Back
Poster, Podium & Video Sessions
Moderated Poster
MP39: Health Services Research: Value of Care: Cost and Outcomes Measures
MP39-11: Cost-Effectiveness of Holmium Laser Enucleation of the Prostate: Insights from a Markov Model Comparing BPH Surgical Options for Glands <80g
Sunday, May 15, 2022
8:45 AM – 10:00 AM
Location: Room 228
Kevin Wymer*, Gopal Narang, Phoenix, AZ, Austen Slade, Indianapolis, IN, Vidit Sharma, Viengneesee Thao, Bijan Borah, Bijan Borah, Rochester, MN, Marcelino Rivera, Indianapolis, IN, Scott Cheney, Mitchell Humphreys, Phoenix, AZ
- KW
Kevin Wymer, MD
Mayo Clinic Arizona
Poster Presenter(s)
Introduction: A multitude of surgical treatment options exist for BPH- with differences in the level of invasiveness, complications, and treatment durability.The costs associated with BPH management are also substantial, with estimates of $1,500 and $4 billion annually for patients and the healthcare system, respectively. This study compares the cost-effectiveness of surgical interventions for BPH patients with a prostate <80g.
Methods: Using a Markov Model, a cost-effectiveness analysis compared holmium laser enucleation of the prostate (HoLEP), bipolar TURP (B-TURP), Rezum, and UroLift. Model probabilities were drawn from prospective and randomized control trials while utility values were calculated from post-op symptom scores. Base case analysis was performed at 5 years with an extrapolated lifetime horizon of 20 years. Outcomes included quality-adjusted life years (QALYs), 2021 Medicare costs, and incremental cost-effectiveness ratios (ICERs), with a willingness-to-pay threshold of $100,000/QALY. Univariate and probabilistic sensitivity analyses were performed.
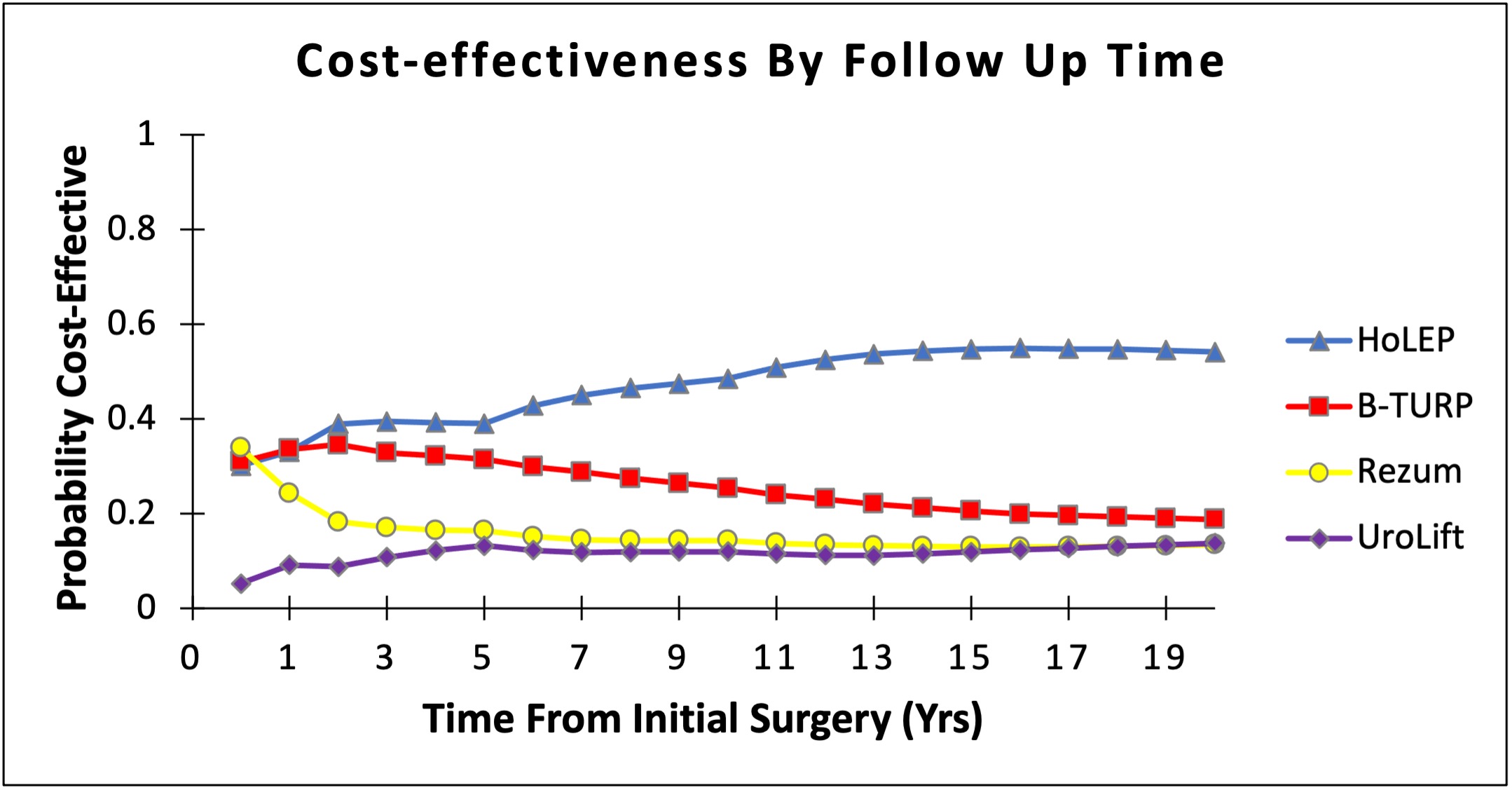
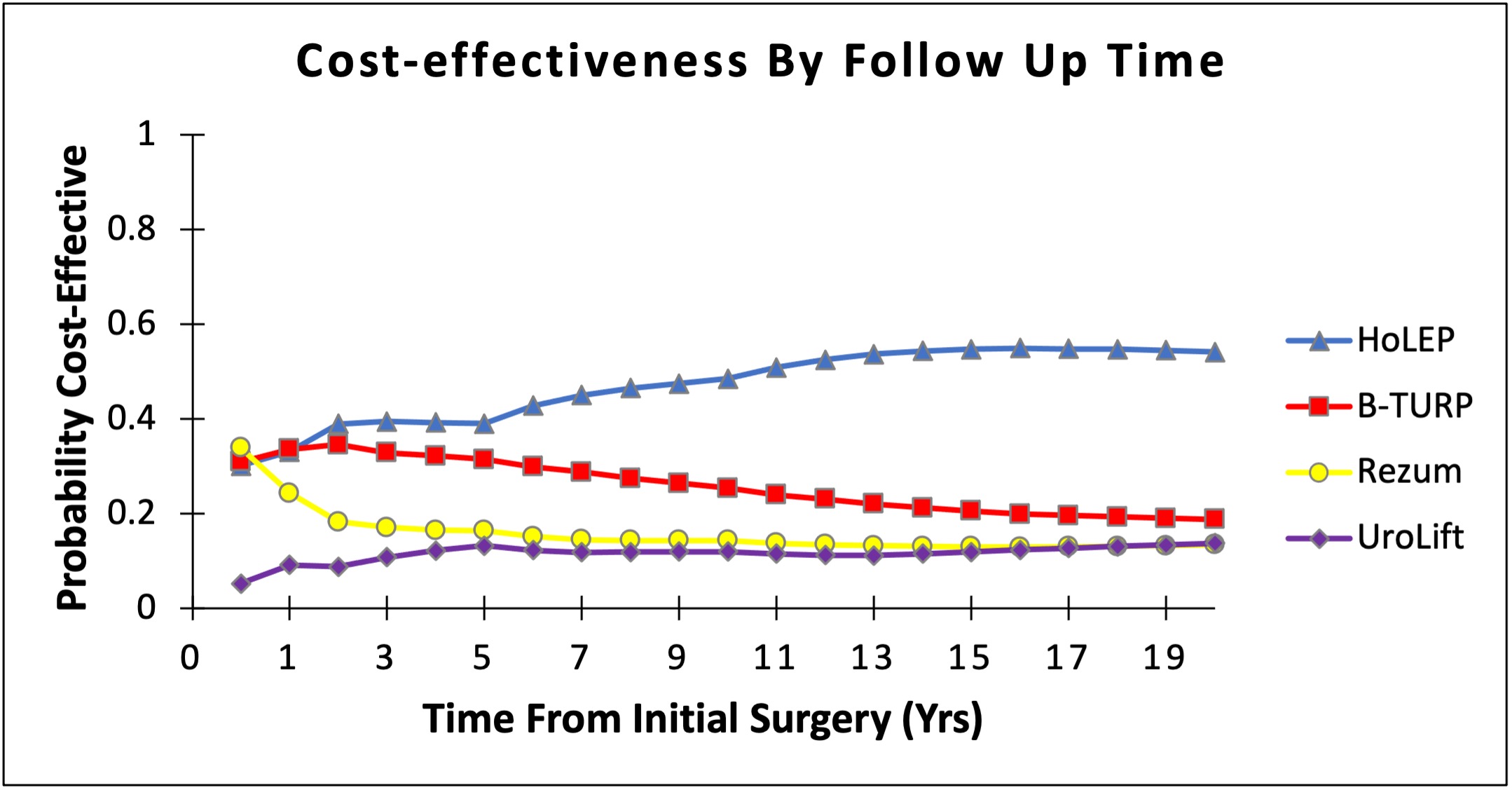
Results: At 5 years, costs per patient were $3,292 (Rezum), $6,532 (HoLEP), $6,670 (B-TURP), and $10,257 (UroLift). HoLEP resulted in the highest QALYs (4.66), followed by B-TURP (4.60), UroLift (4.38), and Rezum (4.38). HoLEP was the most cost-effective (ICER $11,847). B-TURP was cost-effective relative to Rezum (ICER $15,469) but not HoLEP, and UroLift was not cost-effective relative to any other treatment. B-TURP became cost-effective if HoLEP costs increased two-fold, stress incontinence after HoLEP increased ten-fold, or utility following HoLEP decreased. Rezum and UroLift did not become cost-effective at 5 years even with variation in costs and complications. Rezum was preferred at very short follow-up ( <1 year) in probabilistic sensitivity analyses, while HoLEP was strongly preferred with longer follow-up (Figure 1).
Conclusions: Minimally invasive surgical therapies (MIST) such as Rezum or Urolift may be cost-effective in the short-term due to low procedural costs and few acute complications. However, HoLEP is the most cost-effective treatment for BPH glands <80g in the long-term.
Source of Funding: Mayo Clinic Kern Scholars Program
Methods: Using a Markov Model, a cost-effectiveness analysis compared holmium laser enucleation of the prostate (HoLEP), bipolar TURP (B-TURP), Rezum, and UroLift. Model probabilities were drawn from prospective and randomized control trials while utility values were calculated from post-op symptom scores. Base case analysis was performed at 5 years with an extrapolated lifetime horizon of 20 years. Outcomes included quality-adjusted life years (QALYs), 2021 Medicare costs, and incremental cost-effectiveness ratios (ICERs), with a willingness-to-pay threshold of $100,000/QALY. Univariate and probabilistic sensitivity analyses were performed.
Results: At 5 years, costs per patient were $3,292 (Rezum), $6,532 (HoLEP), $6,670 (B-TURP), and $10,257 (UroLift). HoLEP resulted in the highest QALYs (4.66), followed by B-TURP (4.60), UroLift (4.38), and Rezum (4.38). HoLEP was the most cost-effective (ICER $11,847). B-TURP was cost-effective relative to Rezum (ICER $15,469) but not HoLEP, and UroLift was not cost-effective relative to any other treatment. B-TURP became cost-effective if HoLEP costs increased two-fold, stress incontinence after HoLEP increased ten-fold, or utility following HoLEP decreased. Rezum and UroLift did not become cost-effective at 5 years even with variation in costs and complications. Rezum was preferred at very short follow-up ( <1 year) in probabilistic sensitivity analyses, while HoLEP was strongly preferred with longer follow-up (Figure 1).
Conclusions: Minimally invasive surgical therapies (MIST) such as Rezum or Urolift may be cost-effective in the short-term due to low procedural costs and few acute complications. However, HoLEP is the most cost-effective treatment for BPH glands <80g in the long-term.
Source of Funding: Mayo Clinic Kern Scholars Program

.jpg)
.jpg)