Back
Poster, Podium & Video Sessions
Moderated Poster
MP39: Health Services Research: Value of Care: Cost and Outcomes Measures
MP39-06: Evaluating the Real-World Payer and Patient Costs of BPH Surgical Management
Sunday, May 15, 2022
8:45 AM – 10:00 AM
Location: Room 228
Kevin Wymer*, Gopal Narang, Phoenix, AZ, Austen Slade, Indianapolis, IN, Vidit Sharma, Viengneesee Thao, Bijan Borah, Rochester, MN, Marcelino Rivera, Indianapolis, IN, Scott Cheney, Mitchell Humphreys, Phoenix, AZ
- KW
Kevin Wymer, MD
Mayo Clinic Arizona
Poster Presenter(s)
Introduction: A multitude of surgical treatment options exist for BPH - with differences in the level of invasiveness, complications, and durability. Despite the high prevalence of BPH treatment and its significant economic impact, limited data are available comparing the financial burden of specific surgical interventions. We therefore sought to compare out-of-pocket (OOP) and health plan paid (HPP) costs of common surgical treatments for BPH.
Methods: We conducted a retrospective cohort study using administrative claims data from the OptumLabs Data Warehouse, which includes data for commercially insured and Medicare Advantage enrollees. Our cohort consisted of patients with a BPH diagnosis who underwent simple prostatectomy (SP), TURP, HoLEP, PVP, UroLift, or Rezum from 2015-2019. Unadjusted average OPP and HPP costs for different follow-up timeframes by treatment type were included. Our analysis was limited to patients continuously enrolled in their health plan for at least 1 year pre- and post-procedure, ages 30-80. Costs were inflation-adjusted to 2020 U.S. dollars using the Consumer Price Index. One-way ANOVA was performed to evaluate for differences in cost.
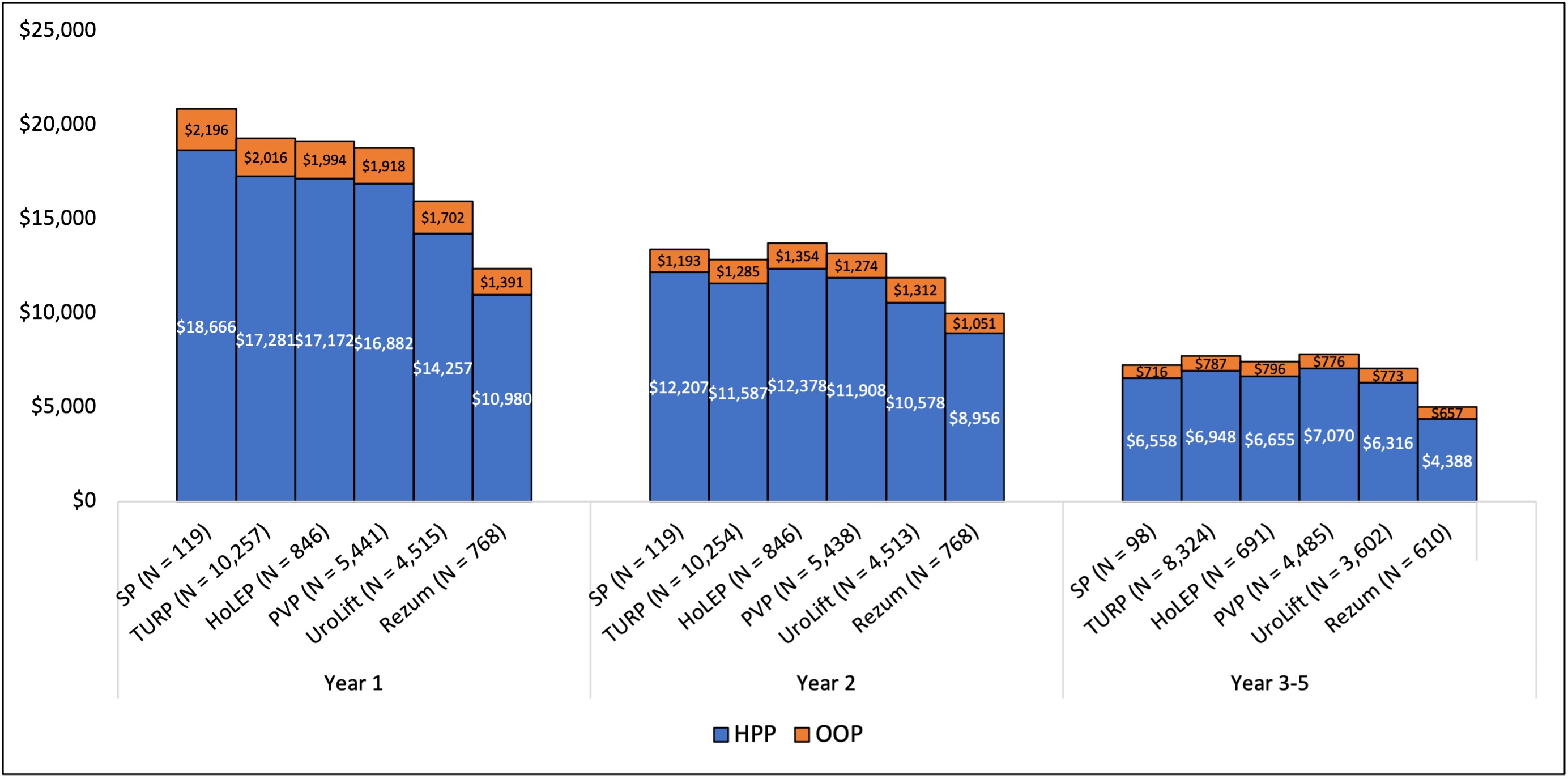
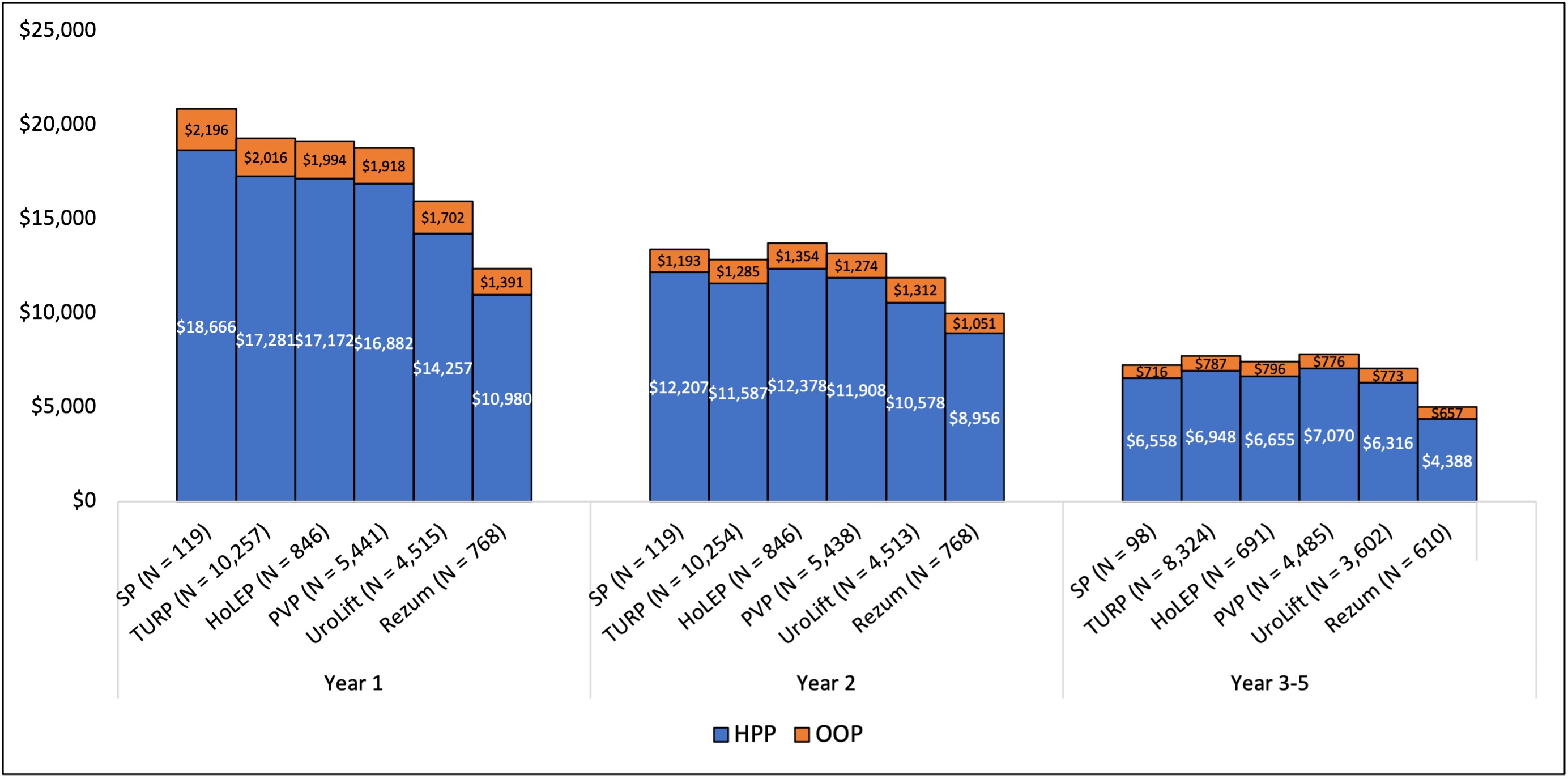
Results: In total, 21,946 patients were included in the analysis. Total HPP and OOP costs for each treatment type by follow-up year are shown in Figure 1. For year 1 (which included the index procedure), there was significant variation in both HPP and OPP costs, with SP associated with highest costs followed by TURP, HoLEP, PVP, UroLift, and Rezum (p <.001). These differences decreased with longer follow up in year 2 and years 3-5, with minimal differences in costs for all procedures except for Rezum which was associated with significantly lower HPP costs (p <.01). There was no significant difference in patient OOP costs among all procedures at 3-5 years (p=.055).
Conclusions: BPH treatment modality has a significant impact on patient and system level costs. These differences are most pronounced within the first year of surgical management, likely related to index procedural costs, complications, and convalescence, and decrease with further follow up. Minimally invasive options, such as Rezum, may offer initial cost reductions; however, such data must be interpreted cautiously without correlation to clinical information, including gland size.
Source of Funding: None
Methods: We conducted a retrospective cohort study using administrative claims data from the OptumLabs Data Warehouse, which includes data for commercially insured and Medicare Advantage enrollees. Our cohort consisted of patients with a BPH diagnosis who underwent simple prostatectomy (SP), TURP, HoLEP, PVP, UroLift, or Rezum from 2015-2019. Unadjusted average OPP and HPP costs for different follow-up timeframes by treatment type were included. Our analysis was limited to patients continuously enrolled in their health plan for at least 1 year pre- and post-procedure, ages 30-80. Costs were inflation-adjusted to 2020 U.S. dollars using the Consumer Price Index. One-way ANOVA was performed to evaluate for differences in cost.
Results: In total, 21,946 patients were included in the analysis. Total HPP and OOP costs for each treatment type by follow-up year are shown in Figure 1. For year 1 (which included the index procedure), there was significant variation in both HPP and OPP costs, with SP associated with highest costs followed by TURP, HoLEP, PVP, UroLift, and Rezum (p <.001). These differences decreased with longer follow up in year 2 and years 3-5, with minimal differences in costs for all procedures except for Rezum which was associated with significantly lower HPP costs (p <.01). There was no significant difference in patient OOP costs among all procedures at 3-5 years (p=.055).
Conclusions: BPH treatment modality has a significant impact on patient and system level costs. These differences are most pronounced within the first year of surgical management, likely related to index procedural costs, complications, and convalescence, and decrease with further follow up. Minimally invasive options, such as Rezum, may offer initial cost reductions; however, such data must be interpreted cautiously without correlation to clinical information, including gland size.
Source of Funding: None

.jpg)
.jpg)