Back
Poster, Podium & Video Sessions
Moderated Poster
MP39: Health Services Research: Value of Care: Cost and Outcomes Measures
MP39-08: Impact of SARS-CoV-2 Pandemic on the Diagnosis And Surgical Intervention Of Common Urological Conditions: Results From A Multi-Institutional Database From The United States
Sunday, May 15, 2022
8:45 AM – 10:00 AM
Location: Room 228
Maxwell Towe*, Sirpi Nackeeran, Mohammad Hout, Abhishek Bhat, Ranjith Ramasamy, Hemendra Shah, Miami, FL
- MT
Poster Presenter(s)
Introduction: The SARS-CoV-2 (COVID) pandemic threatened access to healthcare, raising concerns that patients were going underdiagnosed and undertreated. The aim of our study was to understand the impact of the COVID pandemic on diagnosis and surgical management of common urological conditions.
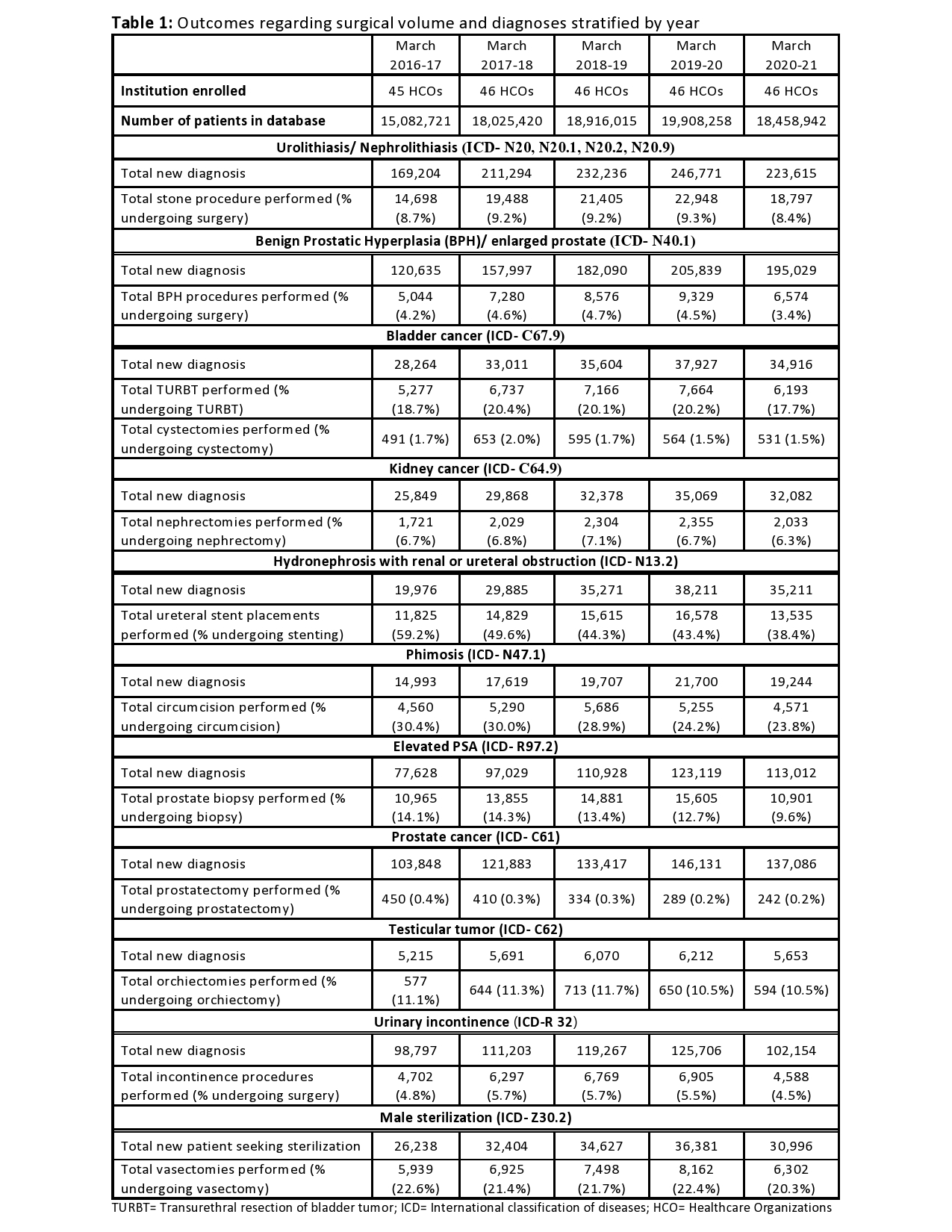
Methods: Using a large multi-center electronic health record network (TRINETx) consisting of 46 healthcare organizations, we conducted an epidemiological study investigating the number of patients newly diagnosed with common urological conditions and those undergoing urologic surgeries at yearly intervals from March 1st, 2016 to March 1st, 2021. Relevant international classification of diseases (ICD) codes used to identify urologic conditions are elaborated on in Table 1. Current procedural terminology (CPT) codes used to identify surgeries are detailed in Figure 1. We then determined the percentage of newly diagnosed patients who underwent surgery for each specific year.
Results: We saw a decrease in number of all urologic surgeries being performed during the initial year of the pandemic (Figure 1). From March 2020-2021, there was a >20% decrease in surgical case load for benign prostatic hyperplasia procedures (-29.5%), prostate biopsies (-30.1%), incontinence procedures (-33.6%), and vasectomies (-22.8%), compared to the preceding year. Radical cystectomies and orchiectomies saw the lowest decrease, -5.9% and -8.6%, respectively. A similar trend was seen in the number of individuals newly diagnosed with urologic conditions and percentage of patients undergoing surgical intervention. The lowest drops were seen with ureteral stent placements (-5.0%) and prostate biopsies (-3.1%).
Conclusions: The number of people receiving urologic diagnoses and surgical case load for urologic procedures significantly reduced during the first year of the COVID pandemic. Providers should be aware of this healthcare disparity, and greater efforts made to identify these “missed” patients moving forward.
Source of Funding: Research was supported by Acerus Pharmaceuticals in the form of an educational grant used to access the TriNetX database. Acerus Pharmaceuticals was not involved in the planning, design, writing or any other aspect of this project.
This work was also supported by National Institutes of Health Grant R01 DK130991 and Clinician Scientist Development Grant from the American Cancer Society to Ranjith Ramasamy.

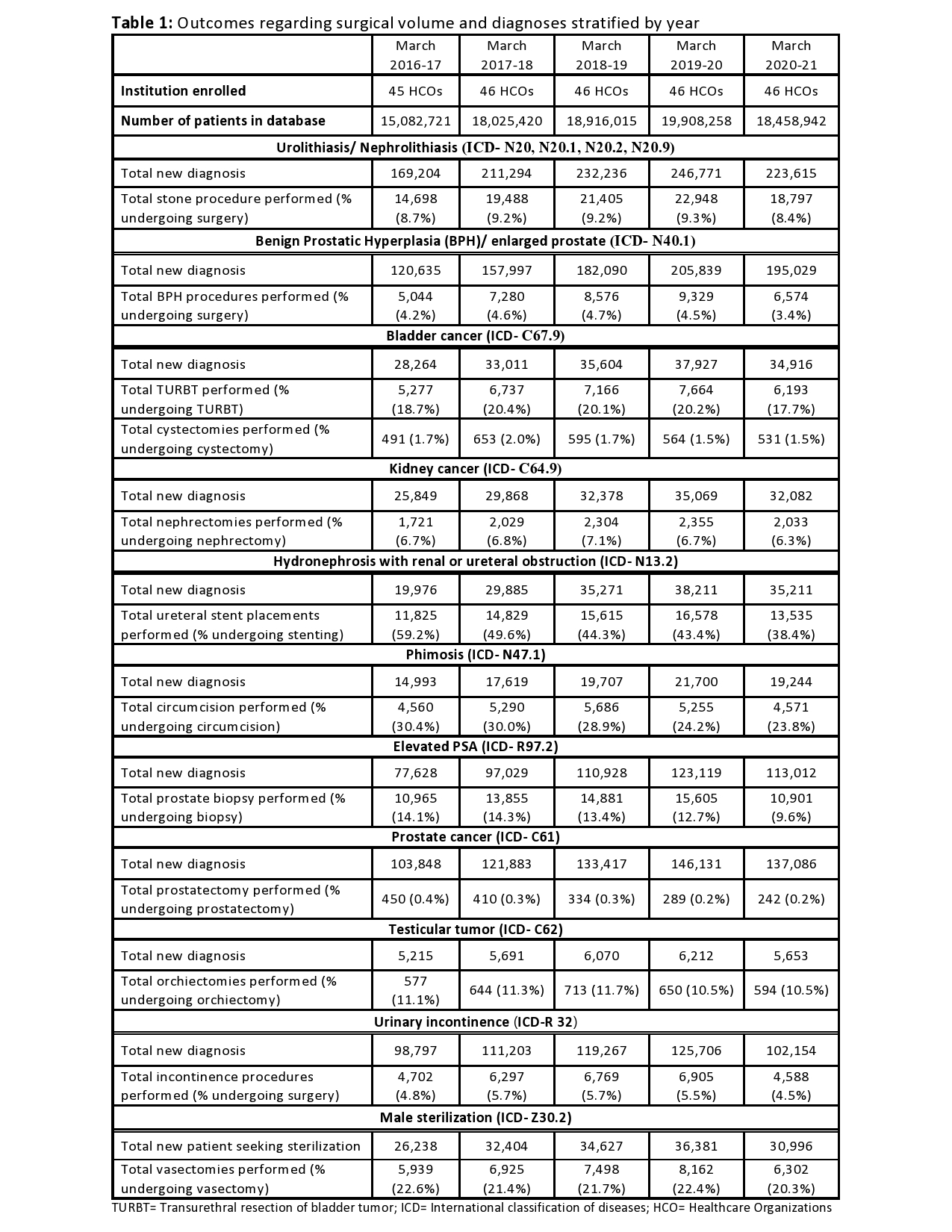
Methods: Using a large multi-center electronic health record network (TRINETx) consisting of 46 healthcare organizations, we conducted an epidemiological study investigating the number of patients newly diagnosed with common urological conditions and those undergoing urologic surgeries at yearly intervals from March 1st, 2016 to March 1st, 2021. Relevant international classification of diseases (ICD) codes used to identify urologic conditions are elaborated on in Table 1. Current procedural terminology (CPT) codes used to identify surgeries are detailed in Figure 1. We then determined the percentage of newly diagnosed patients who underwent surgery for each specific year.
Results: We saw a decrease in number of all urologic surgeries being performed during the initial year of the pandemic (Figure 1). From March 2020-2021, there was a >20% decrease in surgical case load for benign prostatic hyperplasia procedures (-29.5%), prostate biopsies (-30.1%), incontinence procedures (-33.6%), and vasectomies (-22.8%), compared to the preceding year. Radical cystectomies and orchiectomies saw the lowest decrease, -5.9% and -8.6%, respectively. A similar trend was seen in the number of individuals newly diagnosed with urologic conditions and percentage of patients undergoing surgical intervention. The lowest drops were seen with ureteral stent placements (-5.0%) and prostate biopsies (-3.1%).
Conclusions: The number of people receiving urologic diagnoses and surgical case load for urologic procedures significantly reduced during the first year of the COVID pandemic. Providers should be aware of this healthcare disparity, and greater efforts made to identify these “missed” patients moving forward.
Source of Funding: Research was supported by Acerus Pharmaceuticals in the form of an educational grant used to access the TriNetX database. Acerus Pharmaceuticals was not involved in the planning, design, writing or any other aspect of this project.
This work was also supported by National Institutes of Health Grant R01 DK130991 and Clinician Scientist Development Grant from the American Cancer Society to Ranjith Ramasamy.


.jpg)
.jpg)