Back
Poster, Podium & Video Sessions
Moderated Poster
MP43: Prostate Cancer: Localized: Active Surveillance
MP43-12: Impact of NCCN-Compliant Multidisciplinary Conference on the Utilization of Active Surveillance for Patients with Localized Prostate Cancer
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 222
Ayat A. Shah, Holly Houenstein, Yousuf Ramahi*, Philippa Doherty, Zhe Jing, Umar Iqbal, Caleb J. Eun, Grace E. Harrington, Mohammad Khan, Thomas Schwaab, Qiang Li, Eric C. Kauffman, James L. Mohler, Michael Kuettel, Khurshid A. Guru, Ahmed A. Hussein, Buffalo, NY

Yousuf Omar Ramahi, BS
Roswell Park Comprehensive Cancer Center
Poster Presenter(s)
Introduction: We sought to investigate the impact of the National Comprehensive Cancer Network (NCCN) compliant multidisciplinary conference on the uptake of active surveillance (AS) for patients with localized prostate cancer.
Methods: Retrospective review of Localized Prostate Cancer Conference (LPCC) database between 2009 and 2019 was performed. Patients who presented for a second opinion at our NCCN-compliant institution were presented to the multidisciplinary localized prostate cancer conference (LPCC) (comprises urologists, radiation oncologists, GU pathologists, and patient advocates). Patients who were eligible for AS (with very low, low, and intermediate favorable NCCN risk) were identified. We investigated the frequency AS was recommended by the community urologists versus by LPCC, and how many patients received it. Multivariate regression (MVA) model was utilized to evaluate variables associated with receiving AS. Cochrane-Armitage test was utilized to assess trends over time.
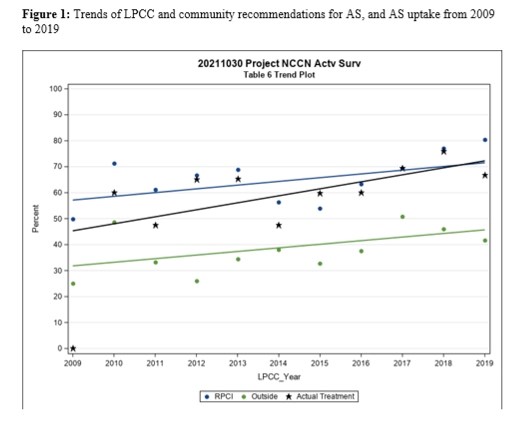
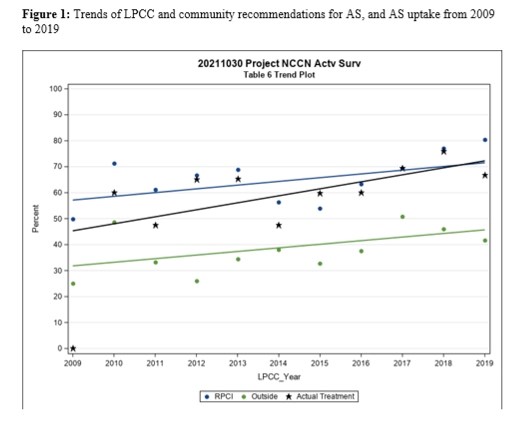
Results: Of the 612 patients eligible for AS, 15% were NCCN very low, 39% low, and 46% favorable intermediate risk. AS was recommended by community urologists in 247 cases (40%) and by the LPCC in 404 cases (66%) and 301 (62%) received AS. Patients who elected treatment were older (64 vs 60 years, p-value <0.01), had larger prostate volume (37 vs 34 mL, p-value <0.01), less positive biopsy cores (2 vs 3, p-value <0.01), longer PSA doubling time (6 vs 5 years, p-value=0.01), lower PSA density (0.11 vs 0.16 ng/mL2, p-value <0.01), Gleason grade 3+4=7 less frequently (27% vs 64%, p-value <0.01), and NCCN favorable intermediate risk less frequently (67% vs 31%, p-value <0.01). On MVA, more recent LPCC era (OR 9.63, 95%CI 3.03-30.60, p<0.0001), and older age (OR 1.12, 95%CI 1.08-1.15, p<0.0001) were more likely to receive AS. Higher number of positive biopsy cores (OR 0.68, 95%CI 0.59-0.78, p<0.0001) and favorable intermediate risk (OR 0.17, 95%CI 0.08-0.36, p<0.0001) were less likely to receive AS. Recommending AS over time increased: by community urologists (from 32% to 47%) and by the LPCC (57% to 72%) (p>0.05). The uptake of AS increased significantly (from 45% to 72%, p<0.005) (Figure 1).
Conclusions: Among patients who are eligible for AS, 40% were recommended AS by community urologists versus 66% by LPCC and 62% received it. NCCN favorable intermediate, and higher number of positive biopsy cores were associated with lower odds of receiving AS, while older patients and more recent LPCC era were more likely to receive it.
Source of Funding: none
Methods: Retrospective review of Localized Prostate Cancer Conference (LPCC) database between 2009 and 2019 was performed. Patients who presented for a second opinion at our NCCN-compliant institution were presented to the multidisciplinary localized prostate cancer conference (LPCC) (comprises urologists, radiation oncologists, GU pathologists, and patient advocates). Patients who were eligible for AS (with very low, low, and intermediate favorable NCCN risk) were identified. We investigated the frequency AS was recommended by the community urologists versus by LPCC, and how many patients received it. Multivariate regression (MVA) model was utilized to evaluate variables associated with receiving AS. Cochrane-Armitage test was utilized to assess trends over time.
Results: Of the 612 patients eligible for AS, 15% were NCCN very low, 39% low, and 46% favorable intermediate risk. AS was recommended by community urologists in 247 cases (40%) and by the LPCC in 404 cases (66%) and 301 (62%) received AS. Patients who elected treatment were older (64 vs 60 years, p-value <0.01), had larger prostate volume (37 vs 34 mL, p-value <0.01), less positive biopsy cores (2 vs 3, p-value <0.01), longer PSA doubling time (6 vs 5 years, p-value=0.01), lower PSA density (0.11 vs 0.16 ng/mL2, p-value <0.01), Gleason grade 3+4=7 less frequently (27% vs 64%, p-value <0.01), and NCCN favorable intermediate risk less frequently (67% vs 31%, p-value <0.01). On MVA, more recent LPCC era (OR 9.63, 95%CI 3.03-30.60, p<0.0001), and older age (OR 1.12, 95%CI 1.08-1.15, p<0.0001) were more likely to receive AS. Higher number of positive biopsy cores (OR 0.68, 95%CI 0.59-0.78, p<0.0001) and favorable intermediate risk (OR 0.17, 95%CI 0.08-0.36, p<0.0001) were less likely to receive AS. Recommending AS over time increased: by community urologists (from 32% to 47%) and by the LPCC (57% to 72%) (p>0.05). The uptake of AS increased significantly (from 45% to 72%, p<0.005) (Figure 1).
Conclusions: Among patients who are eligible for AS, 40% were recommended AS by community urologists versus 66% by LPCC and 62% received it. NCCN favorable intermediate, and higher number of positive biopsy cores were associated with lower odds of receiving AS, while older patients and more recent LPCC era were more likely to receive it.
Source of Funding: none

.jpg)
.jpg)