Back
Poster, Podium & Video Sessions
Moderated Poster
MP44: Stone Disease: Surgical Therapy (including ESWL) III
MP44-14: Mini-PNL facilitates same day discharge without affecting outcomes compared to standard sized PCNL
Sunday, May 15, 2022
1:00 PM – 2:15 PM
Location: Room 228
Fadl Hamouche*, Kevin Chang, Rei Unno, Greg Hosier, Heiko Yang, Justin Ahn, David Bayne, San Francisco , CA, Marshall Stoller, San Francisco, CA, Thomas Chi, San Francisco , CA
.jpg)
Fadl Hamouche, MD
Assistant Professor
McGill University
Poster Presenter(s)
Introduction: Mini-percutaneous nephrolithotomy (mPCNL) establishes a tract diameter less than the traditional 24-30 French tract in hopes of reducing perioperative hemorrhage and postoperative complications. Little prospective data exists comparing clinical outcomes between these two approaches. This study was undertaken to compare the clinical characteristics and outcomes of mini compared to standard PCNL (sPCNL).
Methods: Prospectively collected data from the Registry for Stones of the Kidney and Ureter (ReSKU) was queried on all patients who underwent PCNL at a single center from 2015-2021. Patients were divided in two cohorts based on tract dilation size, sPCNL (>/=24 French) and mPCNL( < 24 French). Demographics, clinical characteristics, and outcomes of both cohorts were compared. Statistical analysis was performed using student t test and chi square test for the univariate analysis as well as logistic regression for the multivariate analysis.
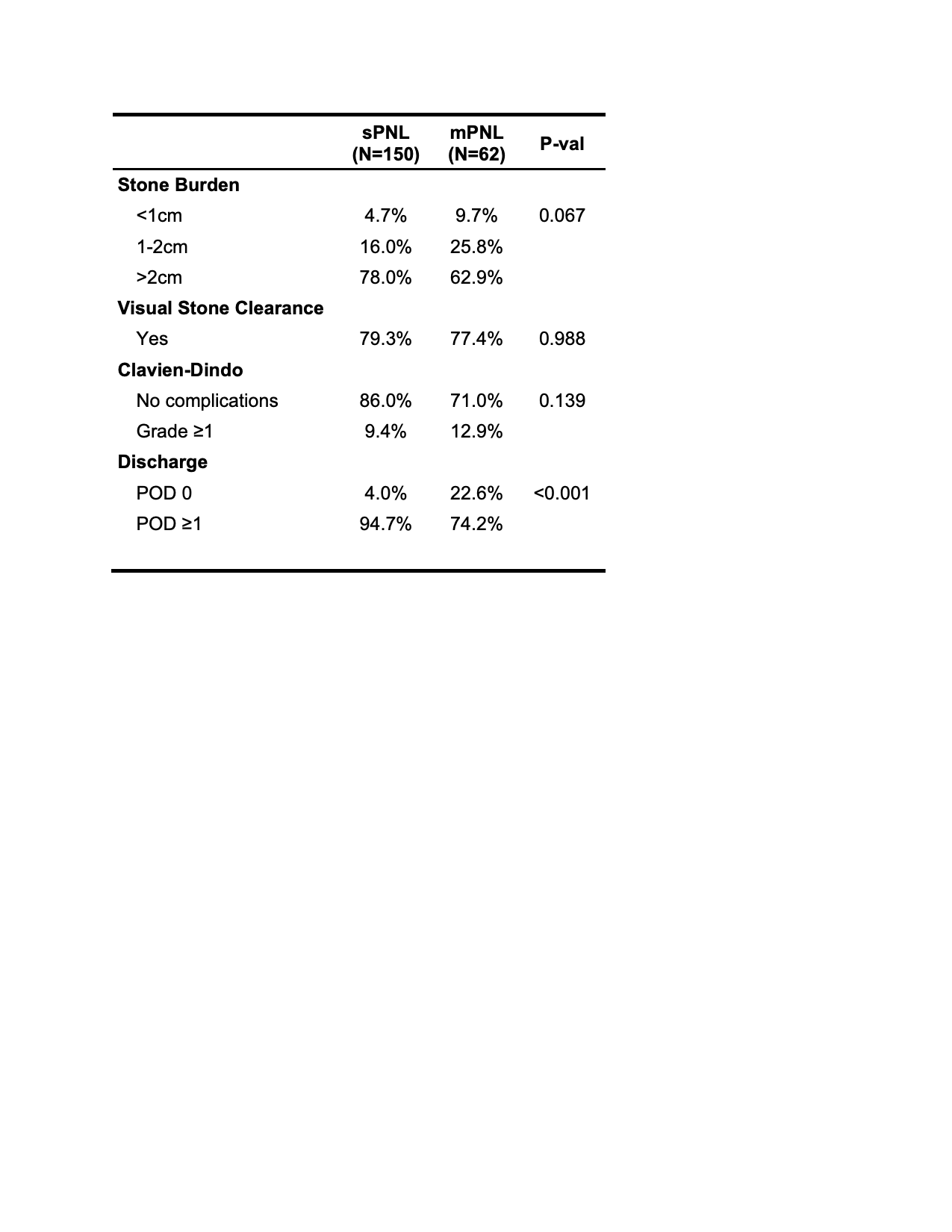
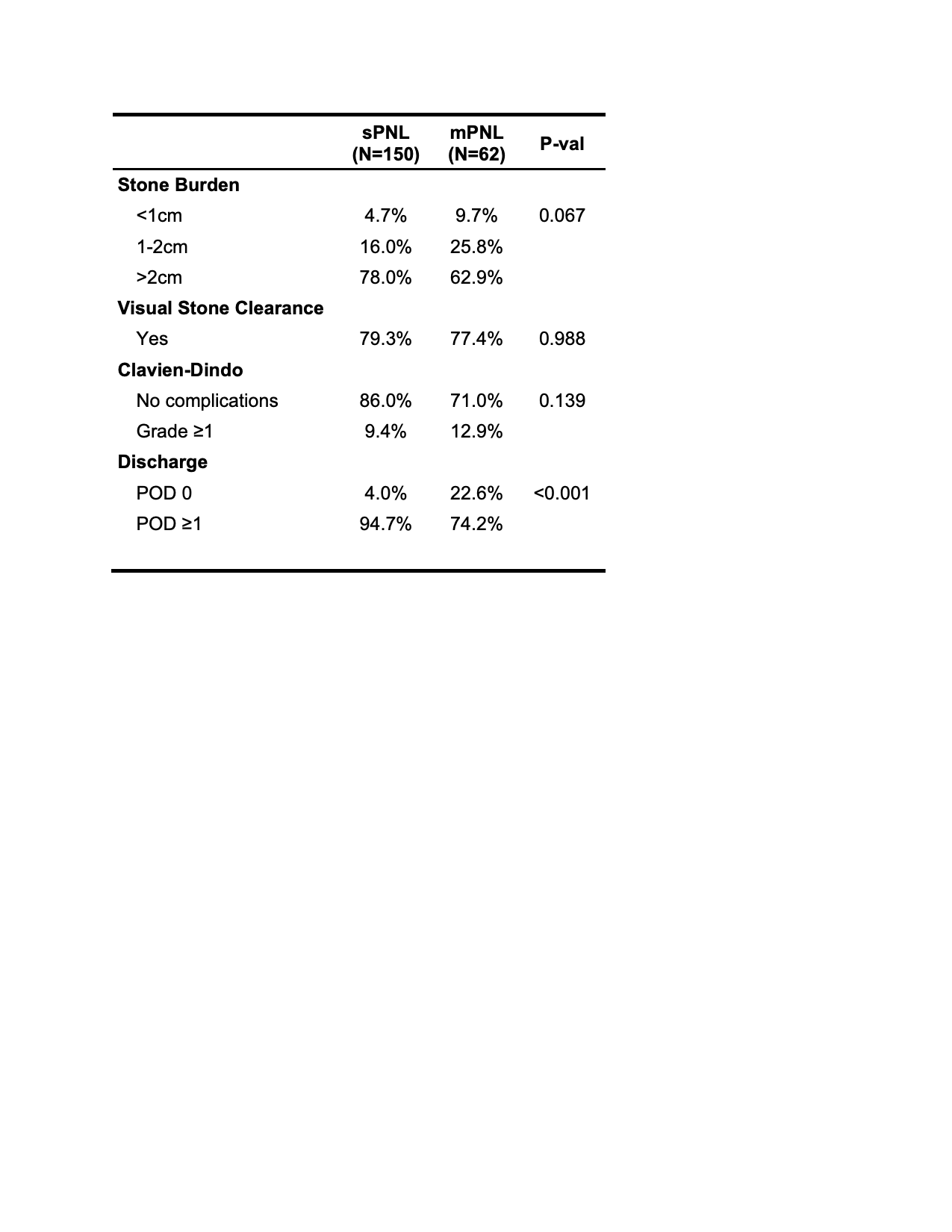
Results: 212 consecutive patients with complete operative and follow up data were included for analysis. This comprised 150 sPNL and 62 mPNL cases. Demographic data, comorbidities and ASA scores were comparable between both cohorts. The majority of patients had a stone burden larger than 2 cm in both groups (117 [78%] vs 39 [62.9%] p=0.0673). Supine positioning and ureteral stent drainage was more common in the mPCNL cohort (85 % vs 45.3% p<0.001 and 41.9% vs 6%, respectively). Percutaneous access was achieved with ultrasound guidance in the majority of patients and calyceal access location was similar between the groups. Complete visual clearance was comparable (119(79.3%) vs 48 77.4% p=0.468). Same day discharge was higher in the mPCNL cohort (14(22.6%) vs 6(4.0 %) p<0.001). There was no difference in postoperative complications or perioperative events. On multivariate analysis, post-operative drainage by a ureteral stent was also associated with discharge within 1 day of surgery in both groups (OR 0.15 (0.03-0.64) p=0.01)
Conclusions: Mini PCNL is comparable to standard PCNL in managing large kidney stones with comparable stone clearance and operative outcomes and a more favorable outpatient surgery profile. In both groups, post-operative drainage with a ureteral stent only seems to be a facilitator factor for a faster hospital discharge.
Source of Funding: Department of Urology
UCSF
Methods: Prospectively collected data from the Registry for Stones of the Kidney and Ureter (ReSKU) was queried on all patients who underwent PCNL at a single center from 2015-2021. Patients were divided in two cohorts based on tract dilation size, sPCNL (>/=24 French) and mPCNL( < 24 French). Demographics, clinical characteristics, and outcomes of both cohorts were compared. Statistical analysis was performed using student t test and chi square test for the univariate analysis as well as logistic regression for the multivariate analysis.
Results: 212 consecutive patients with complete operative and follow up data were included for analysis. This comprised 150 sPNL and 62 mPNL cases. Demographic data, comorbidities and ASA scores were comparable between both cohorts. The majority of patients had a stone burden larger than 2 cm in both groups (117 [78%] vs 39 [62.9%] p=0.0673). Supine positioning and ureteral stent drainage was more common in the mPCNL cohort (85 % vs 45.3% p<0.001 and 41.9% vs 6%, respectively). Percutaneous access was achieved with ultrasound guidance in the majority of patients and calyceal access location was similar between the groups. Complete visual clearance was comparable (119(79.3%) vs 48 77.4% p=0.468). Same day discharge was higher in the mPCNL cohort (14(22.6%) vs 6(4.0 %) p<0.001). There was no difference in postoperative complications or perioperative events. On multivariate analysis, post-operative drainage by a ureteral stent was also associated with discharge within 1 day of surgery in both groups (OR 0.15 (0.03-0.64) p=0.01)
Conclusions: Mini PCNL is comparable to standard PCNL in managing large kidney stones with comparable stone clearance and operative outcomes and a more favorable outpatient surgery profile. In both groups, post-operative drainage with a ureteral stent only seems to be a facilitator factor for a faster hospital discharge.
Source of Funding: Department of Urology
UCSF

.jpg)
.jpg)