Back
Poster, Podium & Video Sessions
Moderated Poster
MP43: Prostate Cancer: Localized: Active Surveillance
MP43-11: The Use and Outcomes of Men with NCCN Favorable Intermediate Risk Prostate Cancer Managed with Active Surveillance
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 222
Roshan Paudel*, Ann Arbor, MI, Raghav Madan, Detroit, MI, Ji Qi, Ann Arbor, MI, Michael Cher, Detroit, MI, Brian Lane, Grand Rapids, MI, Arvin George, Alice Semerjian, Ann Arbor, MI, Kevin Ginsburg, Detroit, MI, for the Michigan Urological Surgery Improvement Collaborative, Ann Arbor, MI
- RP
Roshan Paudel
University of Michigan
Poster Presenter(s)
Introduction: To describe the use of active surveillance (AS), factors associated with the selection of AS, and time on AS for men with NCCN favorable intermediate risk prostate cancer (FIRPC) managed with AS in the Michigan Urological Surgery Improvement Collaborative (MUSIC) registry.
Methods: We calculated the proportion of men with FIRPC that selected AS by year of diagnosis and contributing practice from 2016 to 2020. Selection of AS was defined as both 1) AS listed as the primary management strategy and 2) absence of treatment for at least 12 months post diagnosis. A multivariable logistic regression model was fit to assess for the association of clinical, demographic, and oncological factors associated with AS selection, including the use and result (reassuring [RA] vs. non-reassuring [non-RA]) of confirmatory tests (Genomics, MRI, repeat TRUS, and targeted biopsy). Kaplan-Meier curves were used to estimate treatment free probability for patients on AS in the entire cohort and stratified by patients without, with RA, and non-RA confirmatory test.
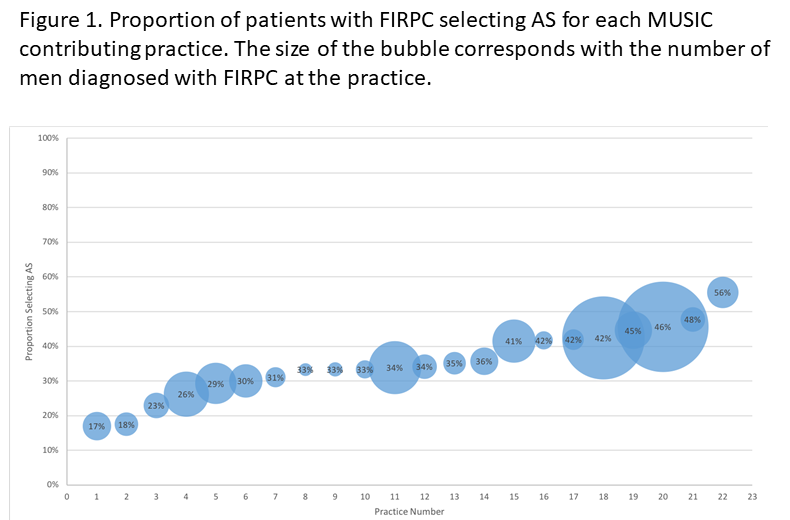
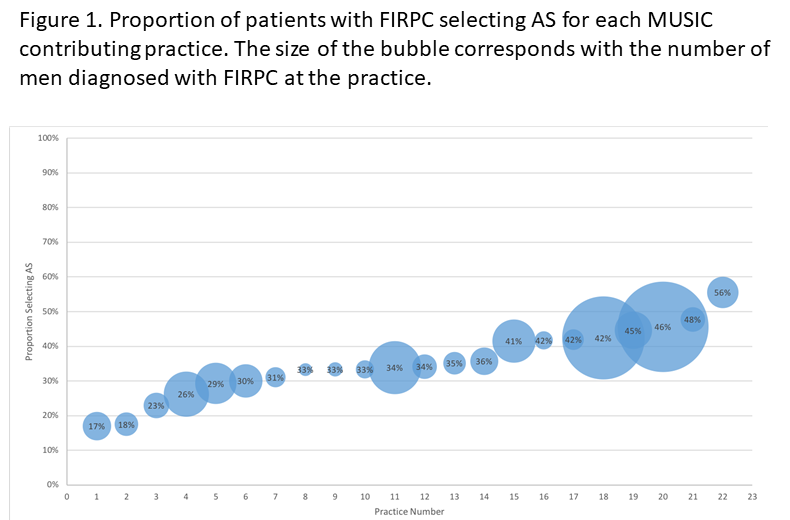
Results: We identified 2473 men diagnosed with FIRPC from 2016 to 2020, of which 977 (40%) chose AS. Use of AS for men with FIRPC gradually increased from 33% in 2016 to 48% in 2020. Additionally, there was notable variability in the proportion of men with FIRPC at each practice that selected AS, ranging from 17%-56% (Figure 1). In the multivariable model, we noted that increasing age (OR 1.10; 95% CI: 1.08-1.12, p<0.001) and RA confirmatory test results (OR 6.69, 95% CI 5.04-8.85, p<0.001) were associated with the selection of AS, while the presence of GG2 disease (OR 0.19, 95% CI 0.13-0.28, p<0.001) was associated with decreased odds of selecting AS. Of men with FIRPC on AS, 81% were free of treatment 24 months after diagnosis. Stratified by confirmatory testing, the estimated 24-month treatment free probability was 83% for patients without a confirmatory test compared with 87% for patients with RA and 78% for patients with non-RA confirmatory tests.
Conclusions: The use of AS for men with FIRPC has increased from 2016 to 2020, but there is notable variability in the proportion of patients with FIRPC selecting AS by contributing practices. Confirmatory tests may prove valuable in helping to select men and the intensity of surveillance for men on AS.
Source of Funding: Blue Cross Blue Shield of MI
Methods: We calculated the proportion of men with FIRPC that selected AS by year of diagnosis and contributing practice from 2016 to 2020. Selection of AS was defined as both 1) AS listed as the primary management strategy and 2) absence of treatment for at least 12 months post diagnosis. A multivariable logistic regression model was fit to assess for the association of clinical, demographic, and oncological factors associated with AS selection, including the use and result (reassuring [RA] vs. non-reassuring [non-RA]) of confirmatory tests (Genomics, MRI, repeat TRUS, and targeted biopsy). Kaplan-Meier curves were used to estimate treatment free probability for patients on AS in the entire cohort and stratified by patients without, with RA, and non-RA confirmatory test.
Results: We identified 2473 men diagnosed with FIRPC from 2016 to 2020, of which 977 (40%) chose AS. Use of AS for men with FIRPC gradually increased from 33% in 2016 to 48% in 2020. Additionally, there was notable variability in the proportion of men with FIRPC at each practice that selected AS, ranging from 17%-56% (Figure 1). In the multivariable model, we noted that increasing age (OR 1.10; 95% CI: 1.08-1.12, p<0.001) and RA confirmatory test results (OR 6.69, 95% CI 5.04-8.85, p<0.001) were associated with the selection of AS, while the presence of GG2 disease (OR 0.19, 95% CI 0.13-0.28, p<0.001) was associated with decreased odds of selecting AS. Of men with FIRPC on AS, 81% were free of treatment 24 months after diagnosis. Stratified by confirmatory testing, the estimated 24-month treatment free probability was 83% for patients without a confirmatory test compared with 87% for patients with RA and 78% for patients with non-RA confirmatory tests.
Conclusions: The use of AS for men with FIRPC has increased from 2016 to 2020, but there is notable variability in the proportion of patients with FIRPC selecting AS by contributing practices. Confirmatory tests may prove valuable in helping to select men and the intensity of surveillance for men on AS.
Source of Funding: Blue Cross Blue Shield of MI

.jpg)
.jpg)