Back
Poster, Podium & Video Sessions
Moderated Poster
MP43: Prostate Cancer: Localized: Active Surveillance
MP43-06: Comparing MRI/US Fusion to Standard Prostate Biopsy in Determining Grade Reclassification at Confirmatory Biopsy in a Multi-Institutional Active Surveillance Cohort: A Pennsylvania Urology Regional Collaborative (PURC) Analysis
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 222
David Strauss*, Rohit Reddy, Matthew Loecher, Philadelphia, PA, Kaynaat Syed, Philadelphia , PA, John Danella, Danville, PA, Serge Ginzburg, Philadelphia, PA, Laurence Belkoff, Bala Cynwyd, PA, Jeffrey Tomaszewski, Camden, NJ, Edouard Trabulsi, Philadelphia, PA, Eric Singer, New Brunswick, NJ, Bruce Jacobs, Pittsburgh, PA, Jay Raman, Hershey, PA, Thomas Guzzo, Robert Uzzo, Adam Reese, Philadelphia, PA
- DS
David M. Strauss, MD
Lewis Katz School of Medicine at Temple University Hospital
Poster Presenter(s)
Introduction: Active surveillance (AS) has emerged as the optimal management of low-risk prostate cancer (CaP) patients, and relies on an accurate confirmatory biopsy to stratify disease risk. The literature is conflicting regarding whether multiparametric (mp) MRI/fusion biopsy improves detection of clinically significant cancers compared to standard 12-core trans rectal ultrasound (TRUS) at time of confirmatory AS biopsy. We aimed to analyze a prospectively maintained multi-institutional AS database with the intent to compare clinically significant reclassification rates between biopsy groups at confirmatory biopsy.
Methods: The Pennsylvania Urological Regional Collaborative (PURC) database, a prospectively maintained consortium CaP database, was retrospectively queried for all low-risk CaP men on AS. Patients were categorized by modality of confirmatory biopsy (either standard 12 core TRUS prostate biopsy or mpMRI targeted/ultrasound fusion prostate biopsy). The primary outcome of interest was grade group reclassification at the time of confirmatory biopsy.
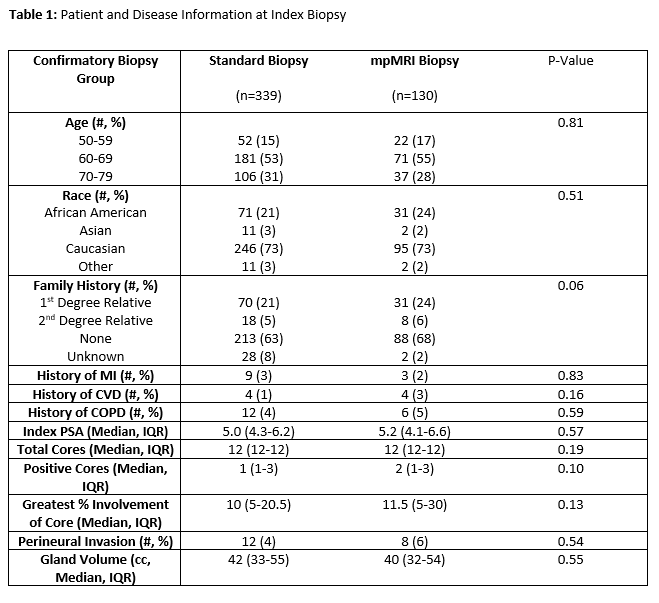
Results: The study cohort included 469 low risk men on AS, with 339 (72%) undergoing standard 12-core TRUS confirmatory biopsy and 130 (28%) undergoing fusion confirmatory biopsy. There were no differences between groups at index biopsy, regarding demographic or disease characteristics. (Table 1) Clinically significant grade reclassification, defined as GG2 or greater, was seen on 42% (54) of mpMRI biopsies vs. only 22% (74) of standard biopsies (p < 0.001). (Table 2)
Conclusions: The use of mp-MRI for AS confirmatory biopsy, compared to standard 12-core TRUS biopsy, improved the detection of clinically significant cancer. These findings suggest the value of MRI/US fusion biopsy to appropriately identify higher risk men on AS who may benefit from definitive treatment.
Source of Funding: N/A

Methods: The Pennsylvania Urological Regional Collaborative (PURC) database, a prospectively maintained consortium CaP database, was retrospectively queried for all low-risk CaP men on AS. Patients were categorized by modality of confirmatory biopsy (either standard 12 core TRUS prostate biopsy or mpMRI targeted/ultrasound fusion prostate biopsy). The primary outcome of interest was grade group reclassification at the time of confirmatory biopsy.
Results: The study cohort included 469 low risk men on AS, with 339 (72%) undergoing standard 12-core TRUS confirmatory biopsy and 130 (28%) undergoing fusion confirmatory biopsy. There were no differences between groups at index biopsy, regarding demographic or disease characteristics. (Table 1) Clinically significant grade reclassification, defined as GG2 or greater, was seen on 42% (54) of mpMRI biopsies vs. only 22% (74) of standard biopsies (p < 0.001). (Table 2)
Conclusions: The use of mp-MRI for AS confirmatory biopsy, compared to standard 12-core TRUS biopsy, improved the detection of clinically significant cancer. These findings suggest the value of MRI/US fusion biopsy to appropriately identify higher risk men on AS who may benefit from definitive treatment.
Source of Funding: N/A


.jpg)
.jpg)