Back
Poster, Podium & Video Sessions
Moderated Poster
MP41: Surgical Technology & Simulation: Training & Skills Assessment
MP41-14: The learning curve of radical nephrectomy for kidney cancer: implications for surgical training
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 228
Federico Belladelli*, Giuseppe Fallara, Giuseppe Rosiello, Daniele Cignoli, Giuseppe Basile, Gianmarco Colandrea, Giacomo Musso, Francesco Cei, Daniela Canibus, Walter Cazzaniga, Gianfranco Baiamonte, Chiara Re, Andrea Ieva, Milan, Italy, Pierre I. Karakiewicz, Montreal, Canada, Federico Dehò, Varese, Italy, Patrizio Rigatti, Giorgio Guazzoni, Milan, Italy, Andrea Gallina, Lugano, Switzerland, Alexandre Mottrie, Aalst, Belgium, Francesco Montorsi, Roberto Bertini, Andrea Salonia, Alberto Briganti, Umberto Capitanio, Alessandro Larcher, Milan, Italy
- FB
Poster Presenter(s)
Introduction: Experience (EXP) is a human factor that importantly affect surgery: the relationship between increasing surgical experience and better clinical outcomes defines the learning curve of a procedure. In this regard, no data are available with respect to radical nephrectomy (RN) for kidney cancer. The aim of the study was to investigate the effect of EXP on patient’s outcomes after RN
Methods: Patients treated with RN for a cT1-3a cN0 cM0 renal mass at one high-volume Institution by 15 surgeons were assessed into a prospective database. For each patient, EXP was defined as the total number of RN performed by each surgeon before the patient's operation. Primary outcomes of the study were all-cause mortality (ACM), clinical progression (CP) Clavien-Dindo =2 postoperative complications (CD=2) and estimated glomerular filtration rate [eGFR] at 12 months. Secondary outcome of the study was operative time (OT). Multivariable Cox (ACM, CP), logistic (CD=2) and linear regression (eGFR, OT) models tested the effect of EXP on the outcomes. Restricted cubic splines were used to test for the non-linear nature of the relationship between EXP and the outcomes. Covariates consisted of age, Charlson comorbidity index, preoperative eGFR, pathological tumour size, tumour grade, T-stage, N-stage, surgical approach and year of surgery to precisely account for case mix.
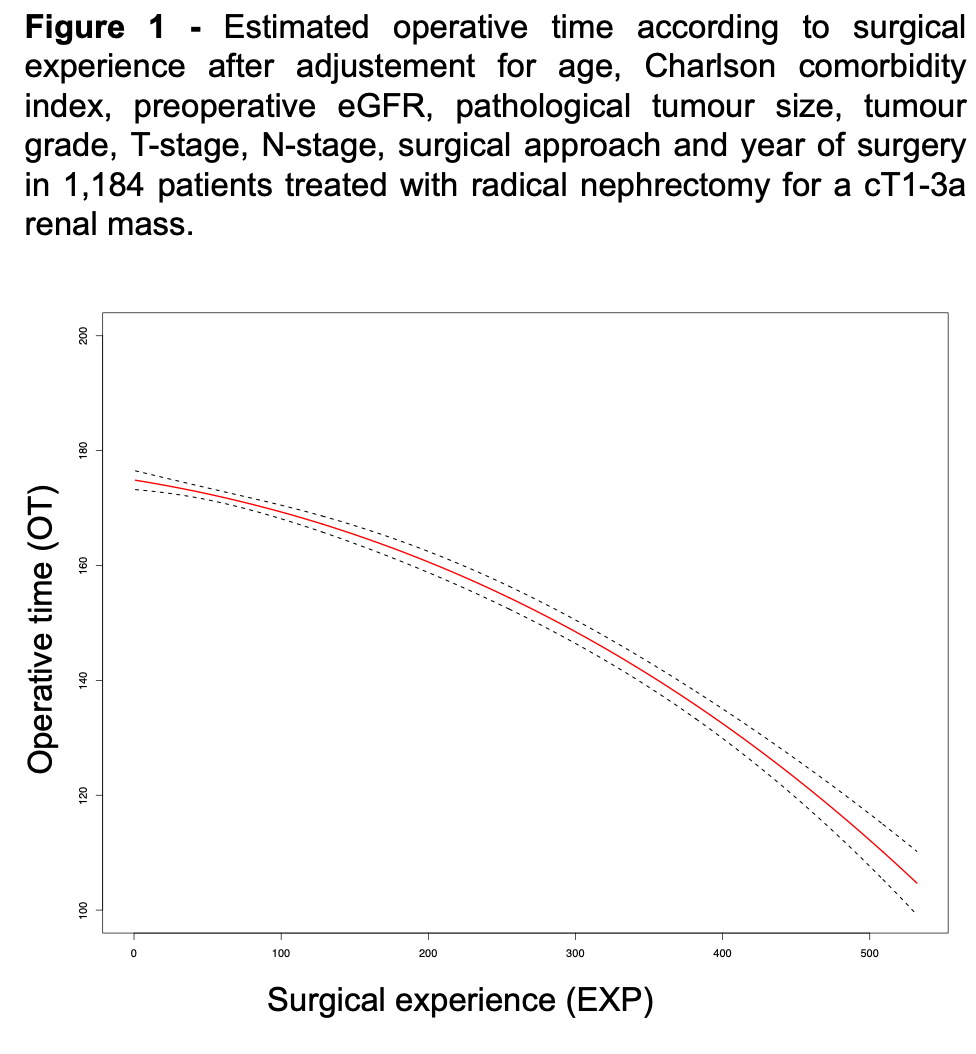
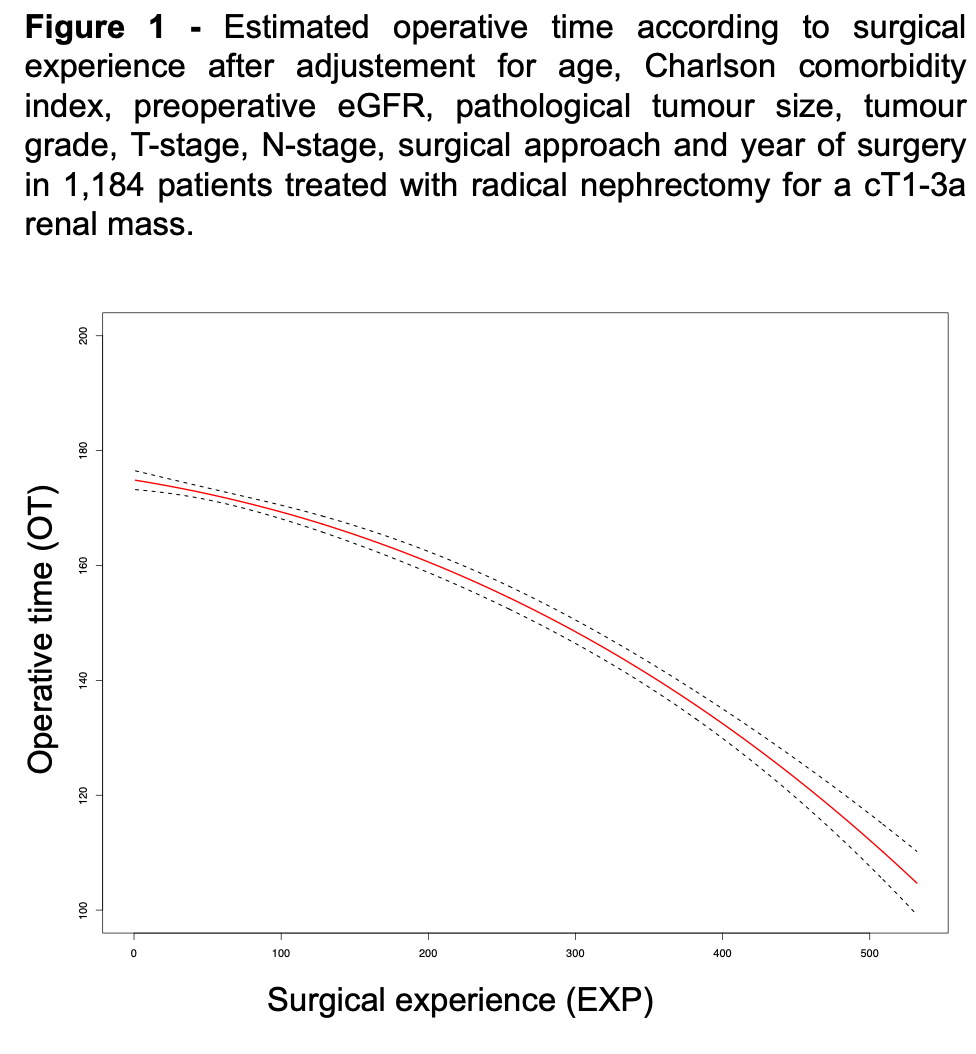
Results: Overall, 1,184 patients were evaluated. Median EXP was 60 cases (interquartile range [IQR] 26-146). After a medianfollow-up of 81 months, the 5-year rates of ACM and CP were 13 and 12%. The rate of CD=2 was 14%. The median 1-year eGFR was 56 mL/min/1.73m2 (IQR 47-68). At multivariable analyses, EXP was not associated with ACM (p=0.7), CP (p=0.2), CD=2 complications (p=0.6) and 12-months eGFR (p=0.9). Conversely, EXP was associated with lower estimated operative time (Estimate -0.9; 95% Confidence intervals -1.7 to -2.5; p<0.01; Figure 1)
Conclusions: EXP does not impact the risk of mortality, cancer control, morbidity or renal function impairment in candidates for RN, although experienced surgeons performed faster surgeries. The very large cohort examined, and the extensive follow-up support the validity of this negative findings. Kidney cancer patients elected for RN and treated by novices have the same clinical outcomes of those treated by experienced surgeons; hence RN represent an ideal scenario for surgical training, provided the planning of longer OT
Source of Funding: No
Methods: Patients treated with RN for a cT1-3a cN0 cM0 renal mass at one high-volume Institution by 15 surgeons were assessed into a prospective database. For each patient, EXP was defined as the total number of RN performed by each surgeon before the patient's operation. Primary outcomes of the study were all-cause mortality (ACM), clinical progression (CP) Clavien-Dindo =2 postoperative complications (CD=2) and estimated glomerular filtration rate [eGFR] at 12 months. Secondary outcome of the study was operative time (OT). Multivariable Cox (ACM, CP), logistic (CD=2) and linear regression (eGFR, OT) models tested the effect of EXP on the outcomes. Restricted cubic splines were used to test for the non-linear nature of the relationship between EXP and the outcomes. Covariates consisted of age, Charlson comorbidity index, preoperative eGFR, pathological tumour size, tumour grade, T-stage, N-stage, surgical approach and year of surgery to precisely account for case mix.
Results: Overall, 1,184 patients were evaluated. Median EXP was 60 cases (interquartile range [IQR] 26-146). After a medianfollow-up of 81 months, the 5-year rates of ACM and CP were 13 and 12%. The rate of CD=2 was 14%. The median 1-year eGFR was 56 mL/min/1.73m2 (IQR 47-68). At multivariable analyses, EXP was not associated with ACM (p=0.7), CP (p=0.2), CD=2 complications (p=0.6) and 12-months eGFR (p=0.9). Conversely, EXP was associated with lower estimated operative time (Estimate -0.9; 95% Confidence intervals -1.7 to -2.5; p<0.01; Figure 1)
Conclusions: EXP does not impact the risk of mortality, cancer control, morbidity or renal function impairment in candidates for RN, although experienced surgeons performed faster surgeries. The very large cohort examined, and the extensive follow-up support the validity of this negative findings. Kidney cancer patients elected for RN and treated by novices have the same clinical outcomes of those treated by experienced surgeons; hence RN represent an ideal scenario for surgical training, provided the planning of longer OT
Source of Funding: No

.jpg)
.jpg)