Back
Poster, Podium & Video Sessions
Moderated Poster
MP42: Bladder Cancer: Epidemiology & Evaluation II
MP42-12: Higher Preoperative eGFR is a Predictor of Worse Renal Function Decline After Robotic Assisted Radical Cystectomy
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 225
Shirin Razdan*, Benjamin Eilender, John Pfail, Mariely Garcia, Daniel Ranti, Shoshana Rosenzweig, New York, NY, Abolfazl Hosseini, Jari Radros, Stockholm, Sweden, Reza Mehrazin, Peter Wiklund, John Sfakianos, New York, NY
- SR
Shirin Razdan, MD
Icahn School of Medicine at The Mount Sinai Hospital
Poster Presenter(s)
Introduction: In patients with muscle invasive bladder cancer or high risk noninvasive bladder cancer, renal function decline is a concern after radical cystectomy with urinary diversion. The pathophysiology of this decline is multifactorial, with subclinical acidosis and metabolic derangements from the diversion thought to contribute. It is unknown whether patients with baseline chronic kidney disease (CKD) are at increased risk of further decline in renal function.
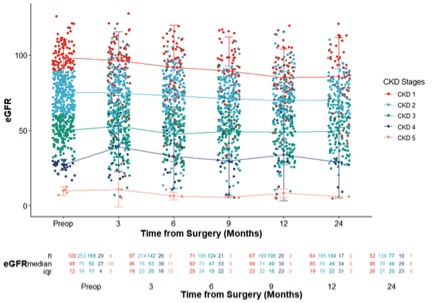
Methods: We performed a retrospective review of two high volume robotic assisted radical cystectomy (RARC) centers between 2016-2020. Preoperative demographics and comorbidities were collected. Postoperative estimated glomerular filtration rate (eGFR) was calculated at 12 and 24 months to determine short-term rate in decline of eGFR. Absolute and percent changes in eGFR were calculated.
Results: There were a total of 555 patients who underwent RARC. Men comprised 76.2% of the cohort. Neoadjuvant chemotherapy was given in 31% of patients and adjuvant chemotherapy was given in 4.81% of patients. Higher preoperative eGFR (B -0.549, 95% CI -0.708 - -0.391, p<0.001) and presence of diabetes mellitus (B -15.414, 95% CI -24.820- -6.008, p=0.001) were significant predictors of eGFR decline at 12 months. At 24 months, presence of diabetes mellitus (B -11.799, 95% CI -21.816 - -1.782, p=0.021) and higher preoperative eGFR (B -0.621, 95% CI -0.796 - -0.446, p<0.001) were correlated with a steeper decline in eGFR. Higher preoperative eGFR was also predictive of upstaging to CKD3 or higher post operatively (OR 1.019, 95% CI 1.004-1.034, p=0.015). Intracorporeal diversion was protective, whereas presence of hypertension, diabetes mellitus, and higher preoperative eGFR predicted greater decline in eGFR.
Conclusions: Patients with higher preoperative eGFR and diabetes are at increased risk of renal function decline post RARC at 12 and 24 months. This suggests that patients with risk factors for renal function decline, but otherwise normal renal function at baseline, are a particularly vulnerable population for progression to CKD after RARC and should be counseled and closely followed postoperatively for renal function deterioration.
Source of Funding: None
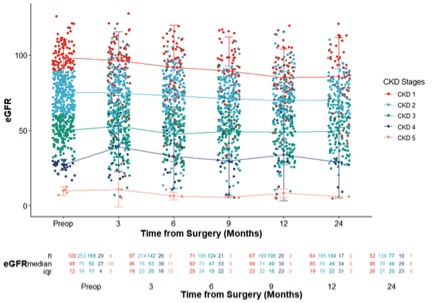
Methods: We performed a retrospective review of two high volume robotic assisted radical cystectomy (RARC) centers between 2016-2020. Preoperative demographics and comorbidities were collected. Postoperative estimated glomerular filtration rate (eGFR) was calculated at 12 and 24 months to determine short-term rate in decline of eGFR. Absolute and percent changes in eGFR were calculated.
Results: There were a total of 555 patients who underwent RARC. Men comprised 76.2% of the cohort. Neoadjuvant chemotherapy was given in 31% of patients and adjuvant chemotherapy was given in 4.81% of patients. Higher preoperative eGFR (B -0.549, 95% CI -0.708 - -0.391, p<0.001) and presence of diabetes mellitus (B -15.414, 95% CI -24.820- -6.008, p=0.001) were significant predictors of eGFR decline at 12 months. At 24 months, presence of diabetes mellitus (B -11.799, 95% CI -21.816 - -1.782, p=0.021) and higher preoperative eGFR (B -0.621, 95% CI -0.796 - -0.446, p<0.001) were correlated with a steeper decline in eGFR. Higher preoperative eGFR was also predictive of upstaging to CKD3 or higher post operatively (OR 1.019, 95% CI 1.004-1.034, p=0.015). Intracorporeal diversion was protective, whereas presence of hypertension, diabetes mellitus, and higher preoperative eGFR predicted greater decline in eGFR.
Conclusions: Patients with higher preoperative eGFR and diabetes are at increased risk of renal function decline post RARC at 12 and 24 months. This suggests that patients with risk factors for renal function decline, but otherwise normal renal function at baseline, are a particularly vulnerable population for progression to CKD after RARC and should be counseled and closely followed postoperatively for renal function deterioration.
Source of Funding: None

.jpg)
.jpg)