmission rate than OS (PN: 15% vs 21%, p = 0.024; and RN: 15.6% vs 18.9%, p = 0.063). Following RN, MIS patients had fewer resource utilizations than OS (inpatient days: 1.0 vs 1.4 days, p = 0.041; hospital outpatient visits: 5.5 vs 6.7, p < 0.001), translating to fewer missed workdays (2.3 vs. 2.8, p = 0.019).
Conclusions: Irrespective of the cost of the index surgery for both PN and RN, the total cumulative cost in one-year post-discharge was lower for MIS when compared to OS. Several factors might contribute to cost savings after MIS in the post-operative period including reduction in re-admission rate and number of outpatient visits. Our findings suggest that impact on downstream cost and resource utilization should be considered when evaluating surgical approach for both partial and radical nephrectomy.
Source of Funding: Intuitive Surgical Inc.

.jpg)
.jpg)