Back
Poster, Podium & Video Sessions
Moderated Poster
MP44: Stone Disease: Surgical Therapy (including ESWL) III
MP44-04: Real-world Practice Stone-free Rates after Ureteroscopy from a Surgical Collaborative: Much to Improve
Sunday, May 15, 2022
1:00 PM – 2:15 PM
Location: Room 228
Hyung Joon Kim*, Stephanie Daignault-Newton, John M. DiBianco, Ann Arbor, MI, S. Mohammad Jafri, Royal Oak, MI, Brian Seifman, Royal Oak, Troy, MI, Eduardo Kleer, Ypsilanti, MI, Casey A. Dauw, Khurshid R. Ghani, for the Michigan Urological Surgery Improvement Collaborative, Ann Arbor, MI
- HK
Poster Presenter(s)
Introduction: The stone-free rate (SFR) is an important outcome measure of quality after ureteroscopy for urinary stones. Recent studies show SFRs may not be as high as previously reported. However, these studies are from expert centers, and data from real-world community practice is lacking. We examined the SFR and its predictors following ureteroscopy among diverse practices in the state of Michigan.
Methods: We used the Michigan Urological Surgery Improvement Collaborative (MUSIC) Reducing Operative Complications from Kidney Stone (ROCKS) registry to identify ureteroscopy cases for renal and ureteral stone location, respectively, treated between 2016 and 2021, that had postoperative imaging. Stone-free was defined as no fragment detected on imaging within 60 days. Practice and surgeon-level SFR variation was assessed. Surgeon volume was categorized according to quartiles of annual volume. Factors associated with SFR were examined using logistic regression.
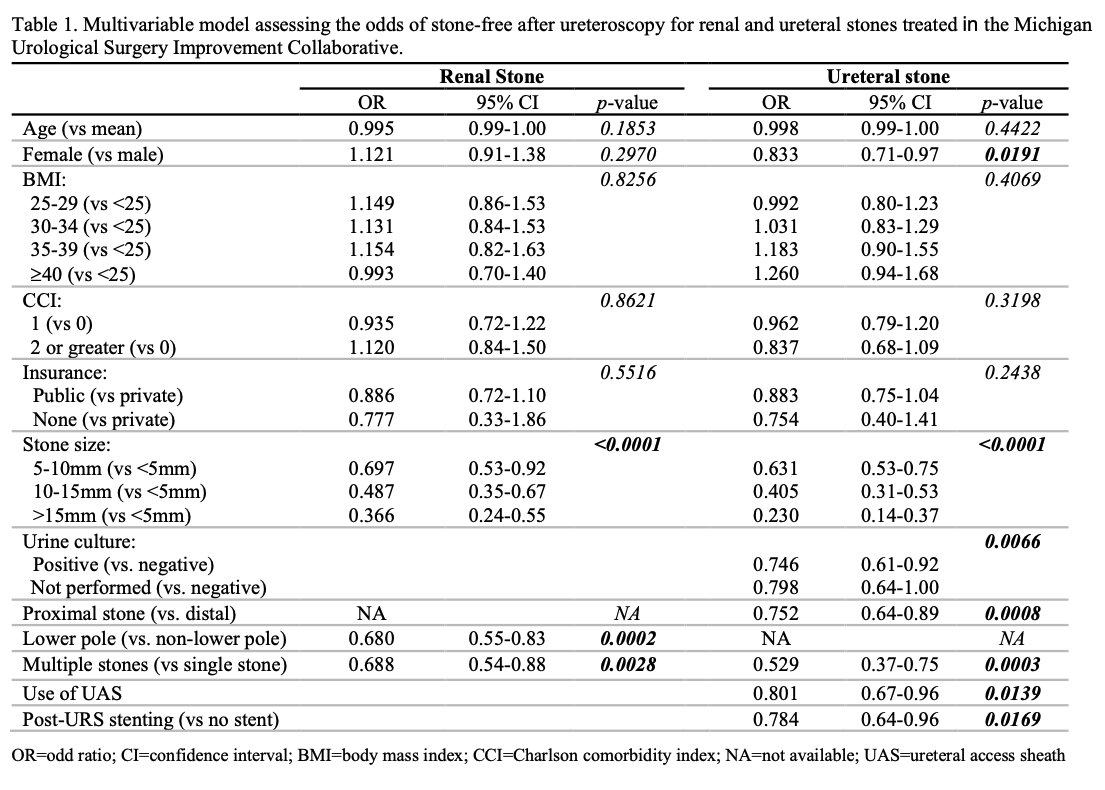
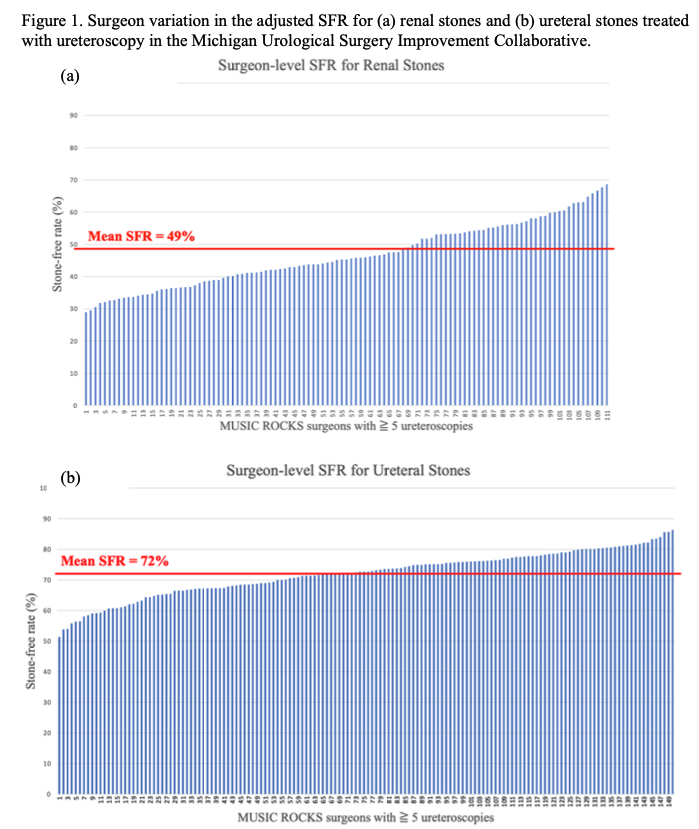
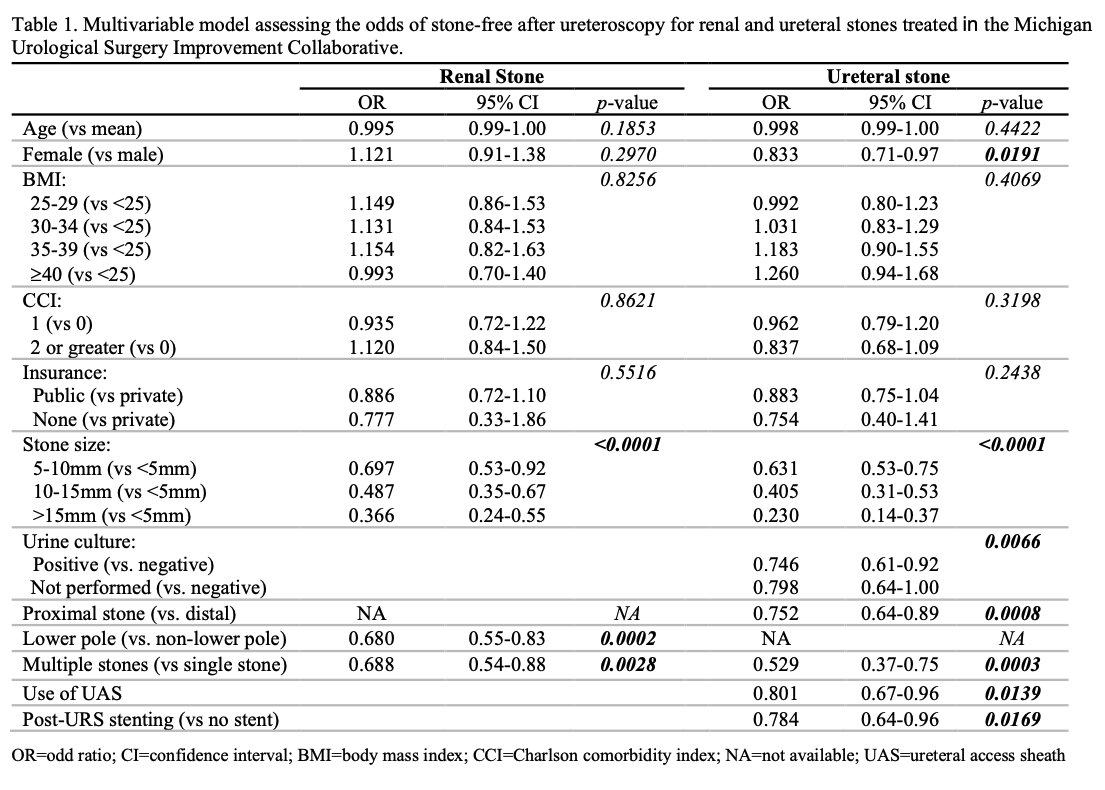
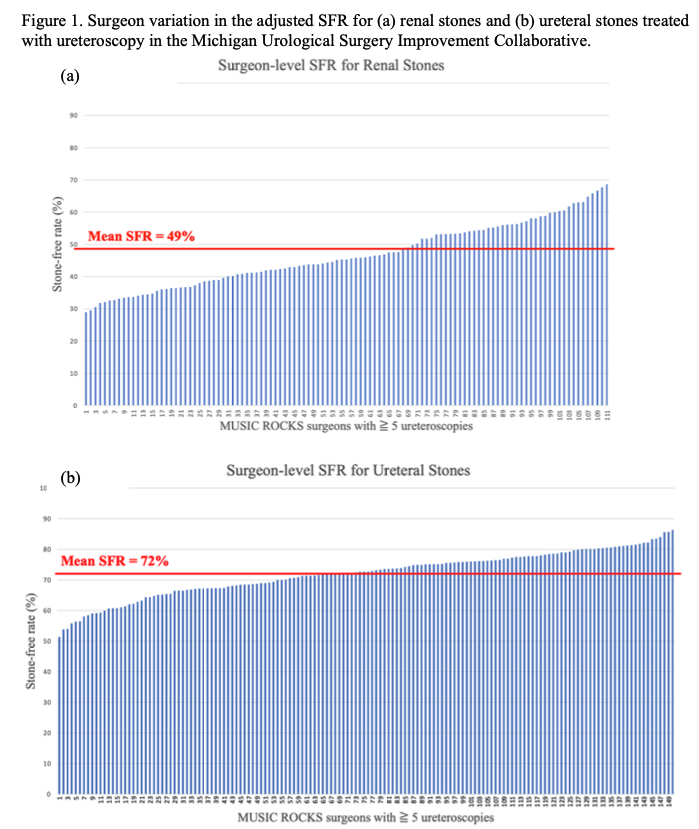
Results: 6,487 ureteroscopies were performed across 29 practices and 164 surgeons, to treat 2,091 (32.2%) renal and 4396 (67.8%) ureteral stones. The SFR was 49.6% and 72.7% for renal and ureteral stone location, respectively. For renal stones, larger stone size, lower pole location, and multiplicity were significantly associated with residual fragments (Table 1). For ureteral stones, female gender, larger stone size, proximal location, multiplicity, positive urine culture, use of ureteral access sheath, and post-ureteroscopy stenting were predictors for low SFR (Table 1). No significant differences in SFRs were identified regarding pre-stenting and surgeon volume. Surgeon variation in the SFR for renal and ureteral stones, when adjusted for risk factors, was 29.0-68.7% (p < 0.0001) and 51.4-86.4% (p < 0.0001), respectively (Figure 1).
Conclusions: There is substantial surgeon-level variation in the SFR after ureteroscopy in Michigan. Our findings demonstrate the need for quality efforts to improve these outcomes.
Source of Funding: Blue Cross Blue Shield of Michigan
Methods: We used the Michigan Urological Surgery Improvement Collaborative (MUSIC) Reducing Operative Complications from Kidney Stone (ROCKS) registry to identify ureteroscopy cases for renal and ureteral stone location, respectively, treated between 2016 and 2021, that had postoperative imaging. Stone-free was defined as no fragment detected on imaging within 60 days. Practice and surgeon-level SFR variation was assessed. Surgeon volume was categorized according to quartiles of annual volume. Factors associated with SFR were examined using logistic regression.
Results: 6,487 ureteroscopies were performed across 29 practices and 164 surgeons, to treat 2,091 (32.2%) renal and 4396 (67.8%) ureteral stones. The SFR was 49.6% and 72.7% for renal and ureteral stone location, respectively. For renal stones, larger stone size, lower pole location, and multiplicity were significantly associated with residual fragments (Table 1). For ureteral stones, female gender, larger stone size, proximal location, multiplicity, positive urine culture, use of ureteral access sheath, and post-ureteroscopy stenting were predictors for low SFR (Table 1). No significant differences in SFRs were identified regarding pre-stenting and surgeon volume. Surgeon variation in the SFR for renal and ureteral stones, when adjusted for risk factors, was 29.0-68.7% (p < 0.0001) and 51.4-86.4% (p < 0.0001), respectively (Figure 1).
Conclusions: There is substantial surgeon-level variation in the SFR after ureteroscopy in Michigan. Our findings demonstrate the need for quality efforts to improve these outcomes.
Source of Funding: Blue Cross Blue Shield of Michigan

.jpg)
.jpg)