Back
Poster, Podium & Video Sessions
Moderated Poster
MP42: Bladder Cancer: Epidemiology & Evaluation II
MP42-13: Pelvic Lymphadenectomy for Bladder Cancer: Does a Thorough Dissection Still Matter?
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 225
Arnav Srivastava*, Hiren Patel, Kevin Chua, Sai Krishnaraya Doppalapudi, Akshay Thaper, Sammy Elsamra, New Brunswick, NJ, Isaac Kim, New Haven, CT, Eric Singer, Thomas Jang, Saum Ghodoussipour, New Brunswick, NJ

Arnav Srivastava, MD, MPH
Rutgers Robert Wood Johnson University Hospital, Rutgers Cancer Institute of New Jersey
Poster Presenter(s)
Introduction: Pelvic lymphadenectomy (PLND) alongside radical cystectomy (RC), provides crucial diagnostic and therapeutic value in bladder cancer patients. With the advent of neoadjuvant chemotherapy and prospective data supporting standard PLND, controversy remains regarding the optimal PLND and who should receive it. Nearly 40% of patients may not receive adequate PLND, even though 25% of patients may have positive lymph nodes (LN) at time of RC. To clarify the importance of PLND, we propose a retrospective investigation of a low-risk patient group (pTanyN0M0) undergoing RC.
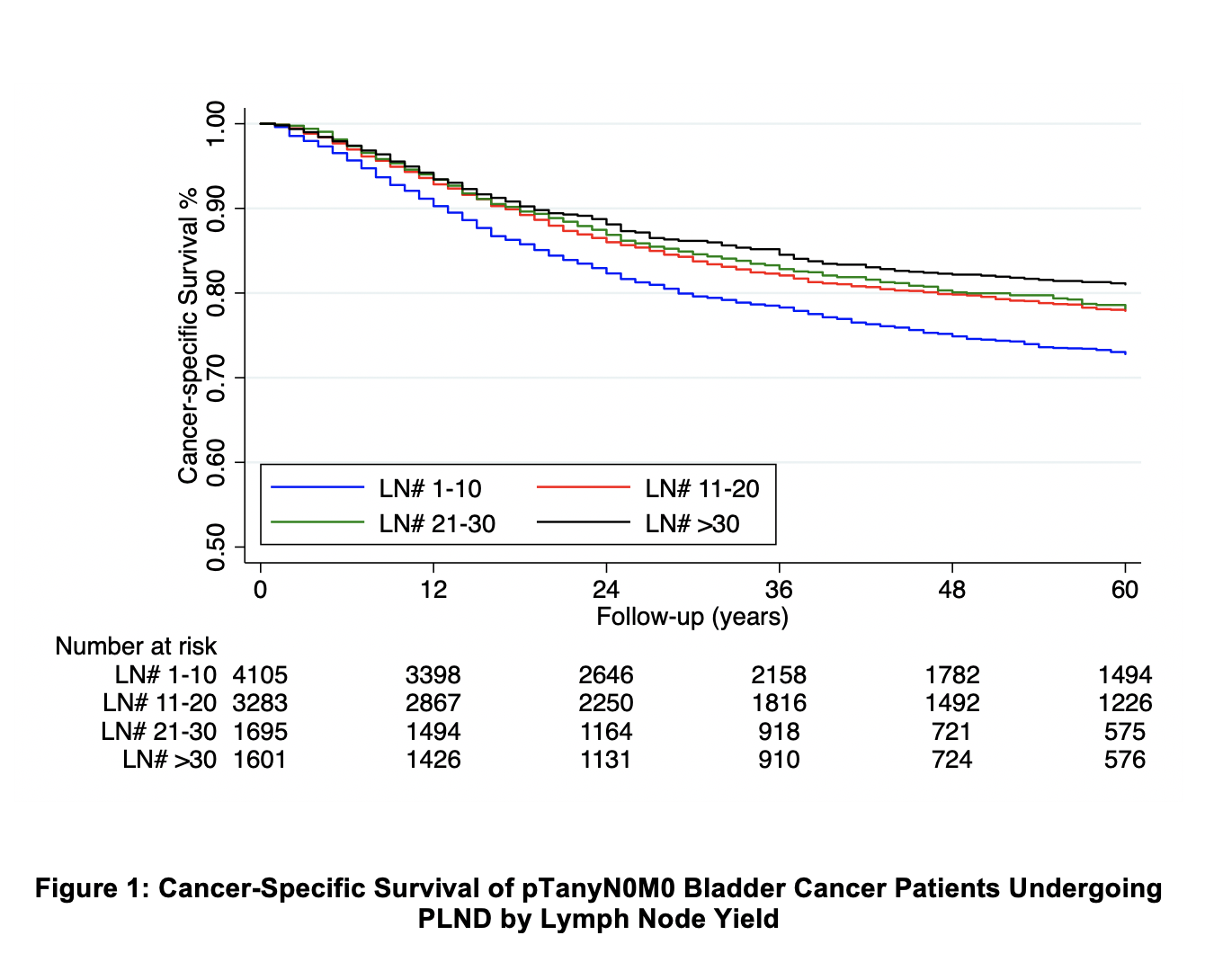
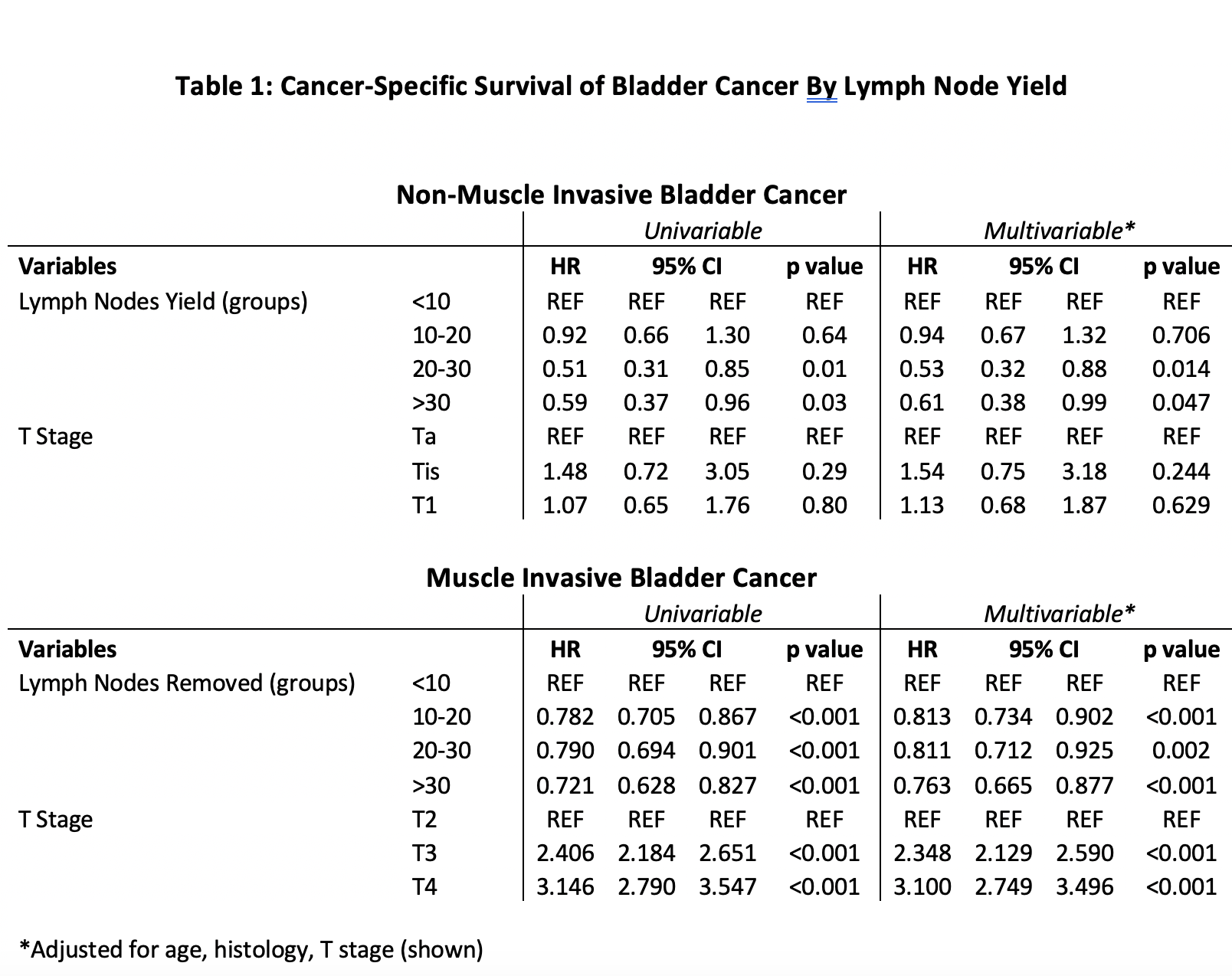
Methods: From the Surveillance, Epidemiology, and End Results (SEER) program, we identified pTanyN0M0 bladder cancer patients undergoing RC from 2004 – 2016. Kaplan Meier curves and Cox proportional hazards models assessed cancer-specific survival (CSS). Patients were analyzed with PLND performed as the primary covariate. Survival analysis then stratified patients undergoing PLND by LN yield (1-10, 11-20, 20-30, and >30 LN) and T stage.
Results: 13,179 patients met inclusion criteria with median follow up of 38 (IQR:17 – 77) months. PLND was performed in 81.21% of patients with a median LN yield of 14 (IQR: 7 – 23). Most commonly, patients had T2 disease (43.77%) and 91.78% had urothelial histology. After controlling for age, T stage, and histology, patients receiving PLND had improved CSS (HR 0.58, 95%CI 0.53 – 0.63). When grouping patients by LN yield, survival improved in a “dose dependent” manner (>30 LN HR 0.75, 95%CI 0.66 – 0.86) (Figure 1). We noted similar results when stratifying patients into non-muscle invasive and muscle-invasive bladder cancer (Table 1).
Conclusions: In a large contemporary series of pTanyN0M0 bladder cancer patients, we found a significant oncologic benefit to PLND. More extensive PLND correlated to improved CSS in non-muscle invasive and muscle invasive disease. Our data support the possibility of occult micro-metastasis – even in non-muscle invasive disease. Additionally, our results emphasize the importance of a thorough PLND for optimal oncologic control.
Source of Funding: NCI (P30CA072720).
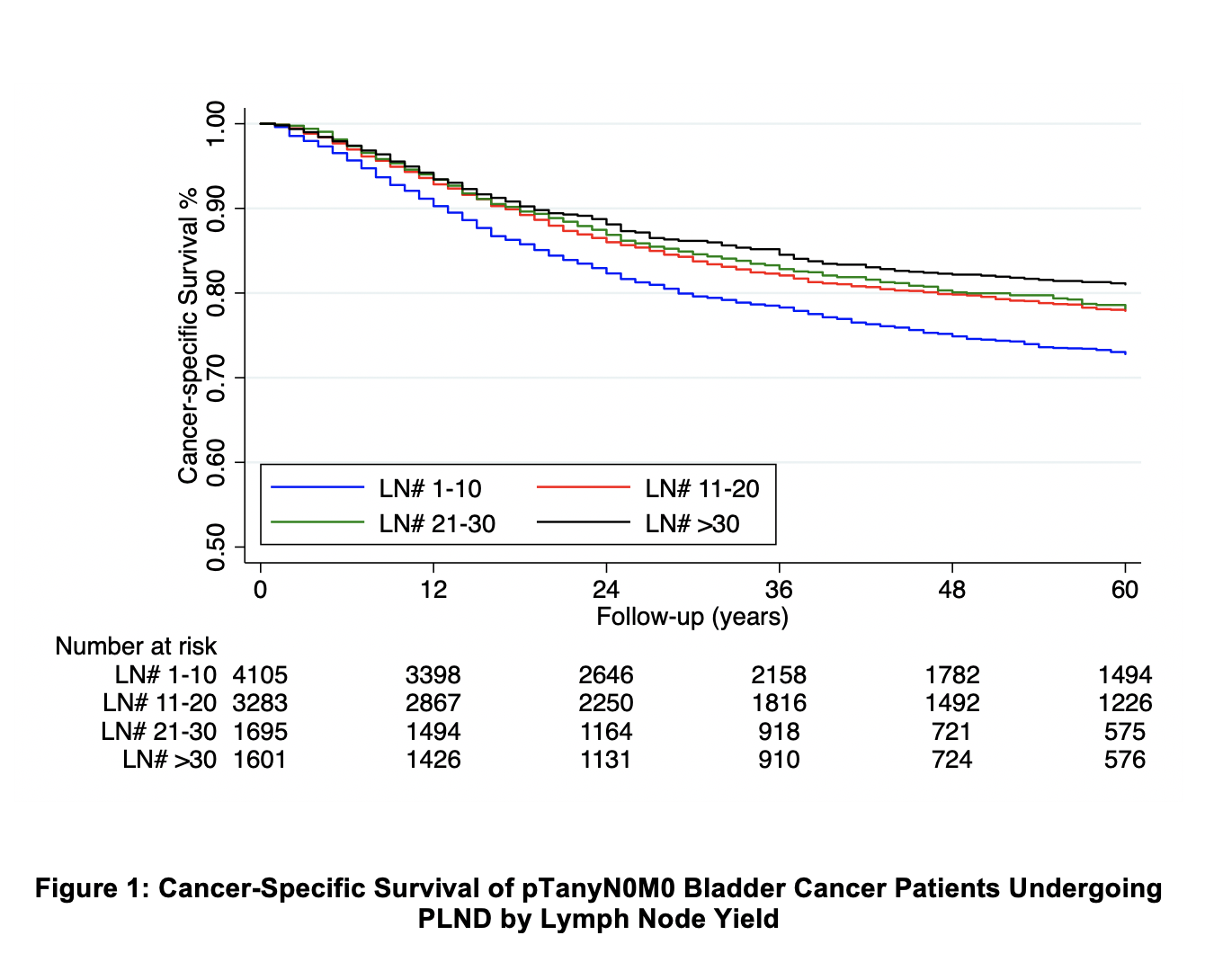
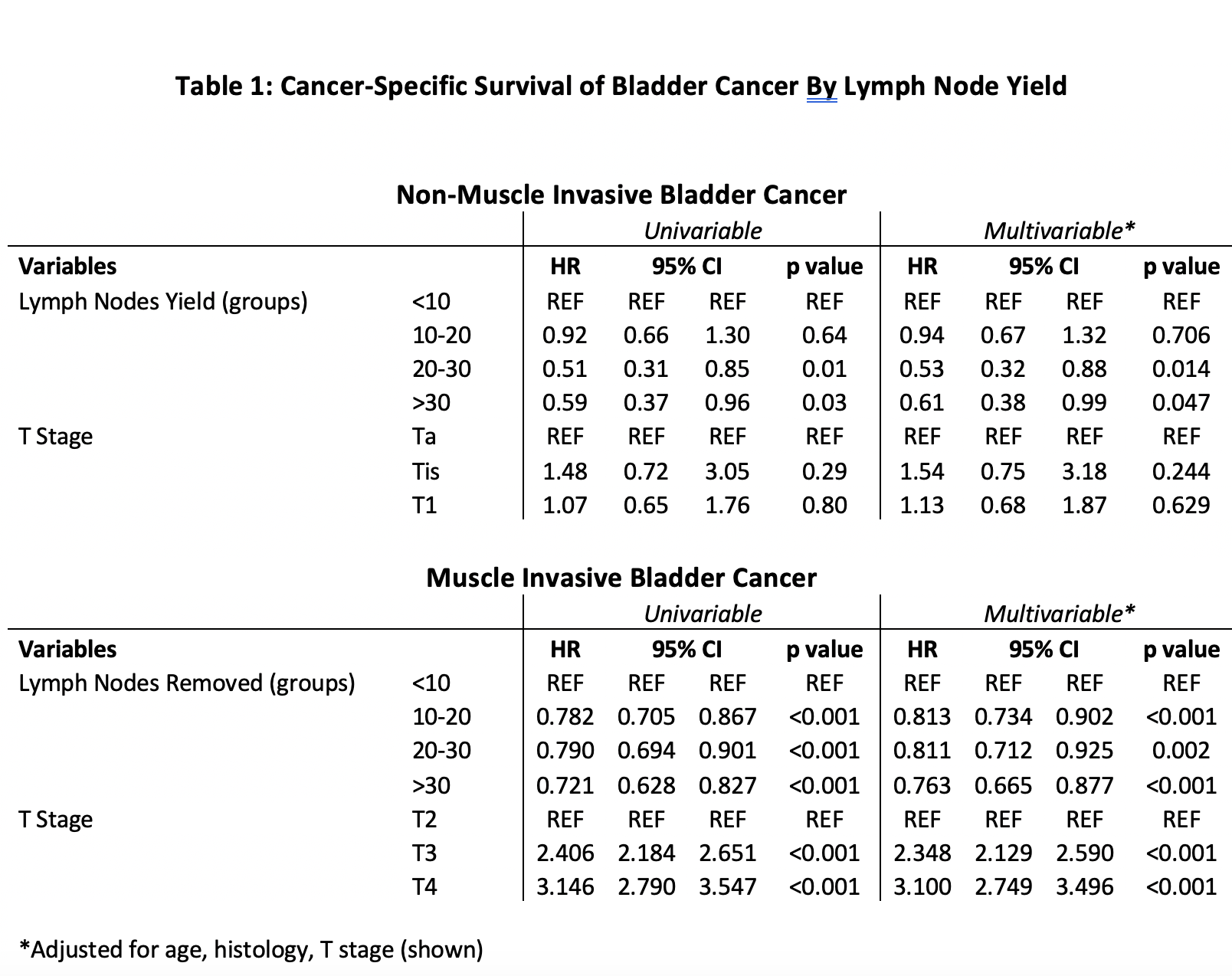
Methods: From the Surveillance, Epidemiology, and End Results (SEER) program, we identified pTanyN0M0 bladder cancer patients undergoing RC from 2004 – 2016. Kaplan Meier curves and Cox proportional hazards models assessed cancer-specific survival (CSS). Patients were analyzed with PLND performed as the primary covariate. Survival analysis then stratified patients undergoing PLND by LN yield (1-10, 11-20, 20-30, and >30 LN) and T stage.
Results: 13,179 patients met inclusion criteria with median follow up of 38 (IQR:17 – 77) months. PLND was performed in 81.21% of patients with a median LN yield of 14 (IQR: 7 – 23). Most commonly, patients had T2 disease (43.77%) and 91.78% had urothelial histology. After controlling for age, T stage, and histology, patients receiving PLND had improved CSS (HR 0.58, 95%CI 0.53 – 0.63). When grouping patients by LN yield, survival improved in a “dose dependent” manner (>30 LN HR 0.75, 95%CI 0.66 – 0.86) (Figure 1). We noted similar results when stratifying patients into non-muscle invasive and muscle-invasive bladder cancer (Table 1).
Conclusions: In a large contemporary series of pTanyN0M0 bladder cancer patients, we found a significant oncologic benefit to PLND. More extensive PLND correlated to improved CSS in non-muscle invasive and muscle invasive disease. Our data support the possibility of occult micro-metastasis – even in non-muscle invasive disease. Additionally, our results emphasize the importance of a thorough PLND for optimal oncologic control.
Source of Funding: NCI (P30CA072720).

.jpg)
.jpg)