Back
Poster, Podium & Video Sessions
Moderated Poster
MP41: Surgical Technology & Simulation: Training & Skills Assessment
MP41-20: Cost-Effective and Readily Replicable Surgical Simulation Model Improves Trainee Performance in Urethrovesical Anastomosis
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 228
Stacy Jeong, Cleveland Heights, OH, Maxx Caveney*, Jacob Knorr, Rebecca Campbell, Daniel Santana, Christopher Weight, Nima Almassi, Steven Campbell, Cleveland, OH
- MC
Maxx Caveney, MD
MD
Glickman Urology and Kidney Institute
Poster Presenter(s)
Introduction: To develop a simple, cost-effective, and re-usable model for urethrovesical anastomosis for robotic-assisted radical prostatectomy and evaluate its impact on fundamental surgical skills and confidence of urology trainees.
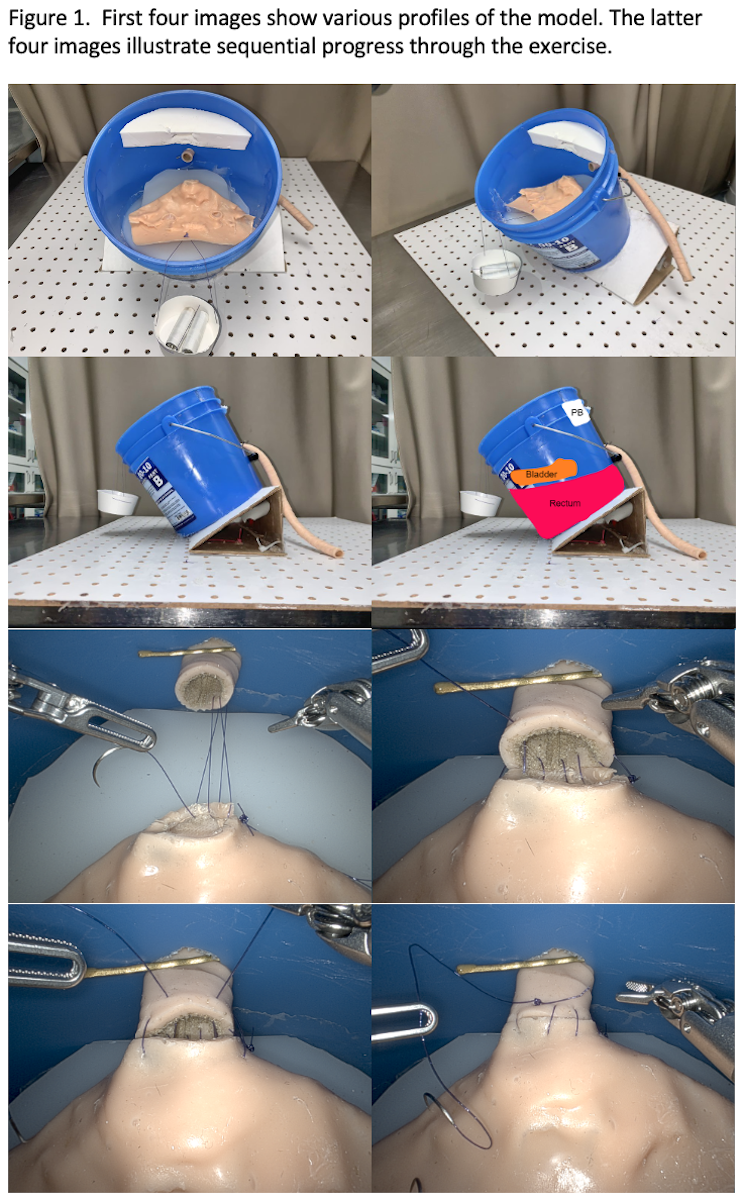
Methods: A model for the bladder, urethra, and bony pelvis was created from silicone using household materials. Each participant performed several trials of urethrovesical anastomosis using the da Vinci Si Surgical system. Pre-task confidence was assessed prior to each attempt. Two blinded researchers measured the following outcomes: time-to-anastomosis, number of suture throws, perpendicular needle entry, and atraumatic needle driving. Integrity of the anastomosis was determined by gravity filling and measuring the pressure at which leakage occurred. These outcomes were translated into an independently validated Prostatectomy Assessment Competency Evaluation (PACE) score.
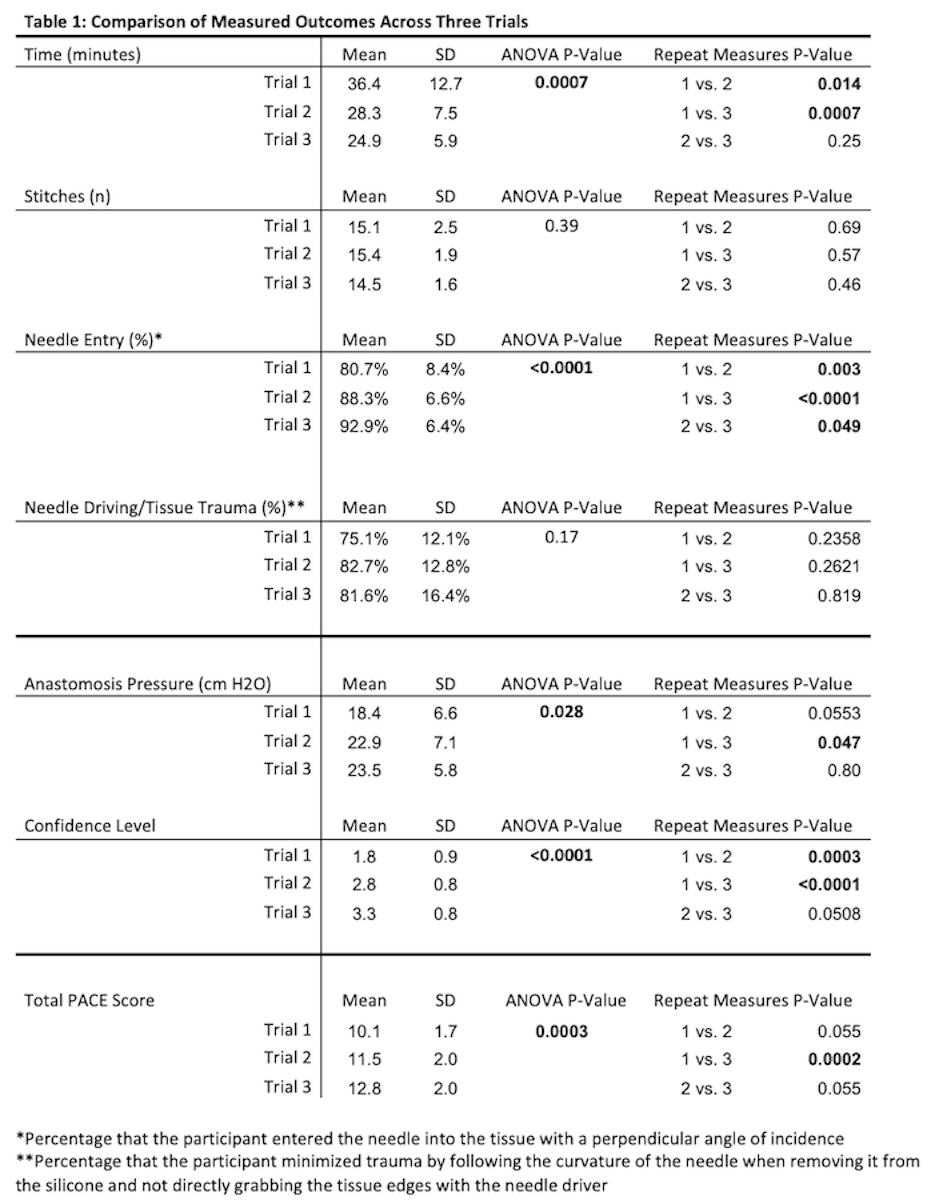
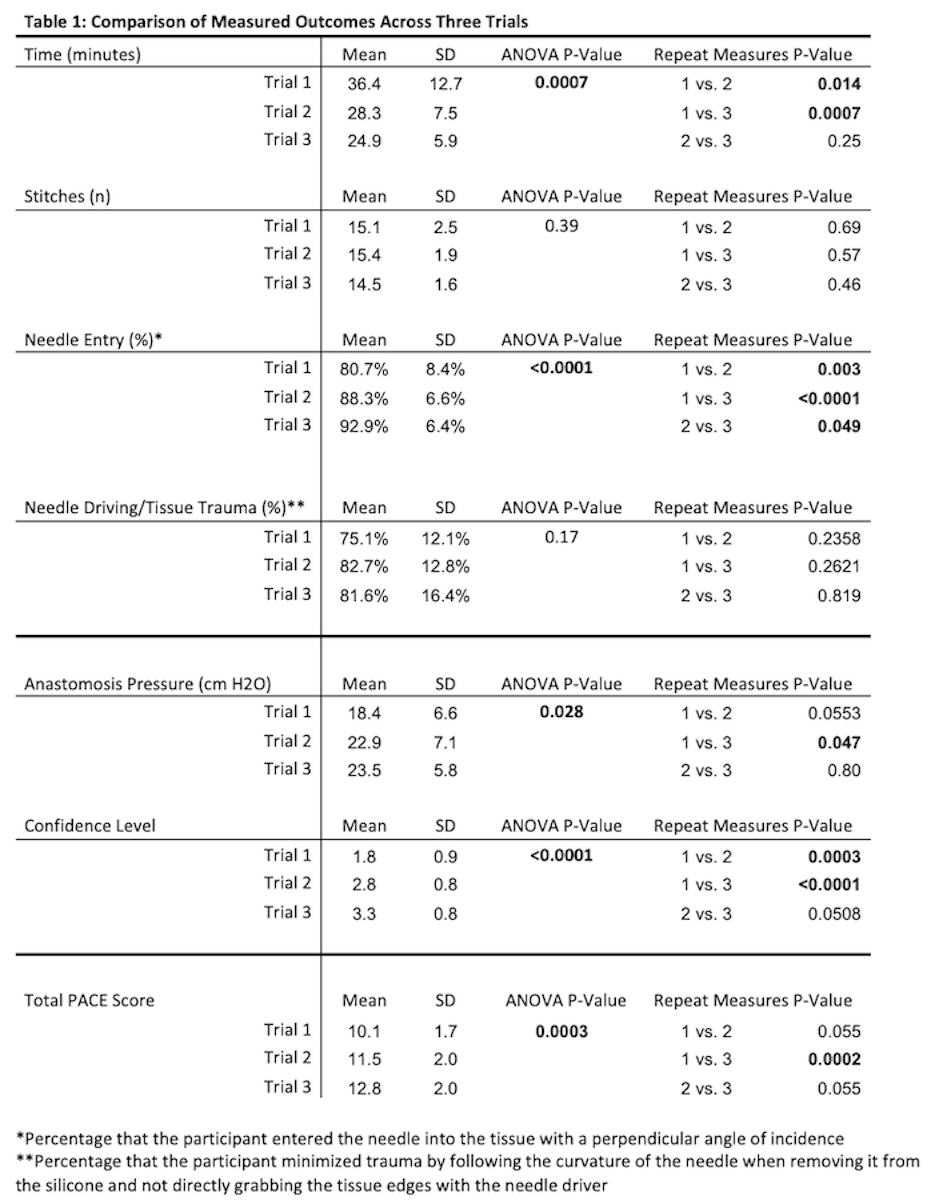
Results: The price of each model was 64 US dollars and took 2 hours to create. Twenty-one residents enrolled and demonstrated significant improvement in time-to-anastomosis, perpendicular needle driving, anastomotic pressure, and total PACE score between the first and third trial. Pre-task confidence was measured on a Likert scale (1-5) and improved significantly over the three trials (Likert scale of 1.8, 2.8, and 3.3).
Conclusions: We developed a cost-effective model of urethrovesical anastomosis that does not require the use of a 3-D printer. This study demonstrates significant improvement of fundamental surgical skills and validated surgical assessment score for urology trainees over several trials. Our model shows potential for increasing accessibility of robotic training models for urologic education. Additional investigation will be required to further confirm the validity of this model.
Source of Funding: N/A
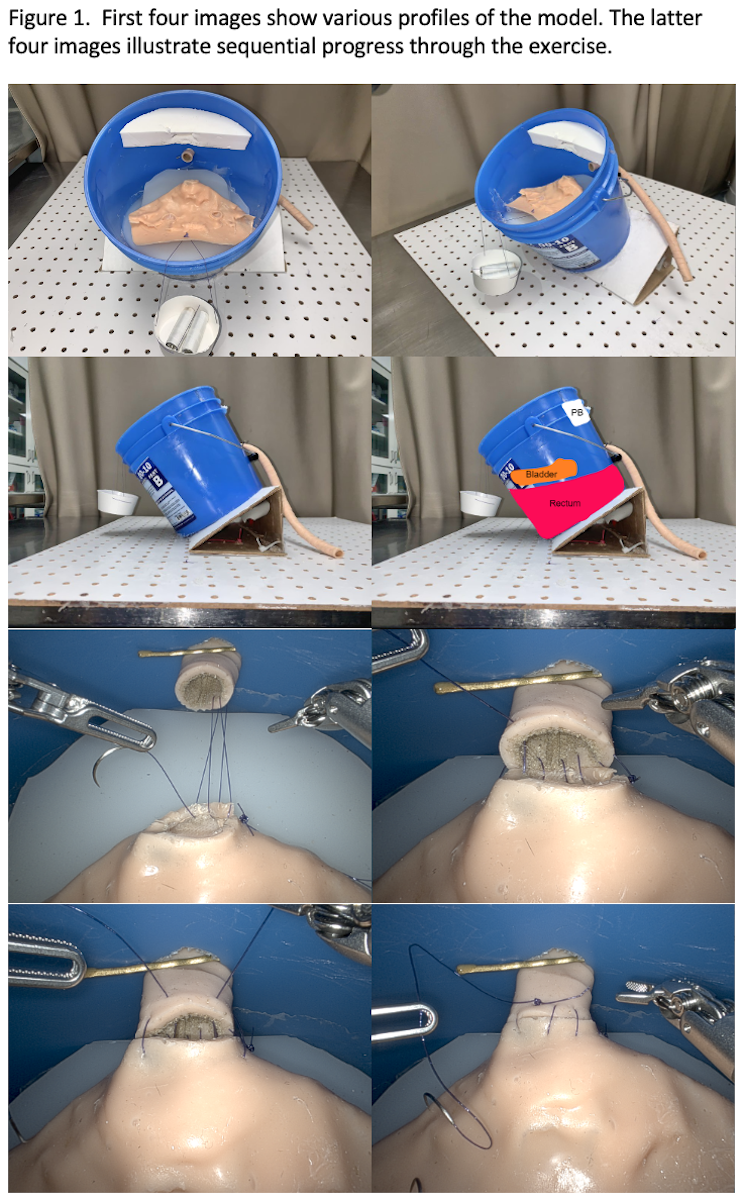
Methods: A model for the bladder, urethra, and bony pelvis was created from silicone using household materials. Each participant performed several trials of urethrovesical anastomosis using the da Vinci Si Surgical system. Pre-task confidence was assessed prior to each attempt. Two blinded researchers measured the following outcomes: time-to-anastomosis, number of suture throws, perpendicular needle entry, and atraumatic needle driving. Integrity of the anastomosis was determined by gravity filling and measuring the pressure at which leakage occurred. These outcomes were translated into an independently validated Prostatectomy Assessment Competency Evaluation (PACE) score.
Results: The price of each model was 64 US dollars and took 2 hours to create. Twenty-one residents enrolled and demonstrated significant improvement in time-to-anastomosis, perpendicular needle driving, anastomotic pressure, and total PACE score between the first and third trial. Pre-task confidence was measured on a Likert scale (1-5) and improved significantly over the three trials (Likert scale of 1.8, 2.8, and 3.3).
Conclusions: We developed a cost-effective model of urethrovesical anastomosis that does not require the use of a 3-D printer. This study demonstrates significant improvement of fundamental surgical skills and validated surgical assessment score for urology trainees over several trials. Our model shows potential for increasing accessibility of robotic training models for urologic education. Additional investigation will be required to further confirm the validity of this model.
Source of Funding: N/A

.jpg)
.jpg)