Back
Poster, Podium & Video Sessions
Moderated Poster
MP42: Bladder Cancer: Epidemiology & Evaluation II
MP42-01: Comparison of Microscopic Hematuria Incidence and Grade Between Microscopic and IRIS&[trade] Automated Urinalysis Methods
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 225
Aleem Khan*, Jani Alkesh, Mark Sawyer, Denver, CO
- AK
Aleem Khan, MD
Resident
Poster Presenter(s)
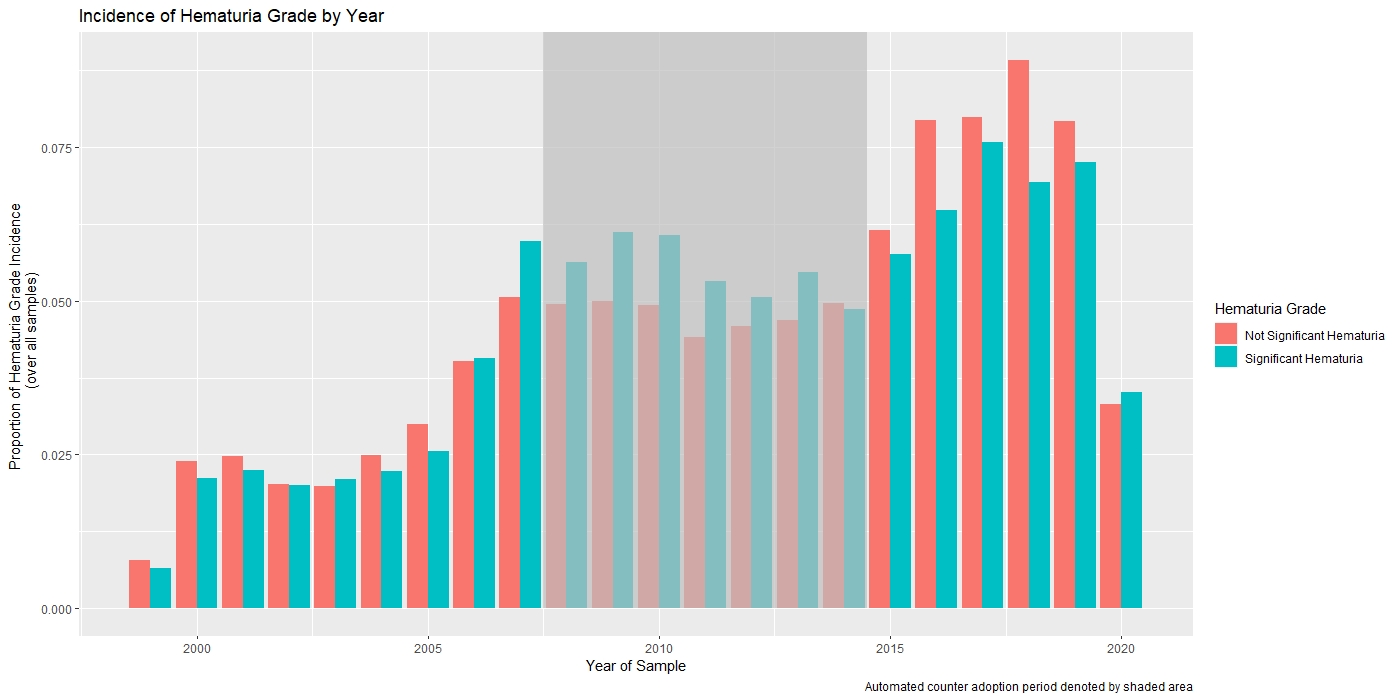
Introduction: Our VA facility first introduced an Iris™ automated urinalysis (UA) system in 2009. Since 2014, automated UA has been the primary method of reporting microscopic hematuria (MH). Our laboratory director was critical of the 2012 AUA guidelines for traditional microscopic specimen analysis, stating the described methodology was not reproducible and inferior to automated methods. In 2018, an email survey was sent to 30 VA facilities, with 29 (97%) reporting use of automated UAs primarily. Unfortunately, the 2020 AUA guidelines provide no guidance on automated UAs. The intent of this study is to determine if rates and severity of MH changed with the switch to automated methods.
Methods: In an IRB approved study, all UAs at our facility (1999-2021) were obtained. Of patients with reported “microscopic” results, only UAs that were nitrite and leukocyte negative were included. For any given patient, the first UA each year that met these criteria was selected. MH grade was categorized by RBCs/HPF as: “Negative” ( <3), Low (3-9), Intermediate (10-19), or High (>=20). Proportions per year was calculated by ratio of samples with at least low grade (LG) isolated MH to total UA tests (excluding ineligible or multiple patient tests). Cohorts of UAs performed before initial adoption of automated methods (until 12/2008) and after complete adoption of automated UAs (from 1/2014 onward) were compared.
Results: Of 1,048,575 total tests, 90,898 met selection criteria across both time periods (119,026 patients). The overall ratio of patients with significant MH decreased by a relatively small, but statistically significant, amount after switching to automated UAs. The percentage of significant MH (at least LG) was 40.6% through 2008 vs. 38.3% since 2014 (p < 0.001). Rates of intermediate or high-grade MH were 20.3% and 19.1%, respectively (p=0.003).
Conclusions: Automated UA appears to diagnose significant MH at a rate only 2.3% lower than microscopic specimen analysis. Automated UAs have various advantages relative to traditional microscopy, which is no longer routine practice for many laboratories. The relatively small difference in MH diagnosis suggests that future guidelines can accept automated UAs as being a valid alternative.
Source of Funding: None
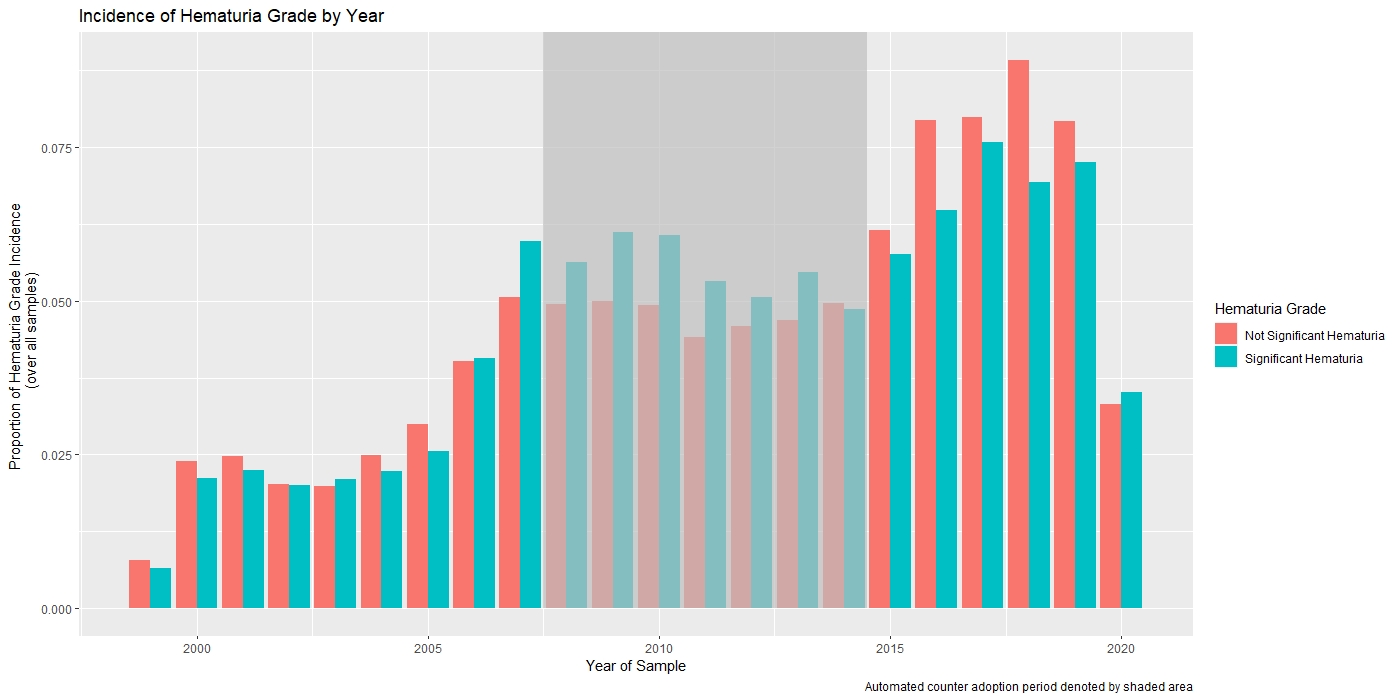
Methods: In an IRB approved study, all UAs at our facility (1999-2021) were obtained. Of patients with reported “microscopic” results, only UAs that were nitrite and leukocyte negative were included. For any given patient, the first UA each year that met these criteria was selected. MH grade was categorized by RBCs/HPF as: “Negative” ( <3), Low (3-9), Intermediate (10-19), or High (>=20). Proportions per year was calculated by ratio of samples with at least low grade (LG) isolated MH to total UA tests (excluding ineligible or multiple patient tests). Cohorts of UAs performed before initial adoption of automated methods (until 12/2008) and after complete adoption of automated UAs (from 1/2014 onward) were compared.
Results: Of 1,048,575 total tests, 90,898 met selection criteria across both time periods (119,026 patients). The overall ratio of patients with significant MH decreased by a relatively small, but statistically significant, amount after switching to automated UAs. The percentage of significant MH (at least LG) was 40.6% through 2008 vs. 38.3% since 2014 (p < 0.001). Rates of intermediate or high-grade MH were 20.3% and 19.1%, respectively (p=0.003).
Conclusions: Automated UA appears to diagnose significant MH at a rate only 2.3% lower than microscopic specimen analysis. Automated UAs have various advantages relative to traditional microscopy, which is no longer routine practice for many laboratories. The relatively small difference in MH diagnosis suggests that future guidelines can accept automated UAs as being a valid alternative.
Source of Funding: None

.jpg)
.jpg)