Back
Poster, Podium & Video Sessions
Moderated Poster
MP43: Prostate Cancer: Localized: Active Surveillance
MP43-08: Active Surveillance for prostate cancer: uptake over time and the impact of an organized protocol
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 222
Sebastiaan Remmers*, Monique Roobol, ERSPC Rotterdam study group, Rotterdam, Netherlands

Sebastiaan Remmers, MSC
Erasmus MC Cancer Institute, University Medical Center Rotterdam
Poster Presenter(s)
Introduction: The European Randomized Study of Screening for Prostate Cancer (ERSPC) showed that PSA-based screening coincides with overdiagnosis and overtreatment. Active Surveillance (AS) was initiated to reduce the harm of overtreatment. However, the rate of uptake of AS is highly heterogeneous around the world. Here, we look at the uptake of AS over time. Specifically, we assessed whether the initiation of an organized protocol increased the rate of men opting for AS and looked at differences between screening and clinical setting.
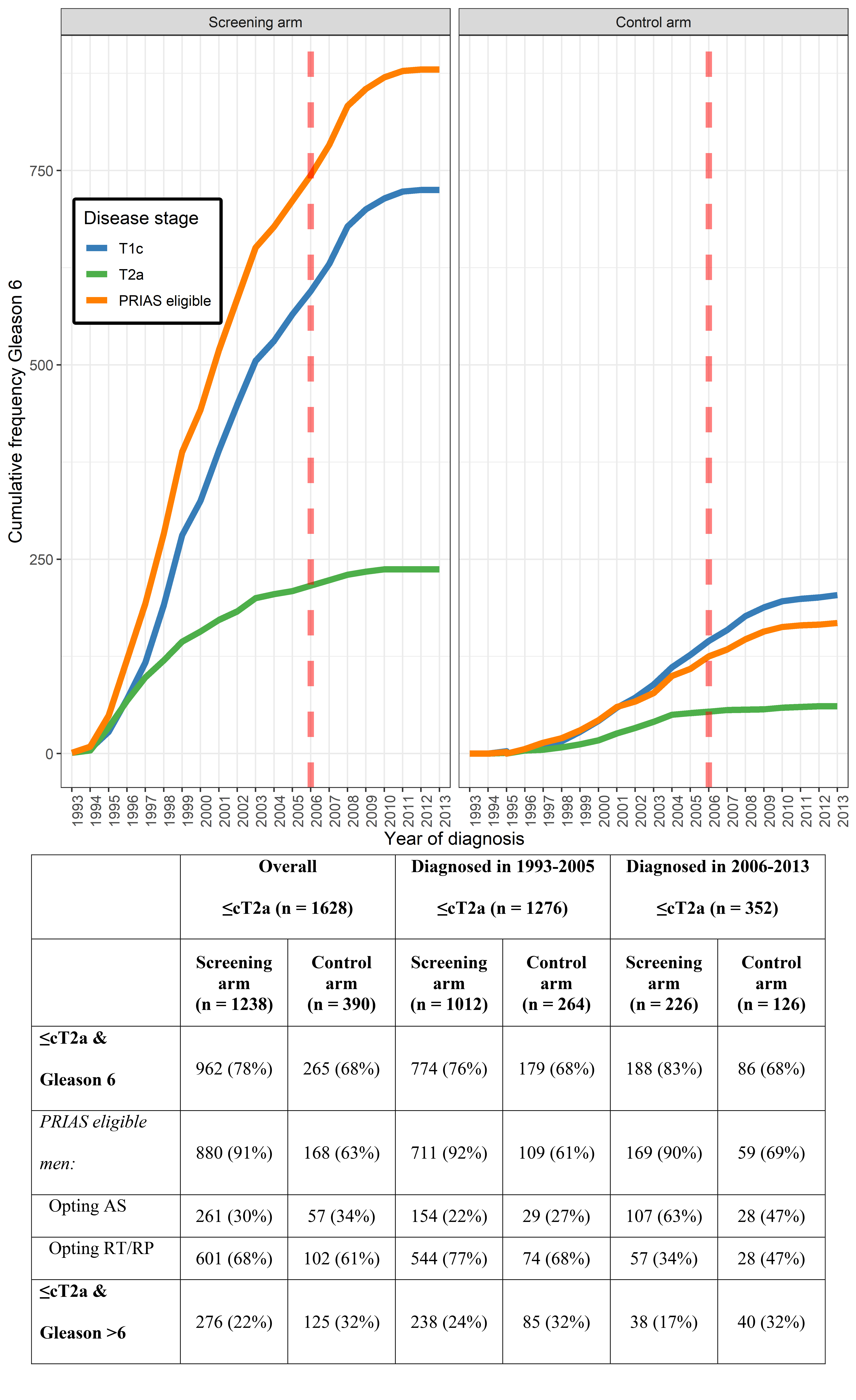
Methods: Data include diagnoses in the period 1993-2013 in men aged =70 yr diagnosed within ERSPC Rotterdam and eligible for AS according to the Prostate cancer Research International: Active Surveillance (PRIAS) pre-MRI criteria (Gleason 6, PSA <10 ng/ml, =cT2a). The number of PRIAS eligible men was compared against all men with low-risk disease in both arms of the trial and we assessed the choice of initial treatment for PRIAS eligible men before and after 2006 (the year PRIAS was initiated).
Results: In the study period, 962 men in the screening (S-) arm and 265 men in the control (C-) arm were diagnosed with cT1c/cT2a Gleason 6 disease (Tab/Fig). The percentage of PRIAS eligible men in this group is very different: 91% in the S-arm and 63% in the C-arm, reflecting lead time (lower PSA and tumor load). In the 90s and before PRIAS was initiated (i.e. <2006), 22% of all PRIAS eligible men in the S- arm opted for AS and 77% for radical prostatectomy (RP) / radiotherapy (RT); in the C- arm 27% opted for AS and 68% for RP/RT. From 2006 (initiation of PRIAS) till 2013 63% of the PRIAS eligible men in the S-arm opted for AS and 34% for RP/RT; in the C- arm 47% of the PRIAS eligible men opted for AS and 47% for RP/ RT. A difference most likely due to (although eligible for AS according to the PRIAS criteria) higher PSA values at diagnosis in the C- arm (median 6.2 ng/ml) than in the S-arm (median 3.9 ng/ml).
Conclusions: In conclusion, PSA-based screen-detected low risk PCa is in general suitable for an AS approach. The initiation and awareness of an organized protocol for AS has increased the uptake in men diagnosed with low-risk PCa, but there is certainly still room for improvement. Since (opportunistic) early detection practices are ubiquitous, next to avoiding overdiagnosis, the use of AS in clinical practice should be strongly encouraged.
Source of Funding: no
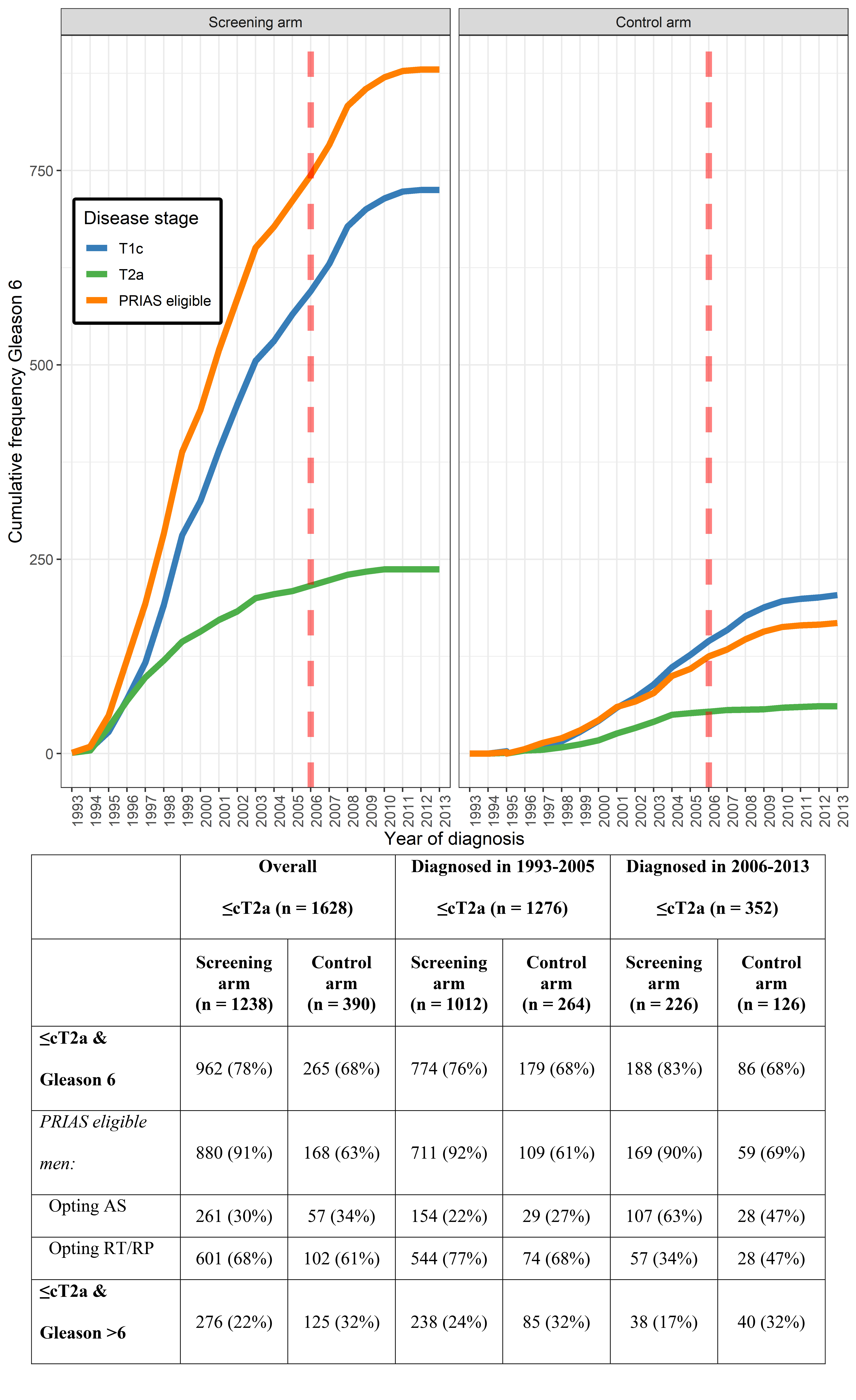
Methods: Data include diagnoses in the period 1993-2013 in men aged =70 yr diagnosed within ERSPC Rotterdam and eligible for AS according to the Prostate cancer Research International: Active Surveillance (PRIAS) pre-MRI criteria (Gleason 6, PSA <10 ng/ml, =cT2a). The number of PRIAS eligible men was compared against all men with low-risk disease in both arms of the trial and we assessed the choice of initial treatment for PRIAS eligible men before and after 2006 (the year PRIAS was initiated).
Results: In the study period, 962 men in the screening (S-) arm and 265 men in the control (C-) arm were diagnosed with cT1c/cT2a Gleason 6 disease (Tab/Fig). The percentage of PRIAS eligible men in this group is very different: 91% in the S-arm and 63% in the C-arm, reflecting lead time (lower PSA and tumor load). In the 90s and before PRIAS was initiated (i.e. <2006), 22% of all PRIAS eligible men in the S- arm opted for AS and 77% for radical prostatectomy (RP) / radiotherapy (RT); in the C- arm 27% opted for AS and 68% for RP/RT. From 2006 (initiation of PRIAS) till 2013 63% of the PRIAS eligible men in the S-arm opted for AS and 34% for RP/RT; in the C- arm 47% of the PRIAS eligible men opted for AS and 47% for RP/ RT. A difference most likely due to (although eligible for AS according to the PRIAS criteria) higher PSA values at diagnosis in the C- arm (median 6.2 ng/ml) than in the S-arm (median 3.9 ng/ml).
Conclusions: In conclusion, PSA-based screen-detected low risk PCa is in general suitable for an AS approach. The initiation and awareness of an organized protocol for AS has increased the uptake in men diagnosed with low-risk PCa, but there is certainly still room for improvement. Since (opportunistic) early detection practices are ubiquitous, next to avoiding overdiagnosis, the use of AS in clinical practice should be strongly encouraged.
Source of Funding: no

.jpg)
.jpg)