Back
Poster, Podium & Video Sessions
Moderated Poster
MP43: Prostate Cancer: Localized: Active Surveillance
MP43-05: Upfront MRI is the new standard, have confirmatory biopsies become obsolete?
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 222
Henk Luiting, Ivo Izaak de Vos*, Sebastiaan Remmers, Egbert Boevé, Chris Bangma, Rotterdam, Netherlands, Riccardo Valdagni, Milan, Italy, Peter Chiu, Hong Kong, Hong Kong, Axel Semjonow, Münster, Germany, Viktor Berge, Oslo, Norway, Karl Tully, Herne, Germany, Antti Rannikko, Helsinki, Finland, Frédéric Staerman, Reims, France, Monique Roobol, Rotterdam, Netherlands
- ID
Ivo De Vos, BS
Erasmus MC
Poster Presenter(s)
Introduction: The AUA guidelines recommend confirmatory biopsies in all patients within two years after diagnosis whereas the EAU guidelines recommend refraining from confirmatory biopsies during active surveillance (AS) in patients diagnosed with upfront MRI. Data on these recommendations is conflicting and limited to highly experienced centers. The objective of this study is to add to the current evidence and to determine the risk difference for grade group (GG) reclassification on confirmatory biopsies between patients included with and without upfront MRI.
Methods: The PRIAS study is a multicenter prospective study providing clinical data of patients on AS. The inclusion criteria and recommended follow up schedule are available on www.prias-project.org. In this analysis, we selected patients diagnosed with or without upfront MRI, who underwent (a second) MRI before confirmatory biopsies. All subsequently underwent targeted biopsies (±systematic biopsies (SBx)) in lesions PIRADS=3, or SBx in case of no lesion. Multivariable logistic regression analysis was performed to determine the risk difference for GG reclassification at confirmatory biopsies between patients included with and without upfront MRI.
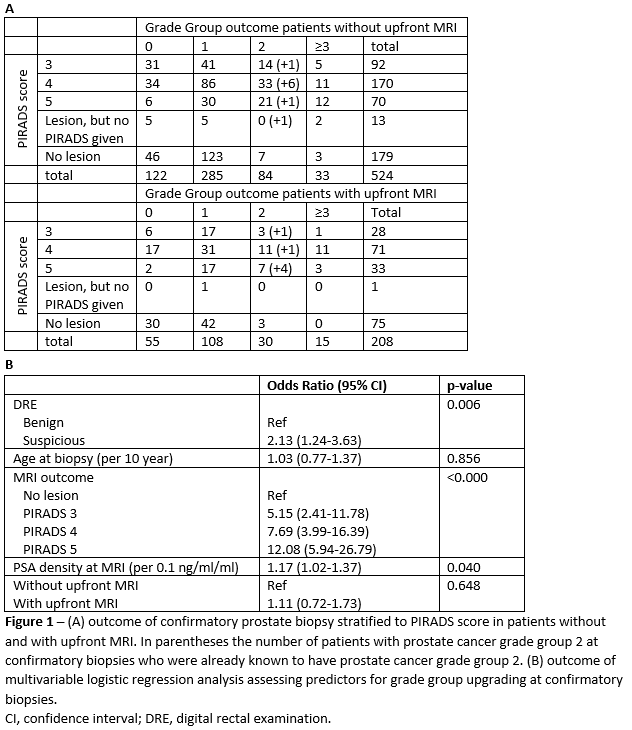
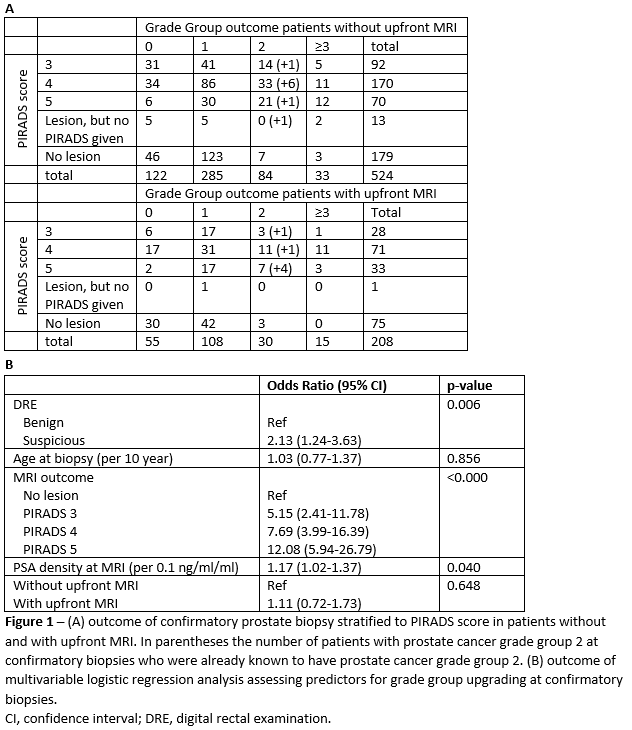
Results: In total, 732 patients underwent MRI informed confirmatory biopsies at a median PSA of 6.4 (interquartile range 4.6-8.4) ng/ml. 524 patients were diagnosed without upfront MRI and 208 with upfront MRI. Biopsy outcome and the outcome of multivariable logistic regression analysis are shown in Figure 1. At confirmatory biopsy, 108 (21%) patients without upfront MRI reclassified whereas 39 (19%) patients with upfront MRI reclassified. Reclassification to GG=3 was seen in 6% and 7% of the patients without and with upfront MRI respectively. No significant difference in risk for reclassification at confirmatory biopsies was seen between the two groups (OR 1.11 (95%CI 0.72-1.73), p=0.6), whereas MRI outcome, DRE outcome and PSA density were significant predictors for reclassification.
Conclusions: Our results show that upfront MRI does not reduce reclassification rates at confirmatory biopsy and as such does not support the EAU guidelines recommendation to simply omit confirmatory biopsies if upfront MRI is used. In preventing unnecessary biopsies during AS, our results highlight the importance of MRI outcome.
Source of Funding: `-
Methods: The PRIAS study is a multicenter prospective study providing clinical data of patients on AS. The inclusion criteria and recommended follow up schedule are available on www.prias-project.org. In this analysis, we selected patients diagnosed with or without upfront MRI, who underwent (a second) MRI before confirmatory biopsies. All subsequently underwent targeted biopsies (±systematic biopsies (SBx)) in lesions PIRADS=3, or SBx in case of no lesion. Multivariable logistic regression analysis was performed to determine the risk difference for GG reclassification at confirmatory biopsies between patients included with and without upfront MRI.
Results: In total, 732 patients underwent MRI informed confirmatory biopsies at a median PSA of 6.4 (interquartile range 4.6-8.4) ng/ml. 524 patients were diagnosed without upfront MRI and 208 with upfront MRI. Biopsy outcome and the outcome of multivariable logistic regression analysis are shown in Figure 1. At confirmatory biopsy, 108 (21%) patients without upfront MRI reclassified whereas 39 (19%) patients with upfront MRI reclassified. Reclassification to GG=3 was seen in 6% and 7% of the patients without and with upfront MRI respectively. No significant difference in risk for reclassification at confirmatory biopsies was seen between the two groups (OR 1.11 (95%CI 0.72-1.73), p=0.6), whereas MRI outcome, DRE outcome and PSA density were significant predictors for reclassification.
Conclusions: Our results show that upfront MRI does not reduce reclassification rates at confirmatory biopsy and as such does not support the EAU guidelines recommendation to simply omit confirmatory biopsies if upfront MRI is used. In preventing unnecessary biopsies during AS, our results highlight the importance of MRI outcome.
Source of Funding: `-

.jpg)
.jpg)