Back
Poster, Podium & Video Sessions
Moderated Poster
MP43: Prostate Cancer: Localized: Active Surveillance
MP43-18: Prostate Cancer Mortality Rates in Low and Favorable Intermediate Risk Active Surveillance Patients: A Population-Based Competing Risks Analysis
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 222
Rashid Sayyid*, John Benton, William Reed, Merry Ma, Phillip Woodruff, Martha Terris, Augusta, GA, Christopher Wallis, Toronto, Canada, Zachary Klaassen, Augusta, GA

Rashid Sayyid, MD
Augusta University
Poster Presenter(s)
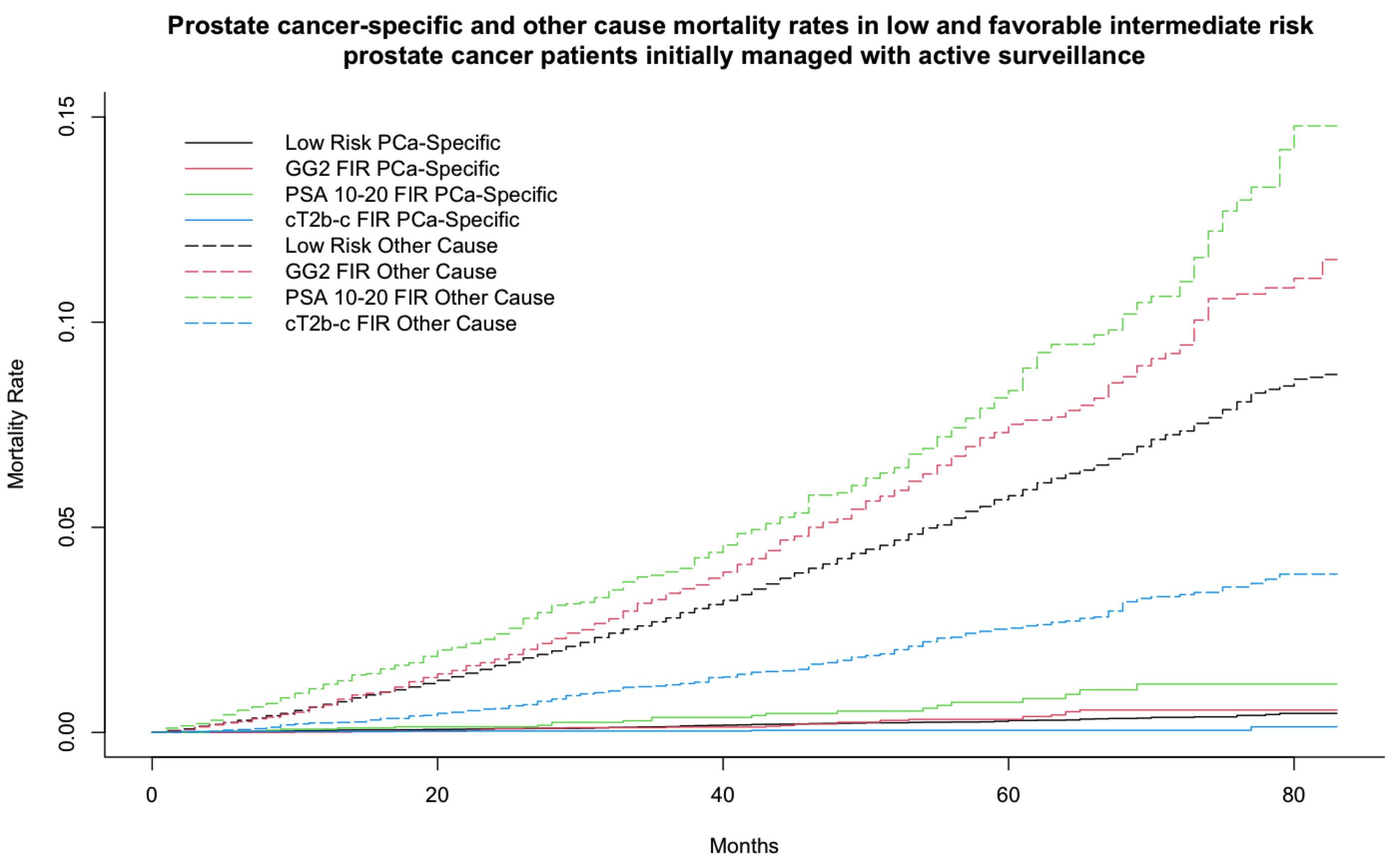
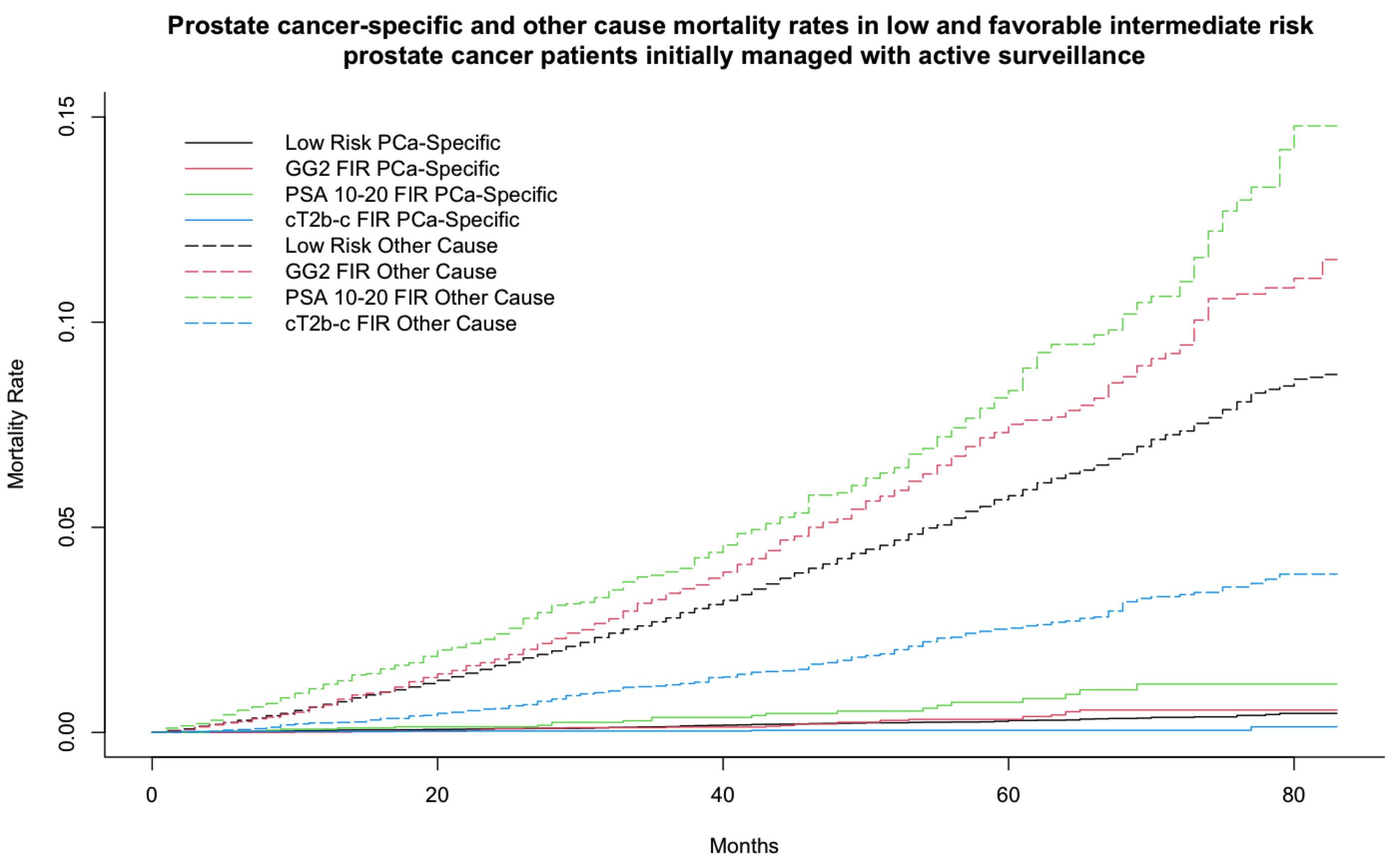
Introduction: Active surveillance (AS) use is recommended for low and select favorable intermediate risk (FIR) prostate cancer (PCa) patients. PCa mortality rates, and thus suitability of AS, in individual FIR subgroups remain undefined. Our objective was to determine PCa and other-cause mortality rates in low and FIR AS patients.
Methods: The Surveillance, Epidemiology, and End Results Prostate with Watchful Waiting database was used to identify men diagnosed with NCCN low or FIR PCa between 2010 and 2015, managed initially with AS. Patients in the FIR group were subdivided into three risk subgroups depending on their intermediate risk factor: Grade Group (GG) two disease, prostate-specific antigen (PSA) level 10-20 ng/ml and cT2b-c. Cumulative incidence function curves with other-cause mortality as the competing risk were utilized. Multivariable regression analyses using Fine and Gray’s semi-parametric proportional hazards model were used to assess predictors of PCa mortality.
Results: Among 70,871 patients, 48,127 (67.9%) had low and 22,744 (32.1%) had FIR disease. Median follow up was 49.0 months. There were 166 (0.2%) PCa and 3,176 (4.48%) other-cause mortalities. The five-year PCa mortality rates in the low and FIR cohorts overall were 0.29% and 0.28%, respectively (p=0.64). Within the FIR cohort, the corresponding rates were highest in the PSA 10-20 ng/ml subgroup at 0.73%, followed by 0.32% for Grade Group 2 FIR and 0.052% for cT2b-c FIR disease (p < 0.001).
On multivariable analysis, patients with Medicaid insurance (subdistribution hazard ratio [sHR]: 2.58, p=0.006), lowest SES (sHR:1.39, p=0.032), older age at diagnosis (sHR: 2.38, p=0.006), unmarried (sHR: 2.58, p<0.001), GG2 disease on initial biopsy (sHR: 1.17, p=0.048) and serum PSA level at diagnosis of 10-20 ng/ml (sHR: 2.09, p=0.032) had a significantly increased PCa mortality hazard. Patients undergoing definitive therapy with either RP or definitive XRT did not have a significantly different PCa mortality hazard (sHR 0.70, p=0.14).
Conclusions: Intermediate-term PCa mortality rates in FIR PCa patients appear to be similar to those with low risk PCa. However, there is significant within-group heterogeneity with PCa mortality rates significantly higher in PSA 10-20 FIR PCa patients.
Source of Funding: None
Methods: The Surveillance, Epidemiology, and End Results Prostate with Watchful Waiting database was used to identify men diagnosed with NCCN low or FIR PCa between 2010 and 2015, managed initially with AS. Patients in the FIR group were subdivided into three risk subgroups depending on their intermediate risk factor: Grade Group (GG) two disease, prostate-specific antigen (PSA) level 10-20 ng/ml and cT2b-c. Cumulative incidence function curves with other-cause mortality as the competing risk were utilized. Multivariable regression analyses using Fine and Gray’s semi-parametric proportional hazards model were used to assess predictors of PCa mortality.
Results: Among 70,871 patients, 48,127 (67.9%) had low and 22,744 (32.1%) had FIR disease. Median follow up was 49.0 months. There were 166 (0.2%) PCa and 3,176 (4.48%) other-cause mortalities. The five-year PCa mortality rates in the low and FIR cohorts overall were 0.29% and 0.28%, respectively (p=0.64). Within the FIR cohort, the corresponding rates were highest in the PSA 10-20 ng/ml subgroup at 0.73%, followed by 0.32% for Grade Group 2 FIR and 0.052% for cT2b-c FIR disease (p < 0.001).
On multivariable analysis, patients with Medicaid insurance (subdistribution hazard ratio [sHR]: 2.58, p=0.006), lowest SES (sHR:1.39, p=0.032), older age at diagnosis (sHR: 2.38, p=0.006), unmarried (sHR: 2.58, p<0.001), GG2 disease on initial biopsy (sHR: 1.17, p=0.048) and serum PSA level at diagnosis of 10-20 ng/ml (sHR: 2.09, p=0.032) had a significantly increased PCa mortality hazard. Patients undergoing definitive therapy with either RP or definitive XRT did not have a significantly different PCa mortality hazard (sHR 0.70, p=0.14).
Conclusions: Intermediate-term PCa mortality rates in FIR PCa patients appear to be similar to those with low risk PCa. However, there is significant within-group heterogeneity with PCa mortality rates significantly higher in PSA 10-20 FIR PCa patients.
Source of Funding: None

.jpg)
.jpg)