Back
Poster, Podium & Video Sessions
Moderated Poster
MP39: Health Services Research: Value of Care: Cost and Outcomes Measures
MP39-17: Advanced Practice Providers and Patient Access in Academic Medical Centers: A Secret Shopper Study
Sunday, May 15, 2022
8:45 AM – 10:00 AM
Location: Room 228
Armaan Singh*, Jared Lassner, Ashley Diaz, Marc Sleiman, Parth Modi, CHICAGO, IL
- AS
Armaan Singh, BA
Pritzker School of Medicine
Poster Presenter(s)
Introduction: As the need for urologic care increases in the US, advanced practice providers (APPs), such as nurse practitioners and physician assistants, play a growing role in urologic care at academic medical centers (AMCs). However, the impact of APPs in improving patient access in academic settings is unknown, as this may be impacted by several factors including: state laws, hospital policies, and resident education needs. We examined the impact of APPs on new patient wait times in AMCs in the United States.
Methods: We conducted a “secret shopper” study in which researchers posing as caretakers called academic medical centers to schedule an appointment for an elderly grandfather with gross hematuria. We called all US medical centers that contain an accredited urology residency program. For each center, we recorded the number of days until the first offered appointment, the type of provider that was offered, the availability of an alternative provider, and potential wait time for that alternative visit.
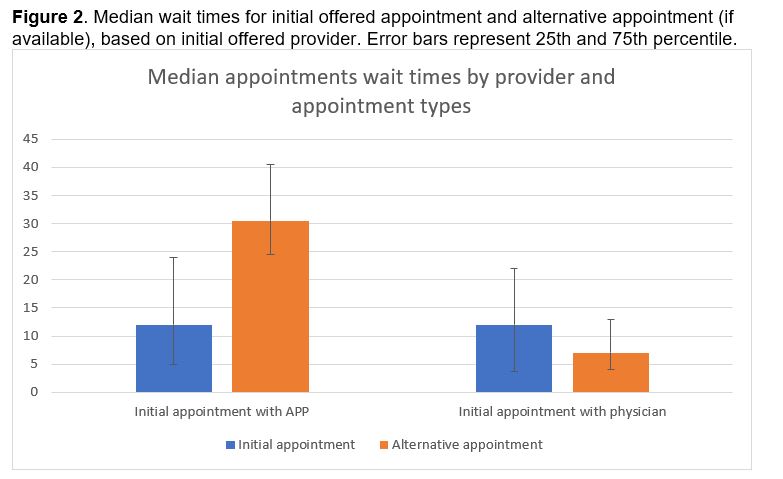
Results: Of 111 AMCs at which we scheduled an appointment, 101 (90%) employed at least one APP. Most AMCs offered appointments with both APPs and physicians (54%), while 37% of AMCs offered appointments with only physicians and 9% of AMCs offered appointments with only APPs. Initial appointments with an APP had the same median wait time as initial appointments with a physician (12 days). When requested for an earlier appointment regardless of provider type, AMCs that initially offered physician appointments were able to offer appointments with a significantly shorter median wait time with an APP (7 days vs 12 days; P=0.05).
Conclusions: Our study suggests that while there is a lack of uniformity in new patient visit protocols, AMCs can use APPs help lower wait times for new patient visits. It is possible that AMCs that offered initial appointments with physicians had more availability across all providers than did AMCs that offered initial appointments with APPs. Patients who are willing to see all types of providers may be able to advocate for shorter wait times. Further work is needed to better elucidate the role of APPs in these practices and how best they might be deployed.
Source of Funding: n/a
Methods: We conducted a “secret shopper” study in which researchers posing as caretakers called academic medical centers to schedule an appointment for an elderly grandfather with gross hematuria. We called all US medical centers that contain an accredited urology residency program. For each center, we recorded the number of days until the first offered appointment, the type of provider that was offered, the availability of an alternative provider, and potential wait time for that alternative visit.
Results: Of 111 AMCs at which we scheduled an appointment, 101 (90%) employed at least one APP. Most AMCs offered appointments with both APPs and physicians (54%), while 37% of AMCs offered appointments with only physicians and 9% of AMCs offered appointments with only APPs. Initial appointments with an APP had the same median wait time as initial appointments with a physician (12 days). When requested for an earlier appointment regardless of provider type, AMCs that initially offered physician appointments were able to offer appointments with a significantly shorter median wait time with an APP (7 days vs 12 days; P=0.05).
Conclusions: Our study suggests that while there is a lack of uniformity in new patient visit protocols, AMCs can use APPs help lower wait times for new patient visits. It is possible that AMCs that offered initial appointments with physicians had more availability across all providers than did AMCs that offered initial appointments with APPs. Patients who are willing to see all types of providers may be able to advocate for shorter wait times. Further work is needed to better elucidate the role of APPs in these practices and how best they might be deployed.
Source of Funding: n/a

.jpg)
.jpg)