Back
Poster, Podium & Video Sessions
Moderated Poster
MP42: Bladder Cancer: Epidemiology & Evaluation II
MP42-17: Conditional Survival Following Radical Cystectomy for Urothelial Carcinoma of the Bladder
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 225
Maria F. Moreno*, Sumedh Kaul, Aaron Fleishman, Ruslan Korets, Peter Chang, Andrew Wagner, Boston, MA, Simon Kim, Aurora, CO, Joaquim Bellmunt, Irving Kaplan, Aria F. Olumi, Boris Gershman, Boston, MA
Poster Presenter(s)
Introduction: Traditional surveillance protocols do not adequately account for the decreasing risk of mortality over time in aggressive malignancies, such as bladder cancer. Rather, the risk of death depends on both the baseline risk of mortality and the time survived since treatment. We therefore evaluated the conditional survival of patients with urothelial carcinoma of the bladder (UCB) following radical cystectomy (RC).
Methods: We identified patients aged 18-75 with Charlson 0-1 and pTany pN0-3 cM0 UCB diagnosed from 2006-2015 in the National Cancer Database and treated with RC. The 2- and 5-year conditional overall survival (COS) – i.e., the probability of surviving an additional 2- or 5-years given a specified time survived since treatment – were estimated using the Kaplan-Meier method. Multivariable Cox regression models with landmark time analysis were used to evaluate the associations of baseline characteristics with OS over time.
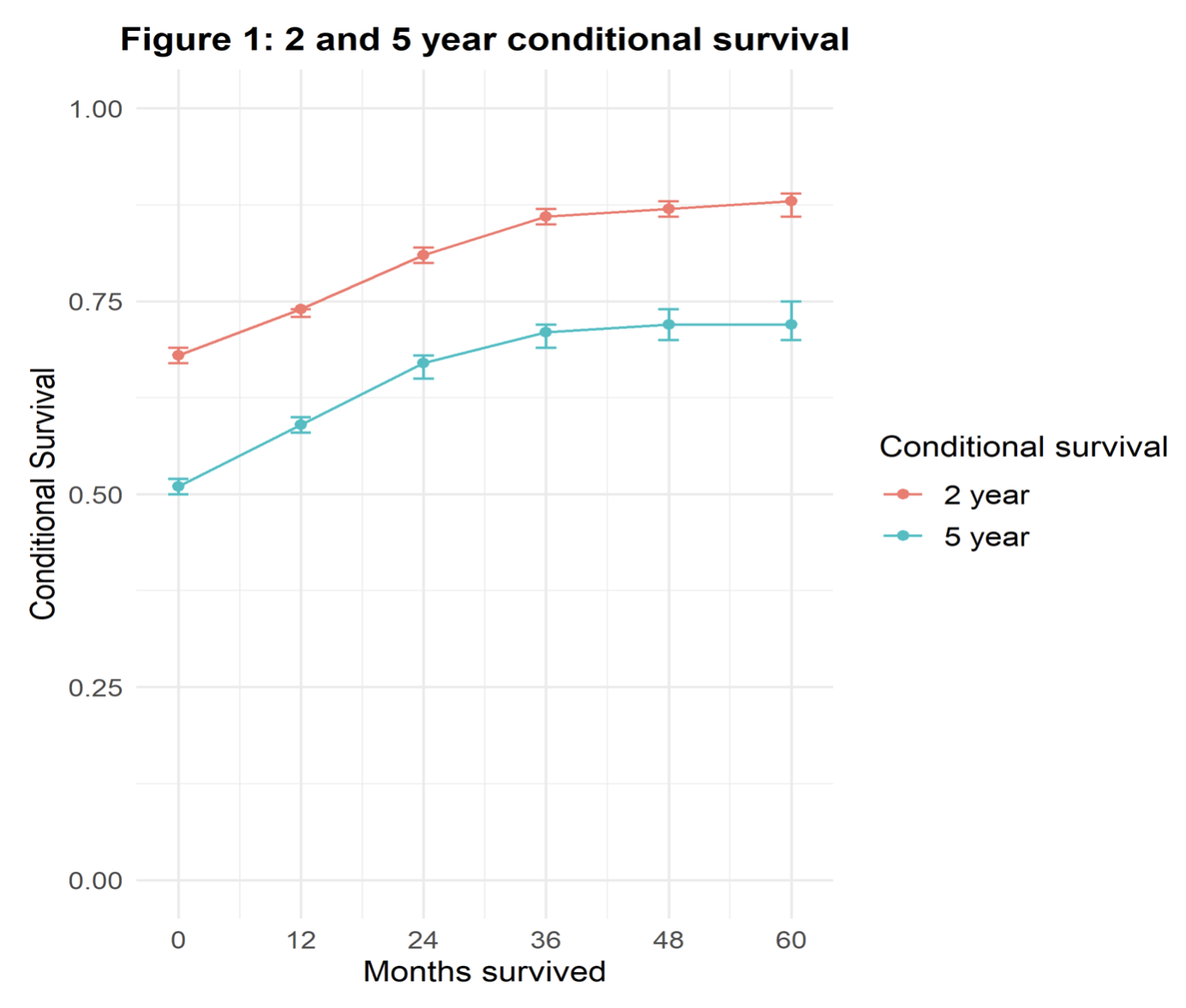
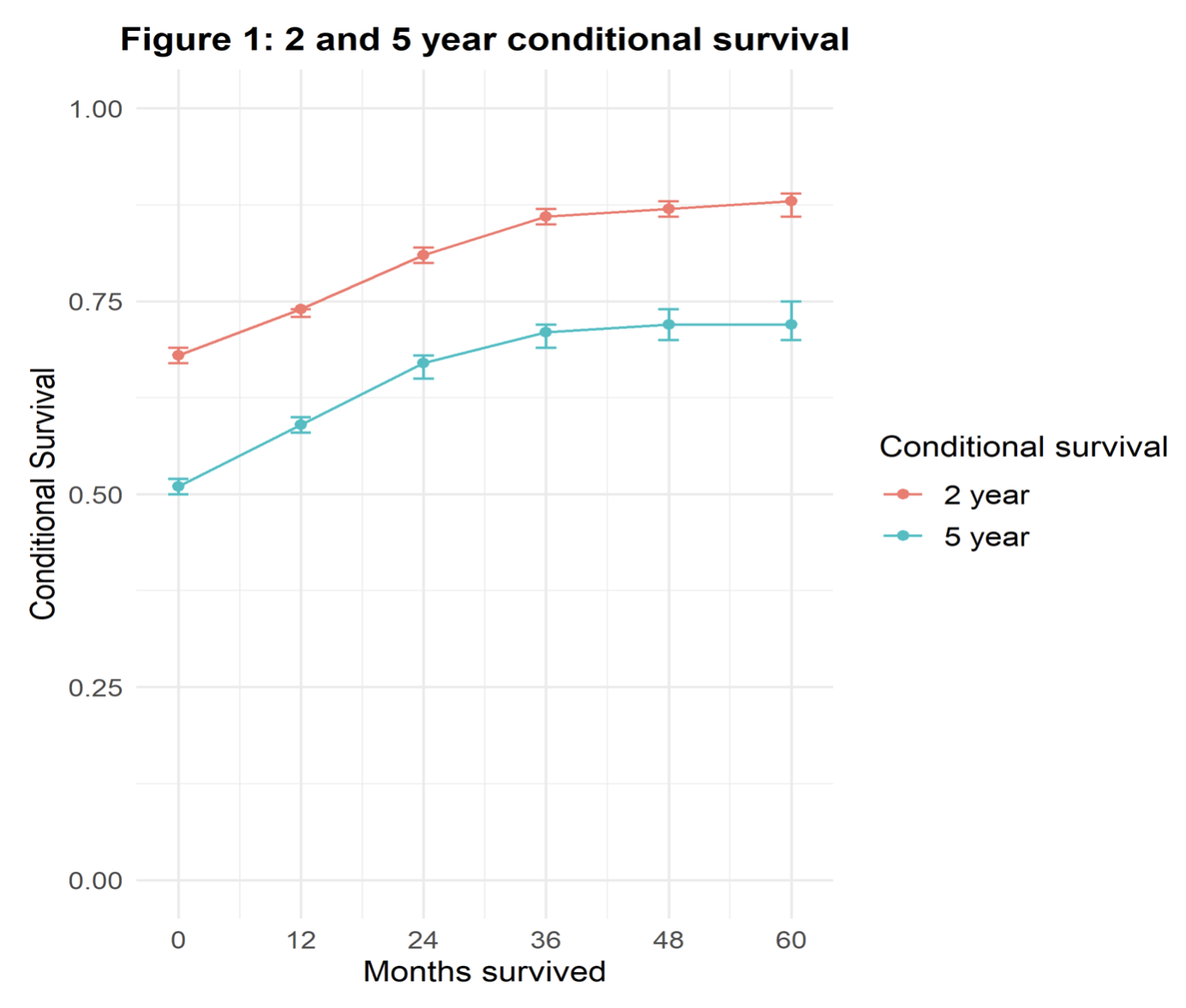
Results: A total of 15,594 patients were included in the study. Median follow-up was 27.8 months. The 2- and 5-year COS for the overall cohort increased through 36 months follow-up and then plateaued (Figure 1). When stratified by pT and pN stage, the COS gain increased with higher pTN stage, demonstrating the greatest increase over time for patients with pTany N1-3 disease (5-year COS of 23% at baseline, 58% at 36-months, and 71% at 60-months; Figure 2). In multivariable Cox regression modelling, pT and pN stage were significantly associated with higher all-cause mortality at baseline (HR 3.27 for pT4, HR 2.57 for pT3 vs =pT2; HR 2.26 for pN2-3, HR 1.77 for pN1 vs pN0), but these associations were attenuated in magnitude with increasing landmark times of 36- and 60-months (HR 1.63 for pT4, HR 1.35 for pT3 vs =pT2; HR 1.34 for pN2-3, HR 1.27 for pN1 vs pN0).
Conclusions: Risk of death after RC varies with time elapsed since treatment and disease stage. Accordingly, stage-specific COS may be used to improve prognostication and surveillance protocols.
Source of Funding: None

Methods: We identified patients aged 18-75 with Charlson 0-1 and pTany pN0-3 cM0 UCB diagnosed from 2006-2015 in the National Cancer Database and treated with RC. The 2- and 5-year conditional overall survival (COS) – i.e., the probability of surviving an additional 2- or 5-years given a specified time survived since treatment – were estimated using the Kaplan-Meier method. Multivariable Cox regression models with landmark time analysis were used to evaluate the associations of baseline characteristics with OS over time.
Results: A total of 15,594 patients were included in the study. Median follow-up was 27.8 months. The 2- and 5-year COS for the overall cohort increased through 36 months follow-up and then plateaued (Figure 1). When stratified by pT and pN stage, the COS gain increased with higher pTN stage, demonstrating the greatest increase over time for patients with pTany N1-3 disease (5-year COS of 23% at baseline, 58% at 36-months, and 71% at 60-months; Figure 2). In multivariable Cox regression modelling, pT and pN stage were significantly associated with higher all-cause mortality at baseline (HR 3.27 for pT4, HR 2.57 for pT3 vs =pT2; HR 2.26 for pN2-3, HR 1.77 for pN1 vs pN0), but these associations were attenuated in magnitude with increasing landmark times of 36- and 60-months (HR 1.63 for pT4, HR 1.35 for pT3 vs =pT2; HR 1.34 for pN2-3, HR 1.27 for pN1 vs pN0).
Conclusions: Risk of death after RC varies with time elapsed since treatment and disease stage. Accordingly, stage-specific COS may be used to improve prognostication and surveillance protocols.
Source of Funding: None


.jpg)
.jpg)
