Back
Poster, Podium & Video Sessions
Moderated Poster
MP43: Prostate Cancer: Localized: Active Surveillance
MP43-01: Clinical Significance of Detection of Perineural Invasion in Low-risk men on Active Surveillance
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 222
Claire de la Calle*, Mufaddal Mamawala, Patricia Landis, Jonathan Epstein, Bruce Trock, Ballentine Carter, Christian Pavlovich, Baltimore, MD
- CD
Claire M. De La Calle, MD
Johns Hopkins Univeristy
Poster Presenter(s)
Introduction: Perineural Invasion (PNI) is a well described mechanism of extracapsular tumor growth in prostate cancer (PCa). The clinical significance of PNI is unclear however, especially when noted on biopsy in patients with low-risk PCa considering active surveillance (AS). Here we aimed to evaluate the clinical significance of PNI in a cohort of men on AS.
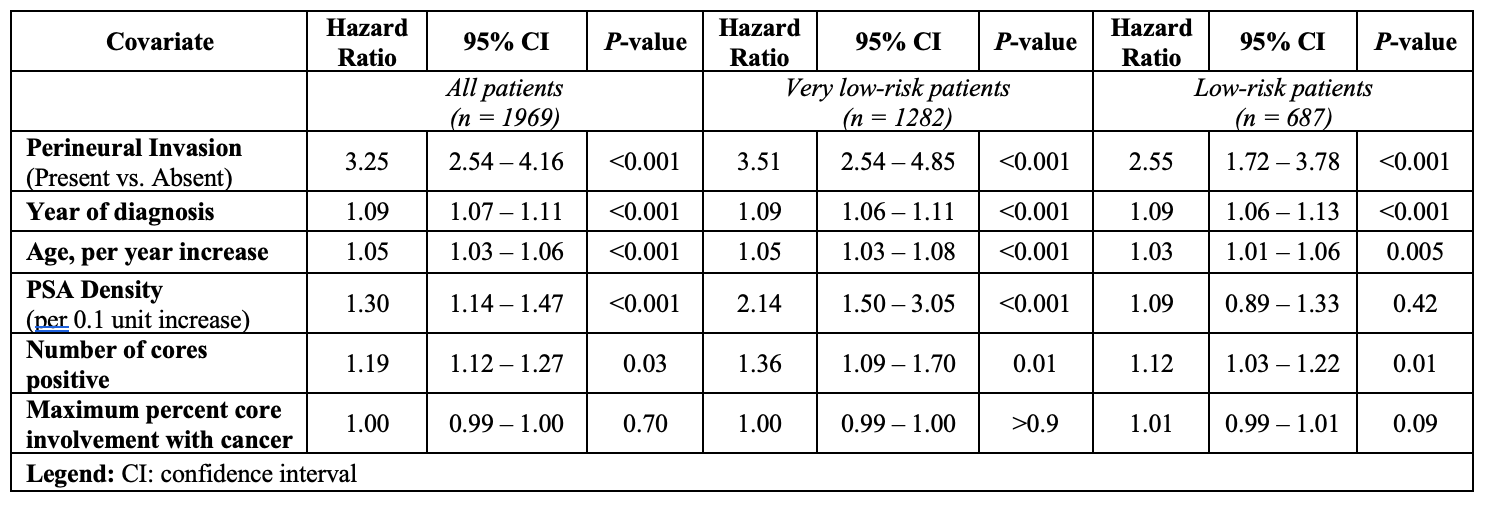
Methods: We retrospectively reviewed 1969 men enrolled in the Johns Hopkins AS registry from 1995 to 2021. All men had either very low-risk (n =1,282) or low-risk (n =687) disease at diagnosis and at least 1 follow-up biopsy. A time dependent cox model was used to assess the association between PNI and grade reclassification (GR) defined as the detection of Gleason grade group (GG) ³2 PCa on a surveillance biopsy, adjusting for age, PSA density, cancer volume metrics, and year of PCa diagnosis.
Results: Overall, median age was 66.0 years (IQR 61.0-69.0) and median PSA 4.9 ng/mL (IQR 3.9-6.4). Median follow-up after AS enrollment was 36 months (IQR 15-66). We identified 198 men (10.0%) with PNI detected on at least one prostate biopsy during AS (including the diagnostic biopsy). The men with PNI had significantly higher number of positive cores (median [IQR]: 1 [1-2] vs. 1 [1-2], p <0.001) and maximum percent core involvement (median [IQR]: 10 [1-20] vs. 5 [1-5], p =0.004) than the men without PNI. During AS, the men with PNI had more GR (87 patients (43.9%) vs. 465 (26.3%), p <0.001), and were more likely to undergo any treatment than the men without PNI (120 patients (60.6%) vs. 667 (37.7%), p <0.001). In a multivariable analysis PNI was significantly associated with GR (Table 1). Sixty-three patients with PNI underwent radical prostatectomy (RP) (31.8%) vs. 390 men without PNI (22.0%) (p =0.003). The men with PNI had more extraprostatic extension at RP compared to the group of men without PNI detected at biopsy (33.3% vs. 19.5%, p =0.02), but there was no difference in adverse pathology (defined at GG3 or higher and/or pT3 or higher and/or lymph node involvement) between the two groups.
Conclusions: PNI detected on biopsy in patients with low-risk PCa on AS is strongly associated with grade reclassification. PNI should not preclude low-risk patients from AS but our findings will allow us to better counsel men with PNI choosing AS versus treatment and help us determine how aggressively to monitor them while on AS.
Source of Funding: Funded by the James Buchanan Brady Urological Institute
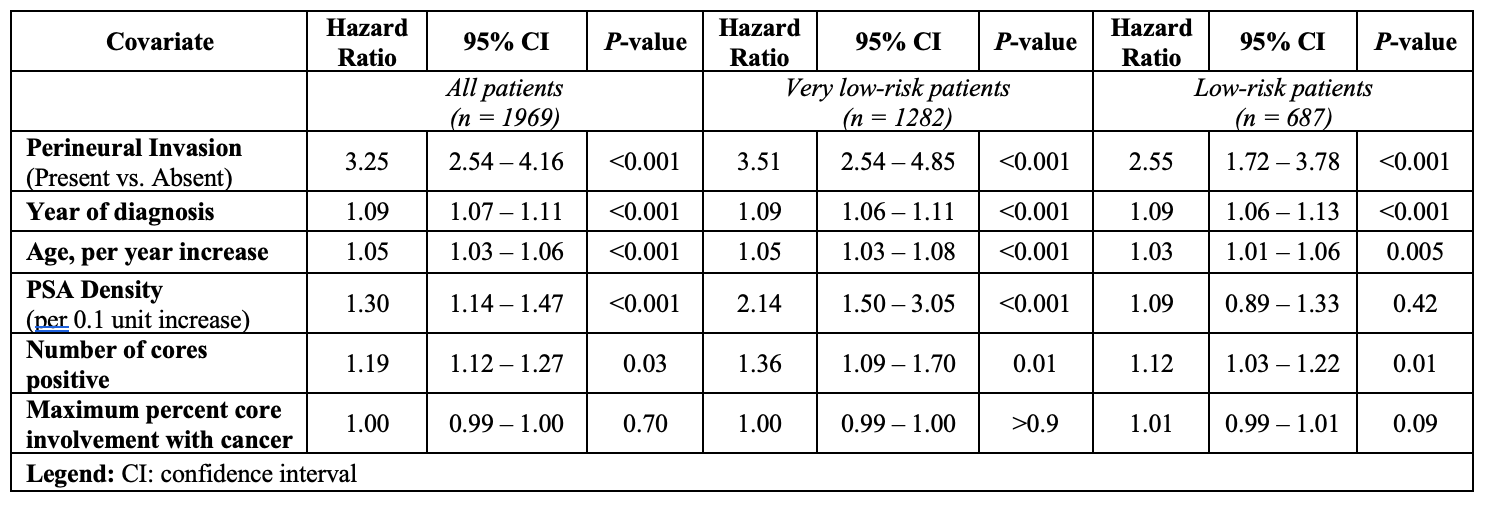
Methods: We retrospectively reviewed 1969 men enrolled in the Johns Hopkins AS registry from 1995 to 2021. All men had either very low-risk (n =1,282) or low-risk (n =687) disease at diagnosis and at least 1 follow-up biopsy. A time dependent cox model was used to assess the association between PNI and grade reclassification (GR) defined as the detection of Gleason grade group (GG) ³2 PCa on a surveillance biopsy, adjusting for age, PSA density, cancer volume metrics, and year of PCa diagnosis.
Results: Overall, median age was 66.0 years (IQR 61.0-69.0) and median PSA 4.9 ng/mL (IQR 3.9-6.4). Median follow-up after AS enrollment was 36 months (IQR 15-66). We identified 198 men (10.0%) with PNI detected on at least one prostate biopsy during AS (including the diagnostic biopsy). The men with PNI had significantly higher number of positive cores (median [IQR]: 1 [1-2] vs. 1 [1-2], p <0.001) and maximum percent core involvement (median [IQR]: 10 [1-20] vs. 5 [1-5], p =0.004) than the men without PNI. During AS, the men with PNI had more GR (87 patients (43.9%) vs. 465 (26.3%), p <0.001), and were more likely to undergo any treatment than the men without PNI (120 patients (60.6%) vs. 667 (37.7%), p <0.001). In a multivariable analysis PNI was significantly associated with GR (Table 1). Sixty-three patients with PNI underwent radical prostatectomy (RP) (31.8%) vs. 390 men without PNI (22.0%) (p =0.003). The men with PNI had more extraprostatic extension at RP compared to the group of men without PNI detected at biopsy (33.3% vs. 19.5%, p =0.02), but there was no difference in adverse pathology (defined at GG3 or higher and/or pT3 or higher and/or lymph node involvement) between the two groups.
Conclusions: PNI detected on biopsy in patients with low-risk PCa on AS is strongly associated with grade reclassification. PNI should not preclude low-risk patients from AS but our findings will allow us to better counsel men with PNI choosing AS versus treatment and help us determine how aggressively to monitor them while on AS.
Source of Funding: Funded by the James Buchanan Brady Urological Institute

.jpg)
.jpg)