Back
Poster, Podium & Video Sessions
Moderated Poster
MP43: Prostate Cancer: Localized: Active Surveillance
MP43-15: A 5-year Prospective Study of African American Men on Prostate Cancer Active Surveillance: Does Race Predict Upgrading?
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 222
Joshua Pincus*, Jacob W. Greenberg, Christopher Koller, New Orleans, LA, Jonathan Silberstein, Aventura, FL, L. Spencer Krane, New Orleans, LA

Joshua Pincus
Tulane University School of Medicine
Poster Presenter(s)
Introduction: Active surveillance (AS) is a widely accepted management option for patients with very low and low risk prostate cancer (PCa) to minimize side effects of treatment without compromise of disease mortality. However, most large single institution studies are underrepresented for men from African American (AA) heritage. In this large prospective cohort we hypothesized that race was not associated with Gleason upgrading (GU) for patients electing AS.
Methods: All patients who elected AS for PCa at the Southeast Louisiana Veterans Health Care System are entered into a prospectively managed observational database. Patients were divided into groups based on self-reported race. GU was defined as an increase in WHO grade group (GG) on subsequent biopsy over GG 1. All tests were two sided using a significance of 0.05.
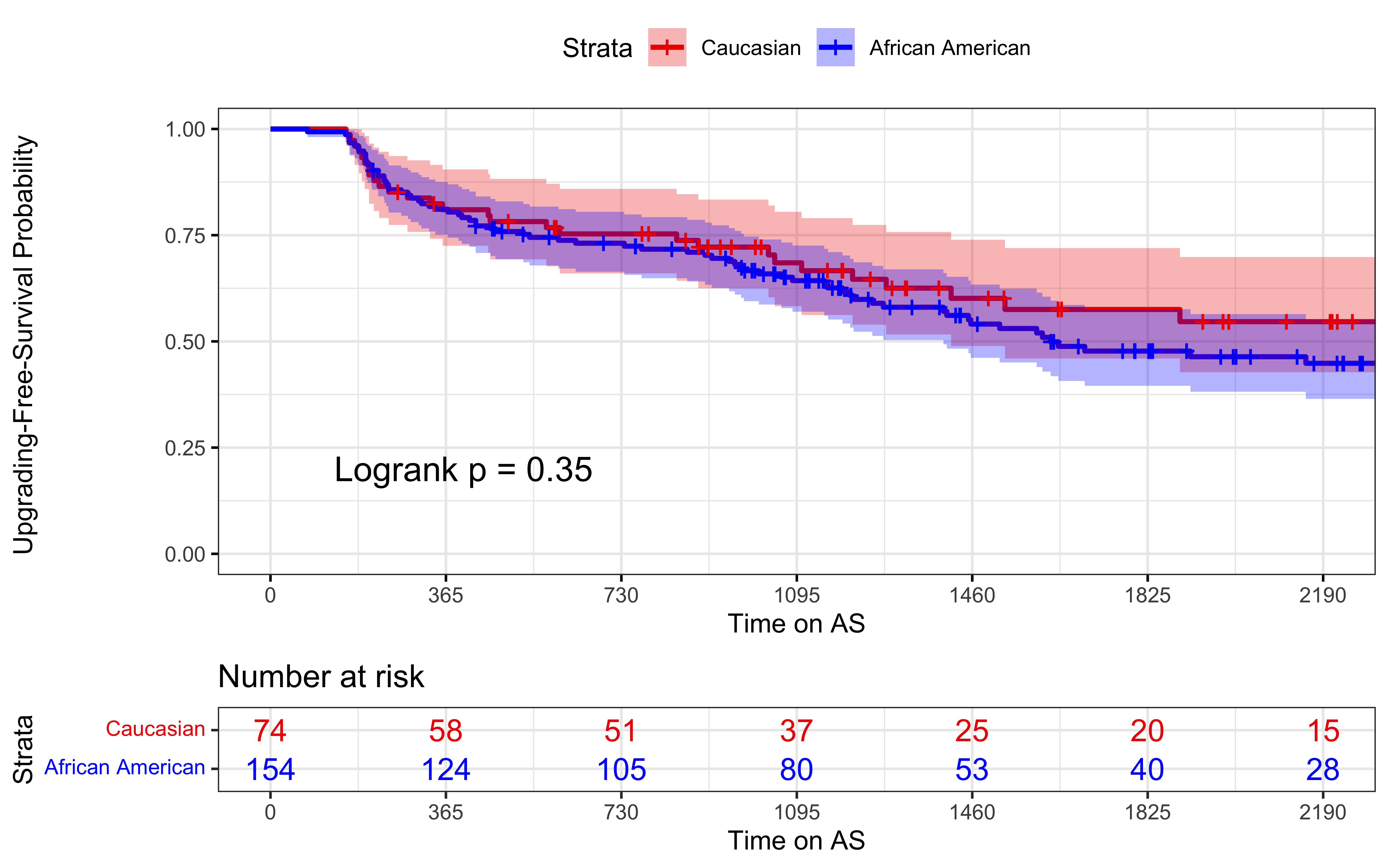
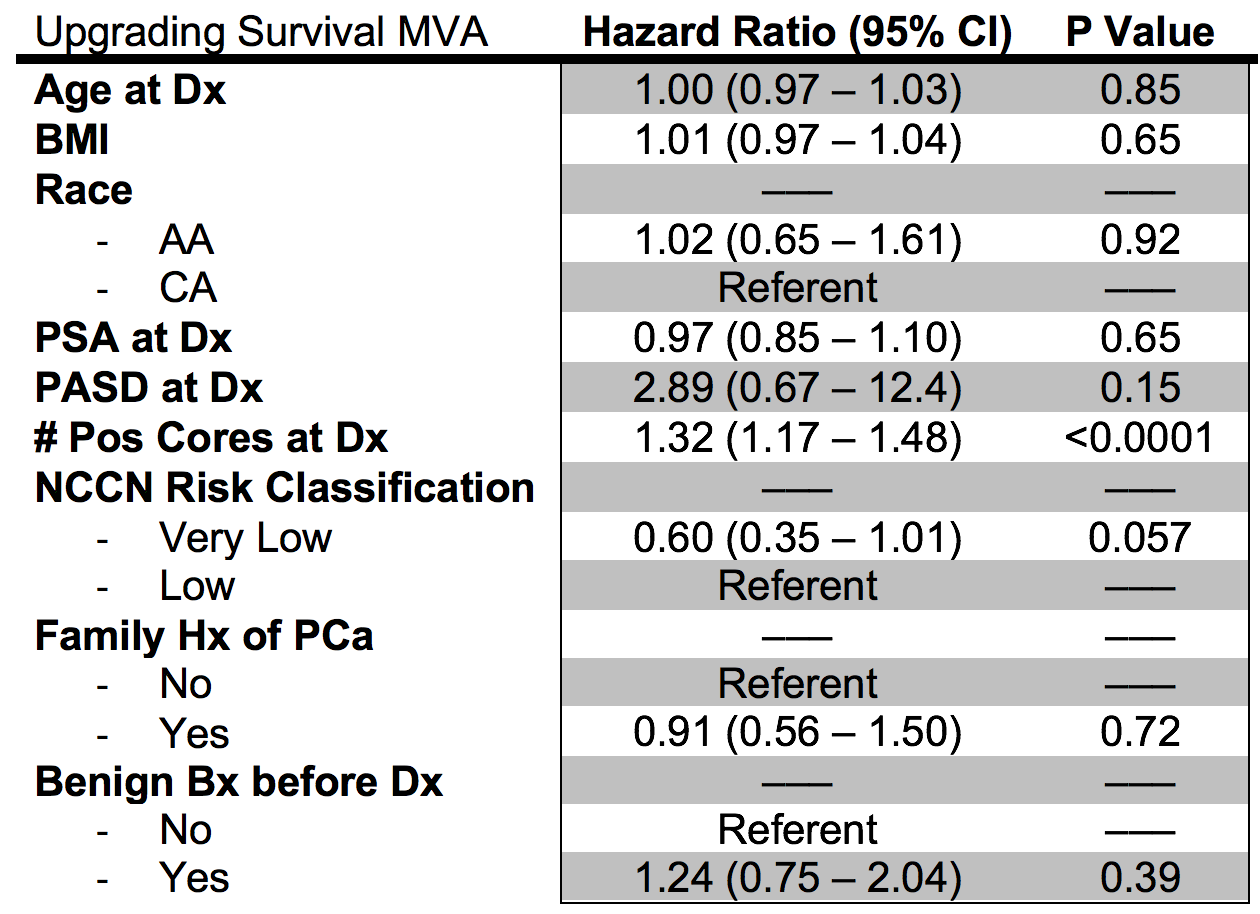
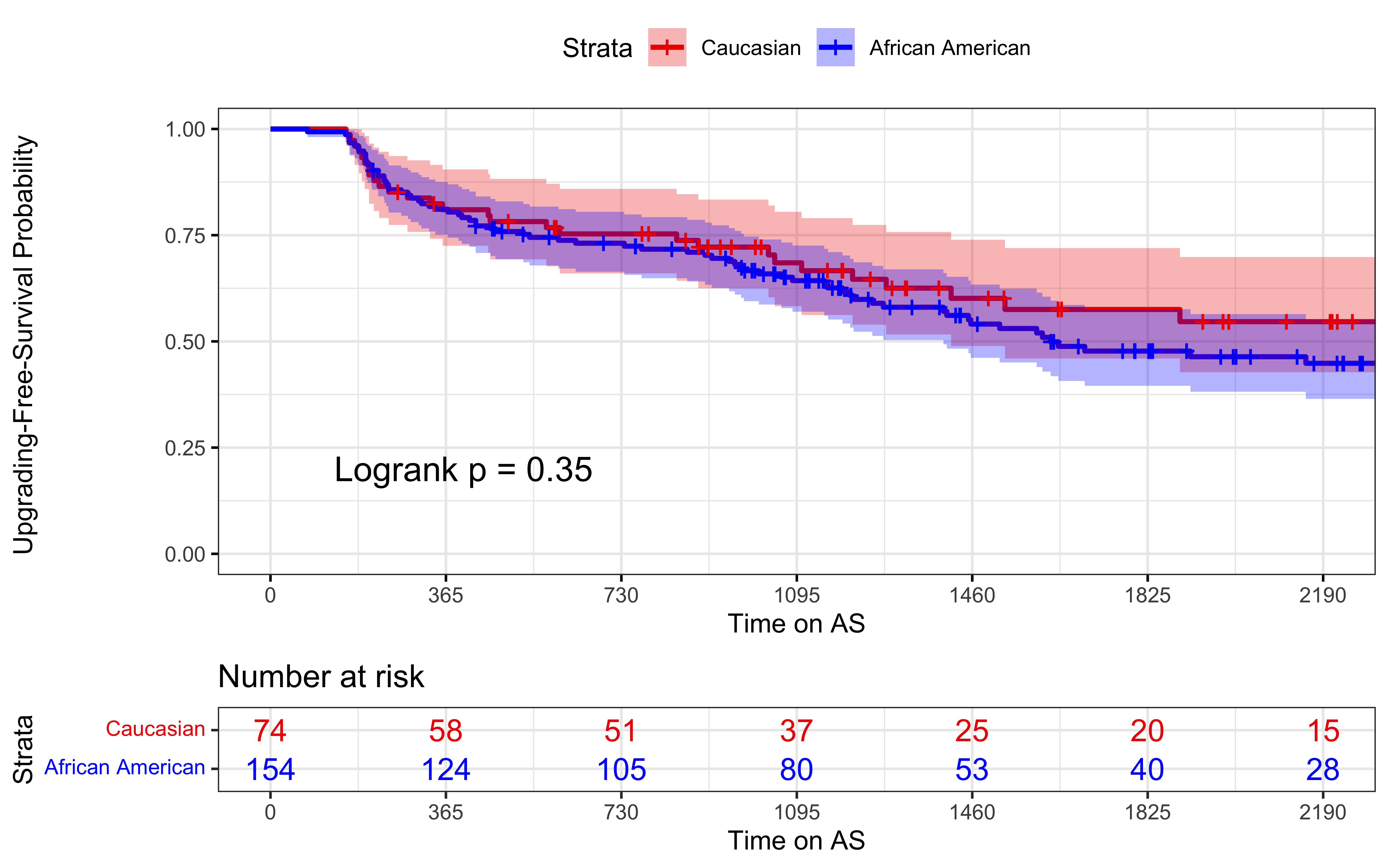
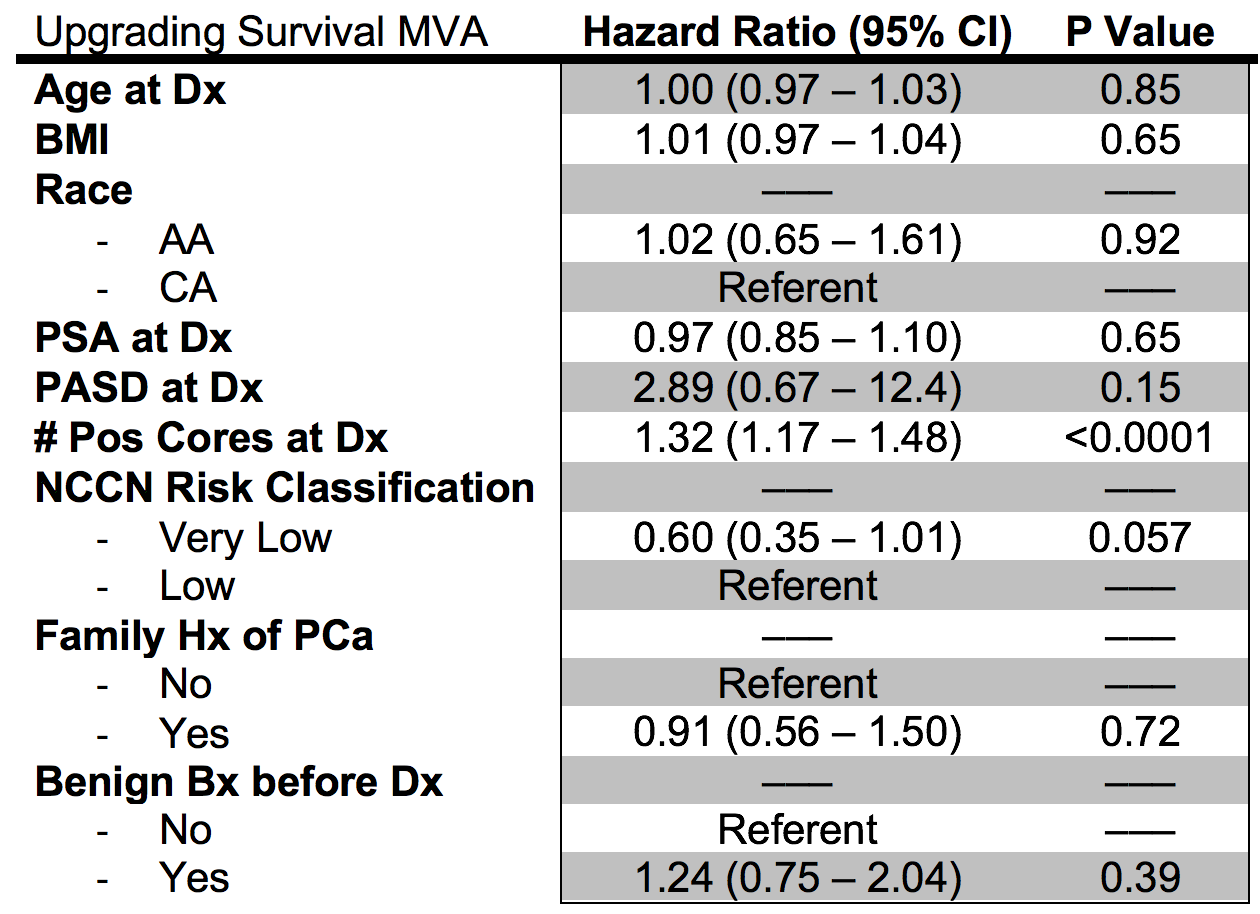
Results: 228 men were enrolled in the study, including 154 AA and 74 CA men, with a median follow-up of 5 years from the initiation of AS. At the time of diagnostic biopsy, there was no significant difference with respect to age, family history of PCa, smoking status, PSA, PSA density, prostate volume, or number of positive cores (all P values > 0.05). AA race was not predictive of GU on Cox multivariate analysis (Table 1), with a hazard ratio (HR) of 1.02 and 95% CI of 0.65 - 1.61 (P = 0.92). Number of positive cores was correlated with GU (HR = 1.32, CI 1.17-1.48, P < 0.0001). On Kaplan-Meier analysis (Figure 1), the 2.5-year GU-Free survival probability was 71% for AA (CI 63% - 78%) and 72% for CA (CI 63% - 83%). At 5 years, AA GU-free survival probability was 48% (CI 40% - 58%) versus 58% for CA (CI 46% - 72%). Risk of GU was similar between races (p=0.35) at both 2.5 and 5 years with 47% of all patients remaining on AS or without local curative therapy.
Conclusions: AS is a safe treatment option for low and very low risk PCa, regardless of race. AA and CA men did not have any significant difference in GU in our cohort with five-year follow up. Importantly, our study is conducted in an equal access setting and includes a large prospective cohort of AA patients on AS for PCa.
Source of Funding: None
Methods: All patients who elected AS for PCa at the Southeast Louisiana Veterans Health Care System are entered into a prospectively managed observational database. Patients were divided into groups based on self-reported race. GU was defined as an increase in WHO grade group (GG) on subsequent biopsy over GG 1. All tests were two sided using a significance of 0.05.
Results: 228 men were enrolled in the study, including 154 AA and 74 CA men, with a median follow-up of 5 years from the initiation of AS. At the time of diagnostic biopsy, there was no significant difference with respect to age, family history of PCa, smoking status, PSA, PSA density, prostate volume, or number of positive cores (all P values > 0.05). AA race was not predictive of GU on Cox multivariate analysis (Table 1), with a hazard ratio (HR) of 1.02 and 95% CI of 0.65 - 1.61 (P = 0.92). Number of positive cores was correlated with GU (HR = 1.32, CI 1.17-1.48, P < 0.0001). On Kaplan-Meier analysis (Figure 1), the 2.5-year GU-Free survival probability was 71% for AA (CI 63% - 78%) and 72% for CA (CI 63% - 83%). At 5 years, AA GU-free survival probability was 48% (CI 40% - 58%) versus 58% for CA (CI 46% - 72%). Risk of GU was similar between races (p=0.35) at both 2.5 and 5 years with 47% of all patients remaining on AS or without local curative therapy.
Conclusions: AS is a safe treatment option for low and very low risk PCa, regardless of race. AA and CA men did not have any significant difference in GU in our cohort with five-year follow up. Importantly, our study is conducted in an equal access setting and includes a large prospective cohort of AA patients on AS for PCa.
Source of Funding: None

.jpg)
.jpg)