Back
Poster, Podium & Video Sessions
Moderated Poster
MP44: Stone Disease: Surgical Therapy (including ESWL) III
MP44-06: Morbidly Obese Patients May Safely Undergo Percutaneous Nephrolithotomy at an Ambulatory Surgery Center
Sunday, May 15, 2022
1:00 PM – 2:15 PM
Location: Room 228
Max Drescher*, Baltimore, MD, Daniel Rosen, Hanover, MD, Joel Abbott, Las Vegas, NV, Julio Davalos, Hanover, MD
- MD
Poster Presenter(s)
Introduction: Obesity can pose surgical challenges in patients undergoing percutaneous nephrolithotomy (PCNL). Obesity’s association with other comorbidities as well as concern for body habitus leading to difficulties with intubation and ventilation often preclude patients above a certain Body Mass Index (BMI) from being treated in an ambulatory surgical center (ASC). We examined outcomes of morbidly obese patients treated at an ASC to see which outcomes may differ compared to non-obese patients.
Methods: Patients with BMI 40-50 underwent airway evaluation prior to clearance for ambulatory surgery. All patients underwent PCNL at a free-standing ASC. We queried our prospectively maintained database for patients with BMI>40 and compared them to patients with BMI <30. Demographic and intraoperative characteristics between the cohorts were compared using Fisher’s exact and two-tailed t tests.
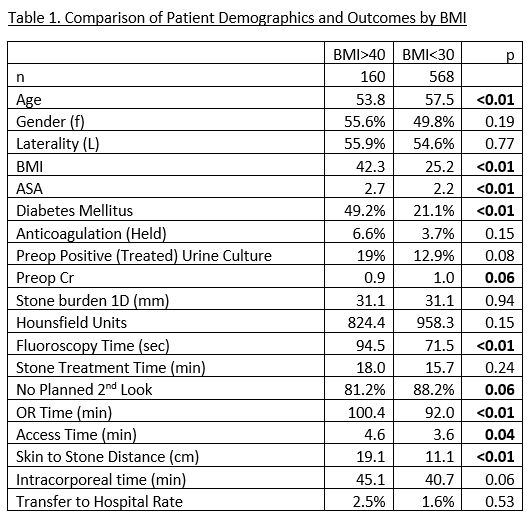
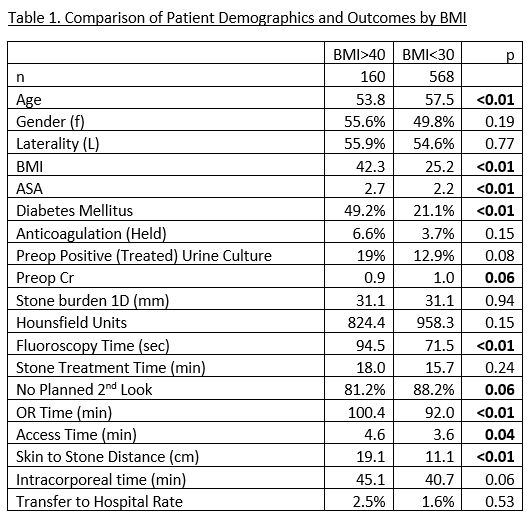
Results: 728 patients had complete data for analysis. Obese patients had higher ASA (2.7 vs. 2.2 p<0.01) and required 9% longer OR time (100 vs 92 min, p<.01), fluoroscopy time (94.5 vs. 71.5 sec, p<.01), and renal access time (4.6 vs. 3.6 min, p<.01). Obese patients did not show any significant difference in stone treatment or intracorporeal time, stone burden or stone free rate, or rate of hospital transfer. There were no airway related complications.
Conclusions: Obese patients were younger and sicker than their non-obese counterparts but required only minimal additional OR and procedure time in order to be safely treated at an ambulatory center. Patients with morbid obesity up to BMI 50, with proper screening and patient selection, can be safely treated with percutaneous nephrolithotomy at an ambulatory center.
Source of Funding: none
Methods: Patients with BMI 40-50 underwent airway evaluation prior to clearance for ambulatory surgery. All patients underwent PCNL at a free-standing ASC. We queried our prospectively maintained database for patients with BMI>40 and compared them to patients with BMI <30. Demographic and intraoperative characteristics between the cohorts were compared using Fisher’s exact and two-tailed t tests.
Results: 728 patients had complete data for analysis. Obese patients had higher ASA (2.7 vs. 2.2 p<0.01) and required 9% longer OR time (100 vs 92 min, p<.01), fluoroscopy time (94.5 vs. 71.5 sec, p<.01), and renal access time (4.6 vs. 3.6 min, p<.01). Obese patients did not show any significant difference in stone treatment or intracorporeal time, stone burden or stone free rate, or rate of hospital transfer. There were no airway related complications.
Conclusions: Obese patients were younger and sicker than their non-obese counterparts but required only minimal additional OR and procedure time in order to be safely treated at an ambulatory center. Patients with morbid obesity up to BMI 50, with proper screening and patient selection, can be safely treated with percutaneous nephrolithotomy at an ambulatory center.
Source of Funding: none

.jpg)
.jpg)