Back
Poster, Podium & Video Sessions
Moderated Poster
MP39: Health Services Research: Value of Care: Cost and Outcomes Measures
MP39-20: Access to definitive treatment and survival for intermediate-risk and high-risk prostate cancer at hospitals systems serving health disparity populations (HSDPs)
Sunday, May 15, 2022
8:45 AM – 10:00 AM
Location: Room 228
David-Dan Nguyen*, Muhieddine Labban, Logan Briggs, Alexander P. Cole, Stuart R. Lipsitz, Hari S. Iyer, Timothy R. Rebbeck, Joel S. Weissman, Quoc-Dien Trinh, Boston, MA

David-Dan Nguyen, MPH
University of Toronto
Poster Presenter(s)
Introduction: In the United States, Black men with prostate cancer (PCa) are less likely to receive definitive treatment and have worse survival compared to White men. Research suggests that racial disparities in PCa may be attributable to the geographic site of care where Black men are more likely to be treated at resource-deprived facilities. Thus, we sought to examine guideline concordant definitive treatment, time to treatment initiation (TTI) within 90 days of diagnosis, and survival between HSDPs and non-HSDPs among men with PCa.
Methods: We queried the National Cancer Database (2004-2016) for patients with intermediate- or high-risk PCa eligible for definitive treatment. We defined HSDPs as minority-serving hospitals (MSHs) – facilities in the highest decile of proportion of Non-Hispanic Black (NHB) or Hispanic cancer patients – and/or high-burden safety-net hospitals (SNHs) – facilities in the highest quartile of proportion of underinsured cancer patients. We used mixed-effect models with facility-level random intercept to compare the outcomes of HSDPs and non-HSDPs and mixed-effect survival models with Weibull distribution among the entire cohort and among men who received definitive treatment. We conducted sensitivity analyses by HSDP facility subtype and examined interactions between race and HSDP status.
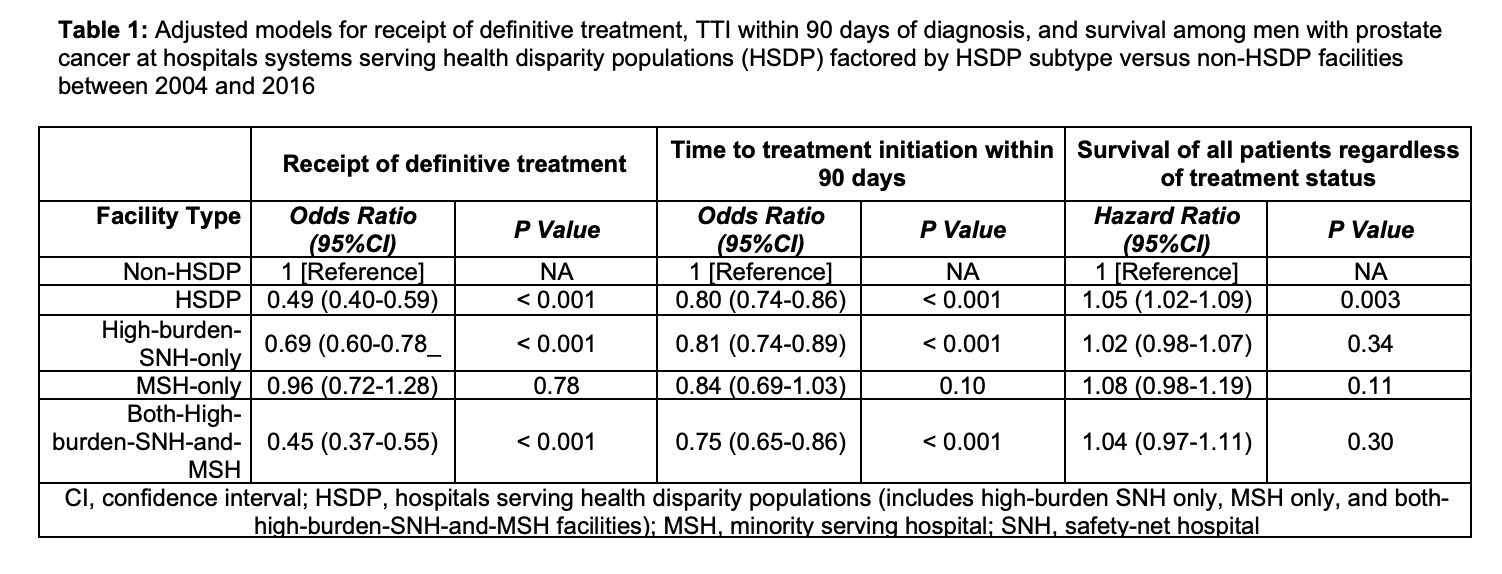
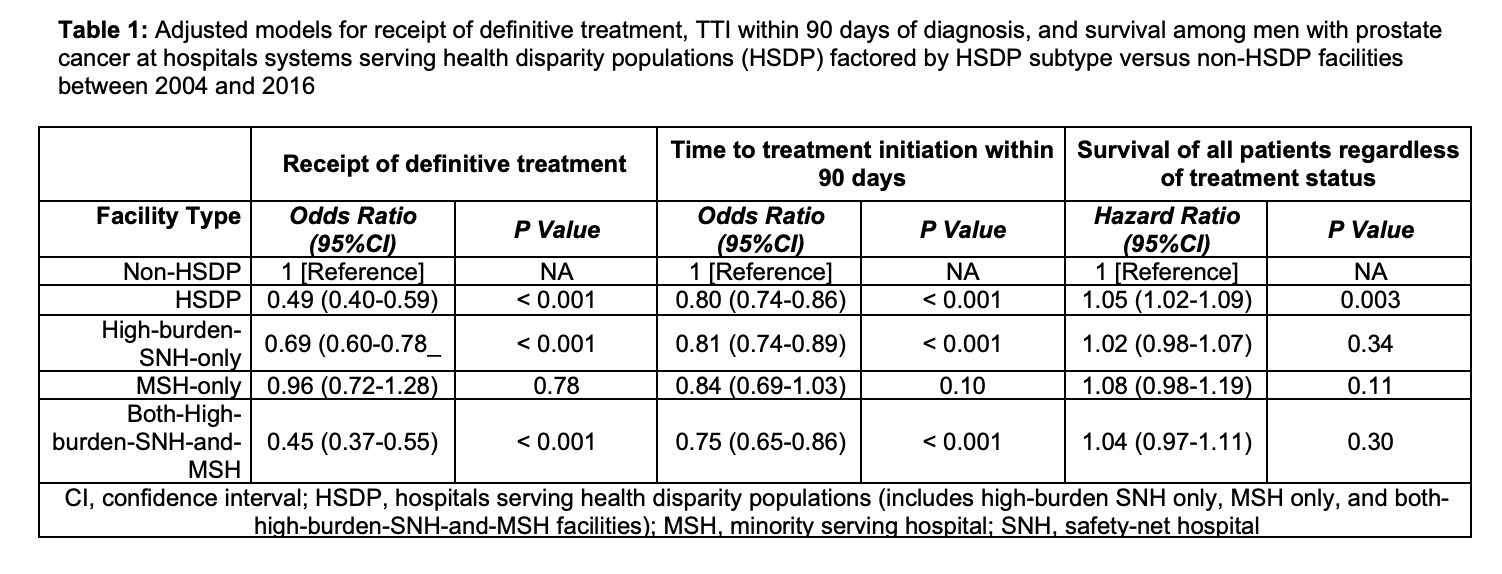
Results: The cohort included 968 non-HSDPs (72.2%) and 373 HSDPs (27.8%) facilities of which 239 (64.1%) were high-burden SNH-only, 39 (10.4%) were MSH-only, and 95 (25.5%) were both-high-burden-SNH-and-MSH facilities. Treatment at HSDPs was associated with lower odds of receipt of definitive treatment, TTI within 90 days of diagnosis, and worse survival (Table 1). Most of the disparities in outcomes were driven by both-high-burden-SNH-and-MSH facilities. Additionally, NHB men at HSDPs had worse outcomes than NHB men treated at non-HSDPs as well as NHW men treated at either facility types.
Conclusions: Patients, especially NHB men, treated at HSDPs were less likely to receive timely definitive treatment and had worse survival. Thus, NHB men with PCa are doubly disadvantaged, since they are more likely to be treated at hospitals with worse outcomes and have worse outcomes than other patients at those same institutions.
Source of Funding: None
Methods: We queried the National Cancer Database (2004-2016) for patients with intermediate- or high-risk PCa eligible for definitive treatment. We defined HSDPs as minority-serving hospitals (MSHs) – facilities in the highest decile of proportion of Non-Hispanic Black (NHB) or Hispanic cancer patients – and/or high-burden safety-net hospitals (SNHs) – facilities in the highest quartile of proportion of underinsured cancer patients. We used mixed-effect models with facility-level random intercept to compare the outcomes of HSDPs and non-HSDPs and mixed-effect survival models with Weibull distribution among the entire cohort and among men who received definitive treatment. We conducted sensitivity analyses by HSDP facility subtype and examined interactions between race and HSDP status.
Results: The cohort included 968 non-HSDPs (72.2%) and 373 HSDPs (27.8%) facilities of which 239 (64.1%) were high-burden SNH-only, 39 (10.4%) were MSH-only, and 95 (25.5%) were both-high-burden-SNH-and-MSH facilities. Treatment at HSDPs was associated with lower odds of receipt of definitive treatment, TTI within 90 days of diagnosis, and worse survival (Table 1). Most of the disparities in outcomes were driven by both-high-burden-SNH-and-MSH facilities. Additionally, NHB men at HSDPs had worse outcomes than NHB men treated at non-HSDPs as well as NHW men treated at either facility types.
Conclusions: Patients, especially NHB men, treated at HSDPs were less likely to receive timely definitive treatment and had worse survival. Thus, NHB men with PCa are doubly disadvantaged, since they are more likely to be treated at hospitals with worse outcomes and have worse outcomes than other patients at those same institutions.
Source of Funding: None

.jpg)
.jpg)