Back
Poster, Podium & Video Sessions
Moderated Poster
MP43: Prostate Cancer: Localized: Active Surveillance
MP43-16: Racial Disparities in Rates of Gleason Grade Reclassification in a Multi-Institutional Prostate Cancer Active Surveillance Cohort: A Pennsylvania Urology Regional Collaborative (PURC) Analysis
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 222
Rohit Reddy*, David Strauss, Matthew Loecher, Kaynaat Syed, Philadelphia, PA, John Danella, Danville, PA, Serge Ginzburg, Philadelphia, PA, Laurence Belkoff, Bala Cynwyd, PA, Jeffrey Tomaszewski, Camden, NJ, Edouard Trabulsi, Philadelphia, PA, Eric A Singer, New Brunswick, NJ, Bruce L Jacobs, Pittsburgh, PA, Jay Raman, Hershey, PA, Thomas Guzzo, Thomas Guzzo, Robert Uzzo, Adam C Reese, Philadelphia, PA

Rohit Reddy, MD, BA
Temple University Hospital
Poster Presenter(s)
Introduction: Active surveillance (AS) is an established management option for patients with low-risk prostate cancer (CaP), with favorable long-term oncologic outcomes. Previous literature has shown significant racial CaP disparities with African-American (AA) men having a higher incidence of disease and more aggressive tumors. The purpose of this study is to analyze a prospectively maintained multi-institutional AS database to compare Gleason grade reclassification rates on confirmatory biopsy stratified by race.
Methods: The Pennsylvania Urological Regional Collaborative (PURC) is a prospectively maintained CaP quality improvement collaborative. The PURC database was queried for low risk CaP men on AS divided by race (AA vs Caucasian/Other). The primary outcome of interest was the rate of Gleason grade reclassification at the time of confirmatory biopsy.
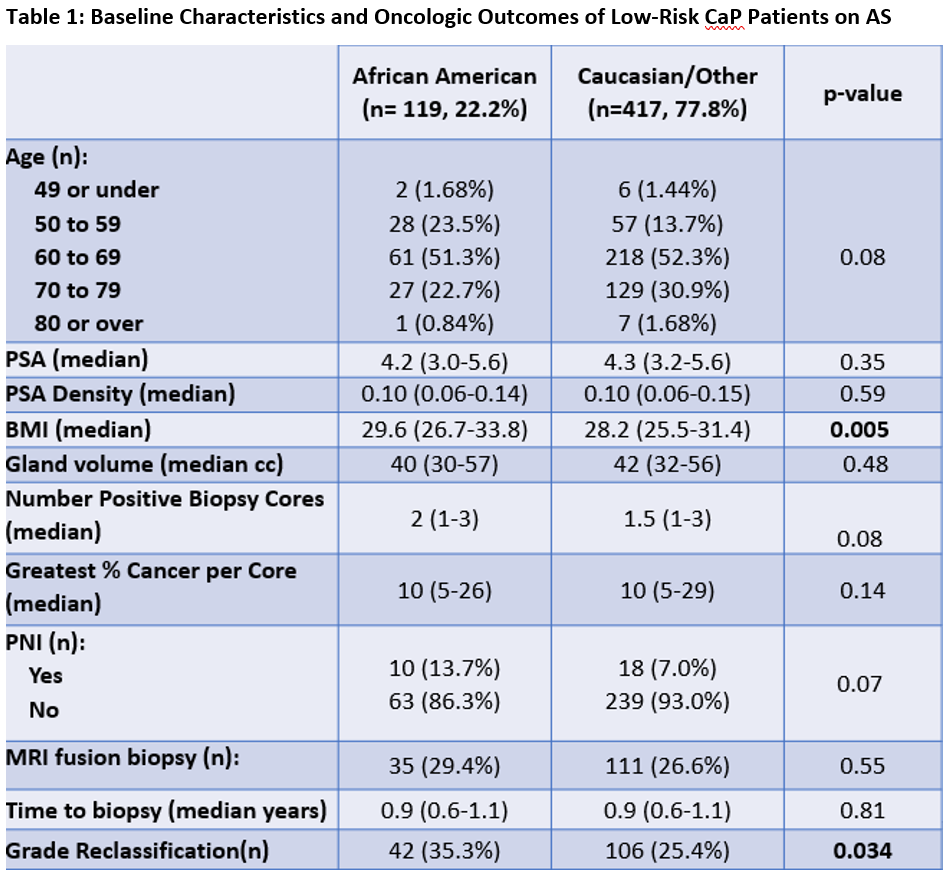
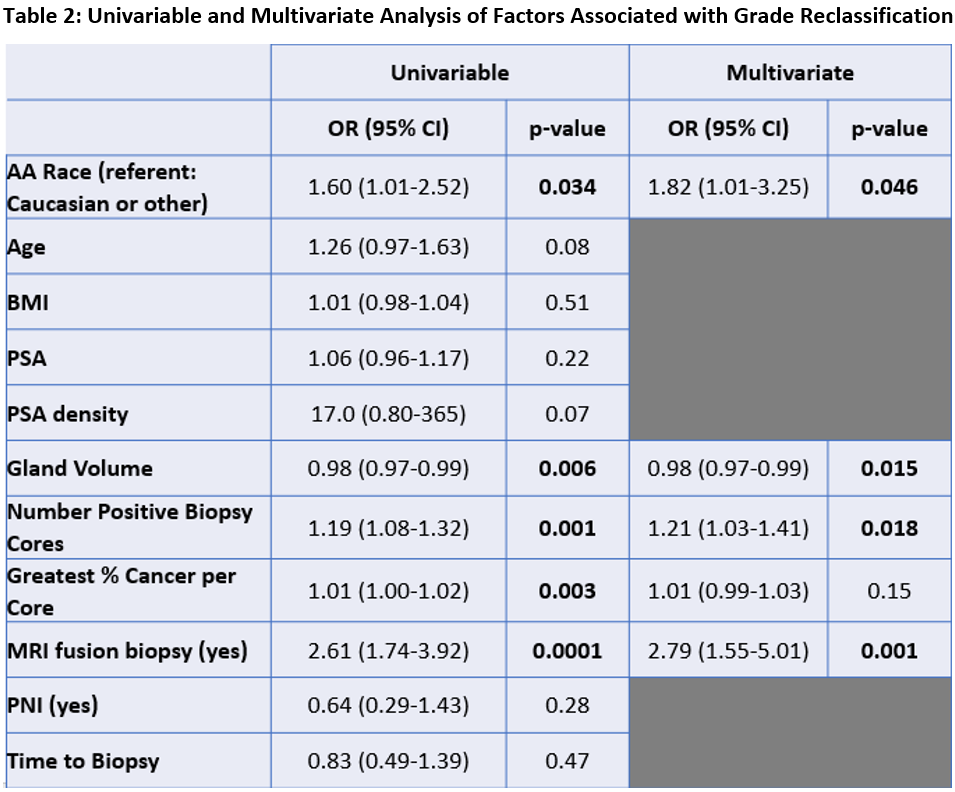
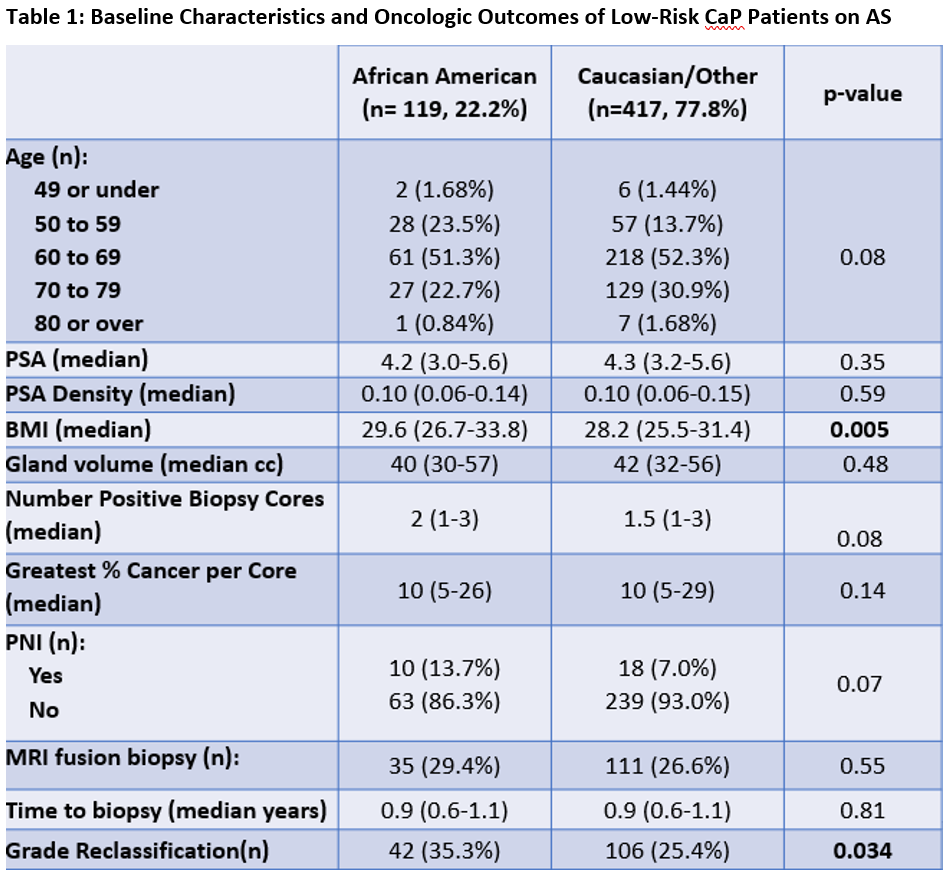
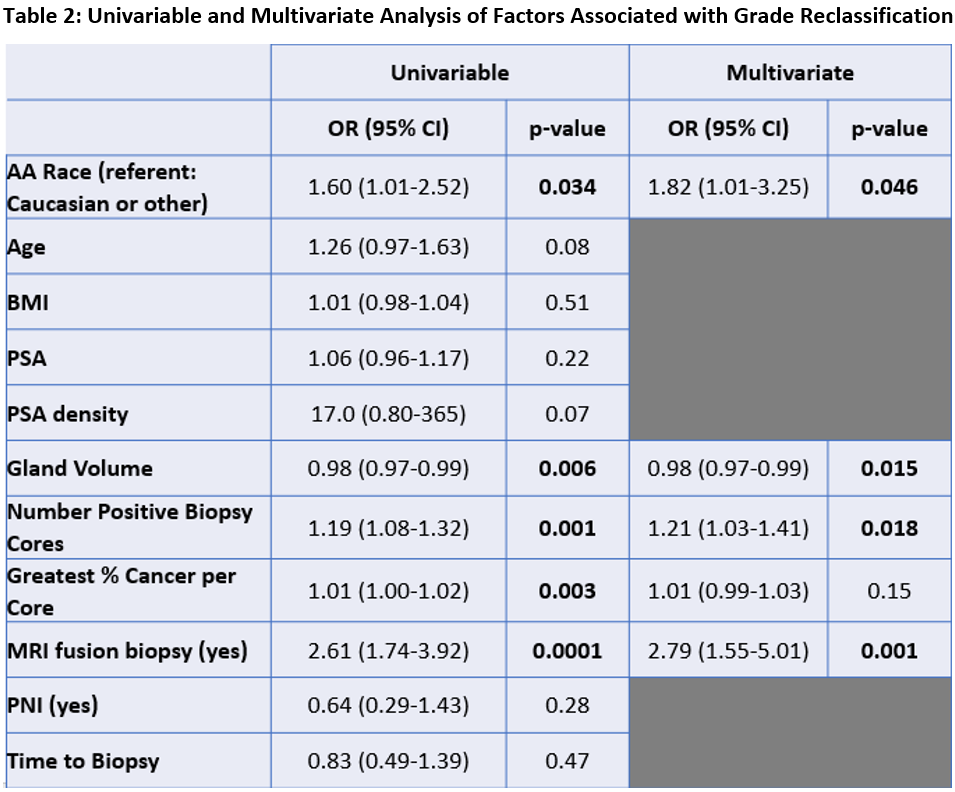
Results: The study cohort included 536 patients with low risk CaP on AS, comprised of 119 (22.2%) AA and 417 (77.8%) Caucasian/Other men. Other than BMI, there were no significant differences in either patient demographics or index biopsy parameters between groups (Table 1). AA men had a significantly higher rate of grade reclassification (35.3% vs 25.4%, p=0.034). On multivariate analysis, AA race was an independent predictor of grade reclassification (OR 1.82, p=0.042) (Table 2).
Conclusions: Established AS selection criteria and surveillance protocols fail to account for potential racial disparities in oncologic outcomes among patients with CaP. AA men in PURC exhibited a higher rate of grade reclassification on confirmatory biopsy, suggesting that AA men may need alternate AS surveillance criteria potentially including adjunct studies (mpMRI, genomic studies) to accurately risk stratify their CaP.
Source of Funding: None
Methods: The Pennsylvania Urological Regional Collaborative (PURC) is a prospectively maintained CaP quality improvement collaborative. The PURC database was queried for low risk CaP men on AS divided by race (AA vs Caucasian/Other). The primary outcome of interest was the rate of Gleason grade reclassification at the time of confirmatory biopsy.
Results: The study cohort included 536 patients with low risk CaP on AS, comprised of 119 (22.2%) AA and 417 (77.8%) Caucasian/Other men. Other than BMI, there were no significant differences in either patient demographics or index biopsy parameters between groups (Table 1). AA men had a significantly higher rate of grade reclassification (35.3% vs 25.4%, p=0.034). On multivariate analysis, AA race was an independent predictor of grade reclassification (OR 1.82, p=0.042) (Table 2).
Conclusions: Established AS selection criteria and surveillance protocols fail to account for potential racial disparities in oncologic outcomes among patients with CaP. AA men in PURC exhibited a higher rate of grade reclassification on confirmatory biopsy, suggesting that AA men may need alternate AS surveillance criteria potentially including adjunct studies (mpMRI, genomic studies) to accurately risk stratify their CaP.
Source of Funding: None

.jpg)
.jpg)