Back
Poster, Podium & Video Sessions
Moderated Poster
MP40: Bladder Cancer: Upper Tract Transitional Cell Carcinoma I
MP40-10: Survival Outcomes of Upper Tract Urothelial Carcinoma Patients Treated with Therapeutic Endoscopic Management
Sunday, May 15, 2022
8:45 AM – 10:00 AM
Location: Room 225
Wesley Yip*, Peter Reisz, Amy Tin, Nicole Benfante, Eugene Cha, Eugene Pietzak, Ari Hakimi, Jonathan Coleman, New York, NY

Wesley Yip, MD
Memorial Sloan Kettering Cancer Center
Poster Presenter(s)
Introduction: Radical nephroureterectomy for upper tract urothelial carcinoma (UTUC) is associated with significant morbidity and renal dysfunction. Interest has increased in endoscopic, kidney-sparing treatment options. We aim to characterize the survival outcomes of UTUC patients treated with therapeutic ureteroscopy (tURS) at our institution.
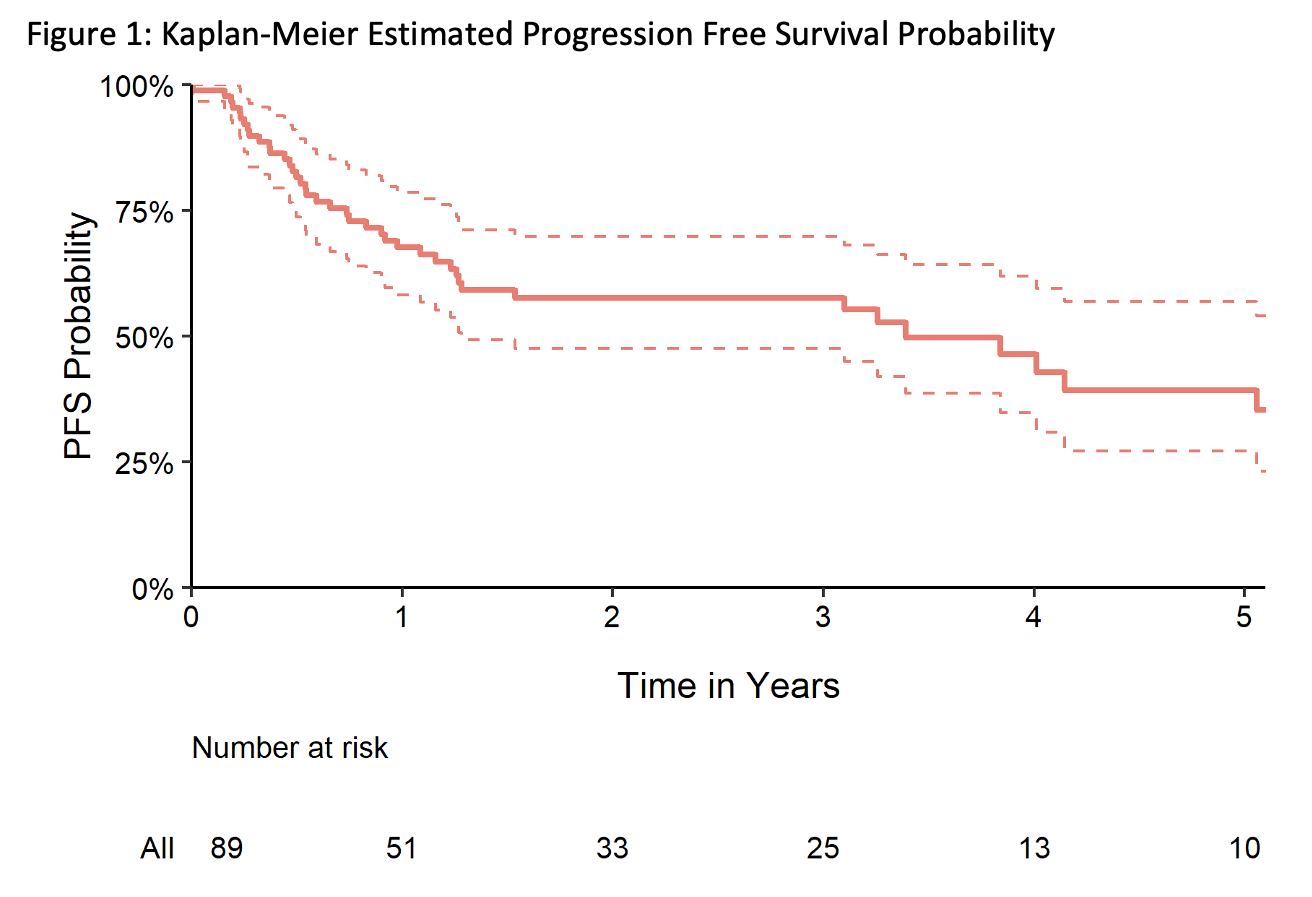
Methods: We retrospectively reviewed all patients treated for UTUC with tURS, defined as two or more URS with therapeutic intent to eradicate all visible tumor. Kaplan-Meier figures were created for three outcomes, including progression-free (PFS), metastasis-free (MFS), and cancer-specific survival (CSS). Progression was defined as converting from negative or low to high-grade disease on follow-up URS, proceeding to systemic therapy, or undergoing ureterectomy/nephroureterectomy. The association between each outcome and certain risk factors at diagnostic URS (tumor grade/size/multiplicity, carcinoma in situ, and variant histology) was assessed by univariable Cox proportional hazard regression models.
Results: 89 patients underwent tURS between 2010 and 2021. Median age was 70 years (IQR 62, 78), the majority were male (69%), and with clinical Ta disease (81%). 33 (37%) patients underwent tURS at the same time as their initial diagnostic URS. Among the remaining 56 patients, the median time from diagnostic to therapeutic URS was 10 weeks (IQR 5, 21). 43 patients progressed, 5 patients developed metastases, and 3 patients died from disease. Median follow-up among patients who did not progress was 2.1 years. Of the patients who progressed, 12 (28%) had high-grade disease on follow-up URS, 4 (9.3%) underwent systemic therapy, 26 (60%) underwent nephroureterectomy, and 1 (2.2%) underwent ureterectomy. Kaplan-Meier estimated one-year and three-years PFS were 68% (95% CI 58%, 79%) and 58% (95% CI 48%, 70%), respectively (Figure 1). Kaplan-Meier estimated 5-year MFS and CSS were 91% (95% CI 83%, 100%) and 96% (95% CI 91%, 100%), respectively.
Conclusions: Endoscopic management is an efficacious treatment option for highly selected UTUC patients based on PFS. A proportion of patients may proceed to salvage therapies; however, metastases and death from disease are rare.
Source of Funding: Thompson Family Foundation, Ruth L. Kirschstein National Research Service Award T32CA082088
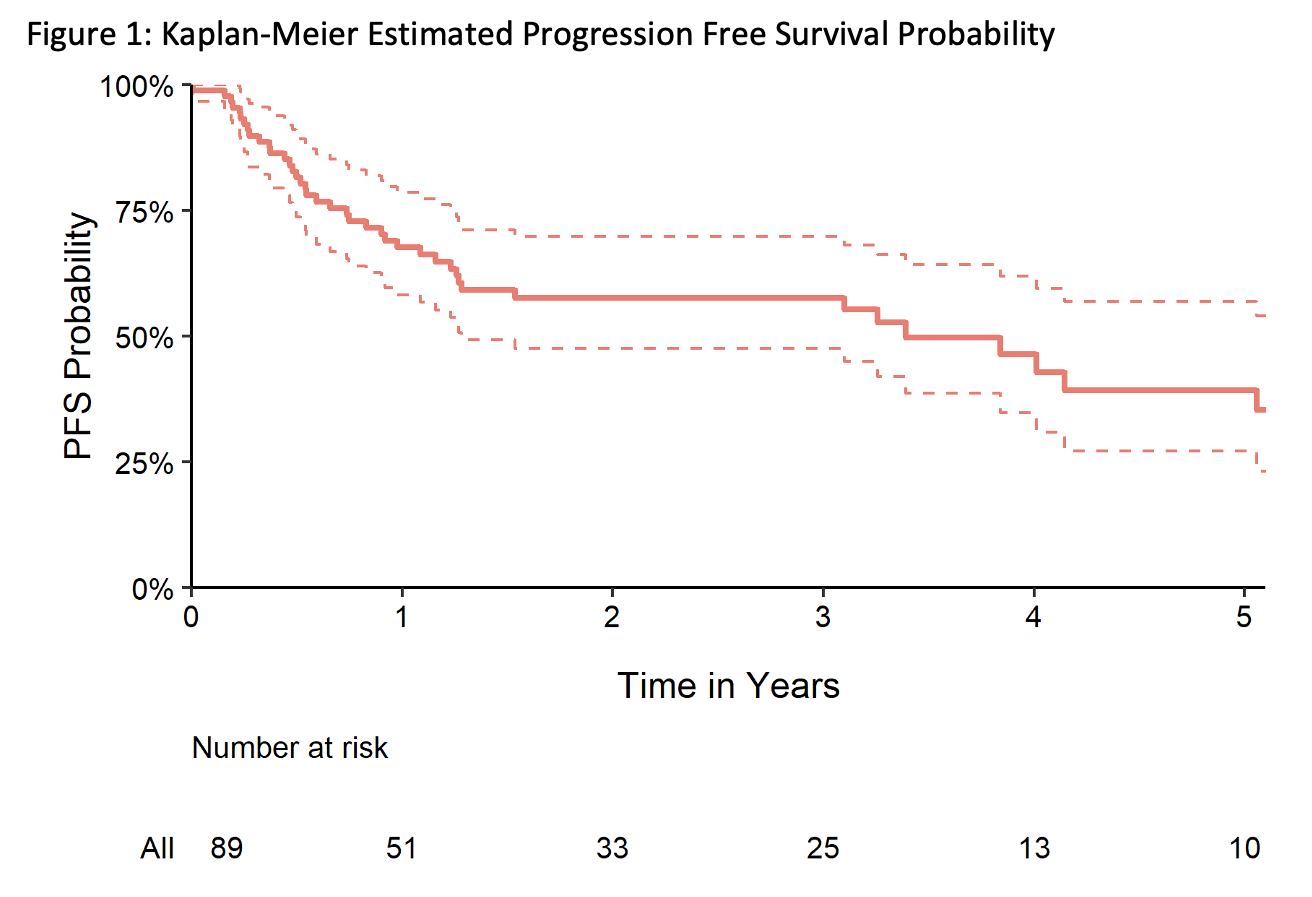
Methods: We retrospectively reviewed all patients treated for UTUC with tURS, defined as two or more URS with therapeutic intent to eradicate all visible tumor. Kaplan-Meier figures were created for three outcomes, including progression-free (PFS), metastasis-free (MFS), and cancer-specific survival (CSS). Progression was defined as converting from negative or low to high-grade disease on follow-up URS, proceeding to systemic therapy, or undergoing ureterectomy/nephroureterectomy. The association between each outcome and certain risk factors at diagnostic URS (tumor grade/size/multiplicity, carcinoma in situ, and variant histology) was assessed by univariable Cox proportional hazard regression models.
Results: 89 patients underwent tURS between 2010 and 2021. Median age was 70 years (IQR 62, 78), the majority were male (69%), and with clinical Ta disease (81%). 33 (37%) patients underwent tURS at the same time as their initial diagnostic URS. Among the remaining 56 patients, the median time from diagnostic to therapeutic URS was 10 weeks (IQR 5, 21). 43 patients progressed, 5 patients developed metastases, and 3 patients died from disease. Median follow-up among patients who did not progress was 2.1 years. Of the patients who progressed, 12 (28%) had high-grade disease on follow-up URS, 4 (9.3%) underwent systemic therapy, 26 (60%) underwent nephroureterectomy, and 1 (2.2%) underwent ureterectomy. Kaplan-Meier estimated one-year and three-years PFS were 68% (95% CI 58%, 79%) and 58% (95% CI 48%, 70%), respectively (Figure 1). Kaplan-Meier estimated 5-year MFS and CSS were 91% (95% CI 83%, 100%) and 96% (95% CI 91%, 100%), respectively.
Conclusions: Endoscopic management is an efficacious treatment option for highly selected UTUC patients based on PFS. A proportion of patients may proceed to salvage therapies; however, metastases and death from disease are rare.
Source of Funding: Thompson Family Foundation, Ruth L. Kirschstein National Research Service Award T32CA082088

.jpg)
.jpg)