Back
Poster, Podium & Video Sessions
Moderated Poster
MP41: Surgical Technology & Simulation: Training & Skills Assessment
MP41-10: Using Customized Feedback to Expedite the Acquisition of Robotic Suturing Skills
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 228
Runzhuo Ma*, Jessica H Nguyen, Andrew Cowan, Ryan S Lee, Taseen Haque, Jonathan You, Sidney I Roberts, Steven Cen, Los Angeles, CA, Anthony Jarc, Norcross, GA, Andrew J Hung, Los Angeles, CA

Runzhuo Ma, MD
USC urology
Poster Presenter(s)
Introduction: Surgical feedback is usually provided by supervising surgeons in the operating room. In a previous study, we identified eight objective suturing performance metrics most predictive of urinary continence recovery after robotic radical prostatectomy. In this study, we aim to use a systematic way to provide customized feedback based on these metrics to expedite the acquisition of robotic suturing skills.
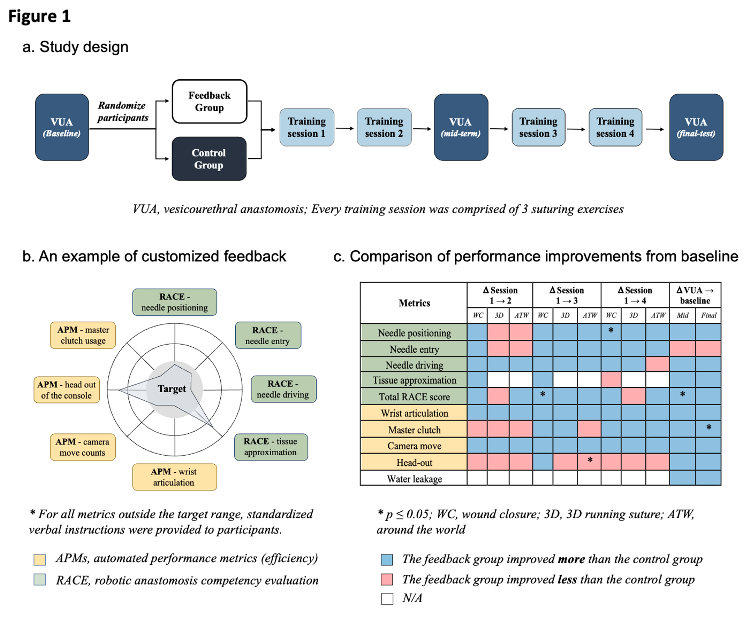
Methods: Training surgeons (prior robotic surgery caseload =15) were recruited and randomized to either the feedback group (FG) or the control group (CG). Both groups completed 3 dry-lab vesicourethral anastomoses (VUAs) and four suturing training sessions with 3 exercises (Fig 1a). Performance metrics were recorded and water-tight test was performed after VUA.
The FG received formative feedback on metrics they failed to pass, benchmarked by the performance of 8 experienced robotic surgeons (prior robotic surgery caseload >100) (Fig 1b). Automated performance metrics (APMs) were derived from the kinematics and system events data of the daVinci robotic system, representing efficiency and console manipulation competency. Robotic anastomosis competency evaluation (RACE) scores assess suturing technical skills. RACE scores were evaluated independently by =2 trained-assessors blinded to participants’ identity. Averaged scores were used for analysis. The intra-class coefficients (ICCs) were measured to monitor the inter-rater reliability. Metric improvement from baseline was compared between the FG and the CG by generalized linear mixed model.
Results: 23 participants were randomized to the FG (N=11) and the CG (N=12). The experience levels and baseline VUA metrics were comparable between groups. The ICC was moderately high for all RACE skill domains (ICCs>0.58, p<0.05). Overall, most metrics of the FG improved more than the CG (Fig 1c). Specifically in VUA tests, the total RACE scores of FG improved more than the CG at the mid-term VUA (mean, ?FG 4.5 vs ?CG 1.1, p=0.05). This difference remained but non-statistically significant in the final VUA (?FG 5.3 vs ?CG 4.9, p=0.78).
Conclusions: Customized feedback based on select APMs and RACE scores may expedite the acquisition of robotic suturing skills. This pilot study paves the way to larger randomized-controlled trials on the efficacy of feedback.
Source of Funding: This study was funded in part by an Intuitive Surgical Clinical Grant and the National Institute Of Biomedical Imaging And Bioengineering of the National Institutes of Health under Award Number K23EB026493.
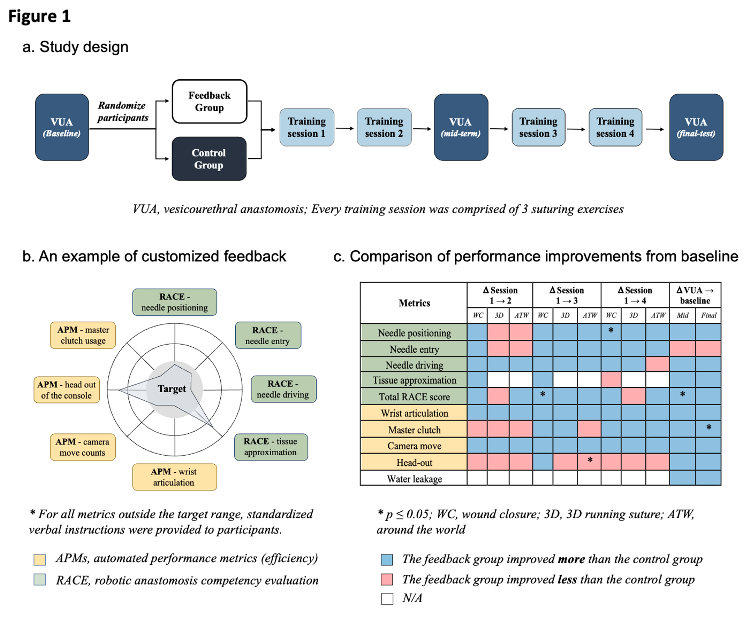
Methods: Training surgeons (prior robotic surgery caseload =15) were recruited and randomized to either the feedback group (FG) or the control group (CG). Both groups completed 3 dry-lab vesicourethral anastomoses (VUAs) and four suturing training sessions with 3 exercises (Fig 1a). Performance metrics were recorded and water-tight test was performed after VUA.
The FG received formative feedback on metrics they failed to pass, benchmarked by the performance of 8 experienced robotic surgeons (prior robotic surgery caseload >100) (Fig 1b). Automated performance metrics (APMs) were derived from the kinematics and system events data of the daVinci robotic system, representing efficiency and console manipulation competency. Robotic anastomosis competency evaluation (RACE) scores assess suturing technical skills. RACE scores were evaluated independently by =2 trained-assessors blinded to participants’ identity. Averaged scores were used for analysis. The intra-class coefficients (ICCs) were measured to monitor the inter-rater reliability. Metric improvement from baseline was compared between the FG and the CG by generalized linear mixed model.
Results: 23 participants were randomized to the FG (N=11) and the CG (N=12). The experience levels and baseline VUA metrics were comparable between groups. The ICC was moderately high for all RACE skill domains (ICCs>0.58, p<0.05). Overall, most metrics of the FG improved more than the CG (Fig 1c). Specifically in VUA tests, the total RACE scores of FG improved more than the CG at the mid-term VUA (mean, ?FG 4.5 vs ?CG 1.1, p=0.05). This difference remained but non-statistically significant in the final VUA (?FG 5.3 vs ?CG 4.9, p=0.78).
Conclusions: Customized feedback based on select APMs and RACE scores may expedite the acquisition of robotic suturing skills. This pilot study paves the way to larger randomized-controlled trials on the efficacy of feedback.
Source of Funding: This study was funded in part by an Intuitive Surgical Clinical Grant and the National Institute Of Biomedical Imaging And Bioengineering of the National Institutes of Health under Award Number K23EB026493.

.jpg)
.jpg)