Back
Poster, Podium & Video Sessions
Moderated Poster
MP44: Stone Disease: Surgical Therapy (including ESWL) III
MP44-20: Comparison of ultra-mini percutaneous nephrolithotomy and retrograde intrarenal surgery for renal stones: A systematic review and meta-analysis from KSER update series
Sunday, May 15, 2022
1:00 PM – 2:15 PM
Location: Room 228
Hae Do Jung*, Gunpo, Korea, Republic of, Doo Yong Chung, Incheon, Korea, Republic of, Min Ho Lee, Changwon, Korea, Republic of, Do Kyung Kim, Sin Woo Lee, Sunghyun Paick, Seung Hyun Jeon, Joo Yong Lee, Seoul, Korea, Republic of
- HJ
Poster Presenter(s)
Introduction: This study aims to compare the therapeutic effect and safety of ultra-mini percutaneous nephrolithotomy (UMPCNL) and retrograde intrarenal surgery (RIRS) for renal stones through updated systematic review and meta-analysis.
Methods: We searched clinical trials comparing UMPCNL and RIRS for renal stones from PubMed, EMBASE, and the Cochrane Library up to March 2021. Stone-free rate (SFR), complication rate, operative time, and hospital stay were analyzed. We also conducted a sub-analysis of lower pole renal stones in two groups.
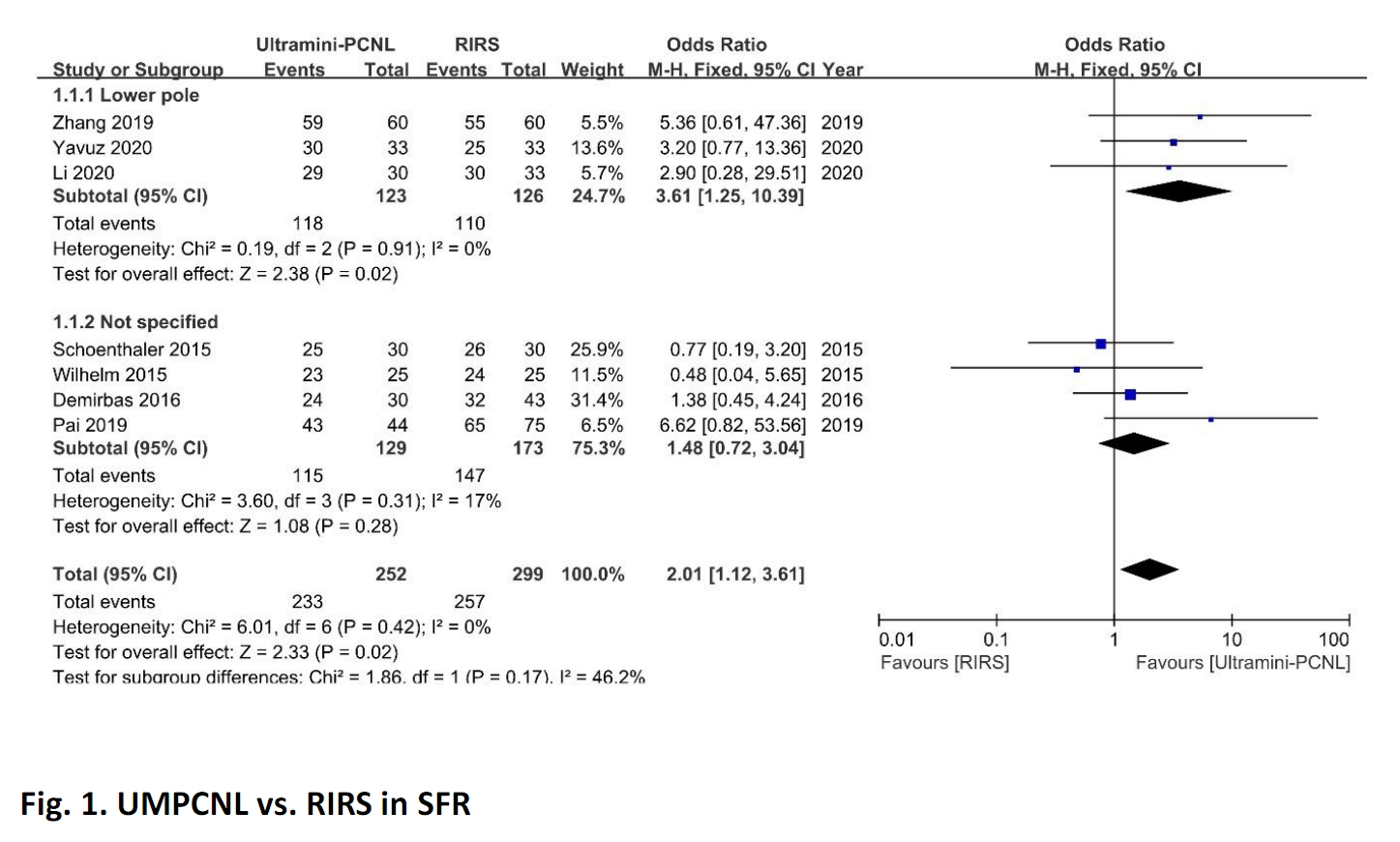
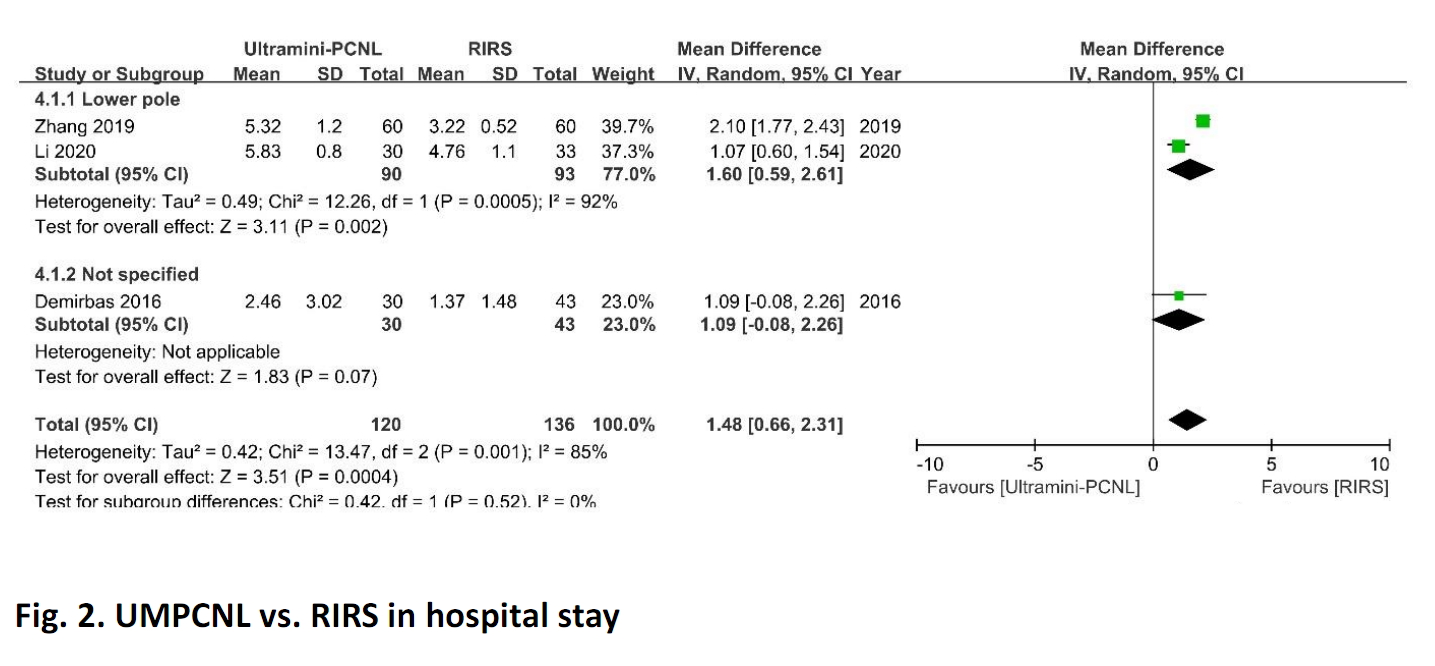
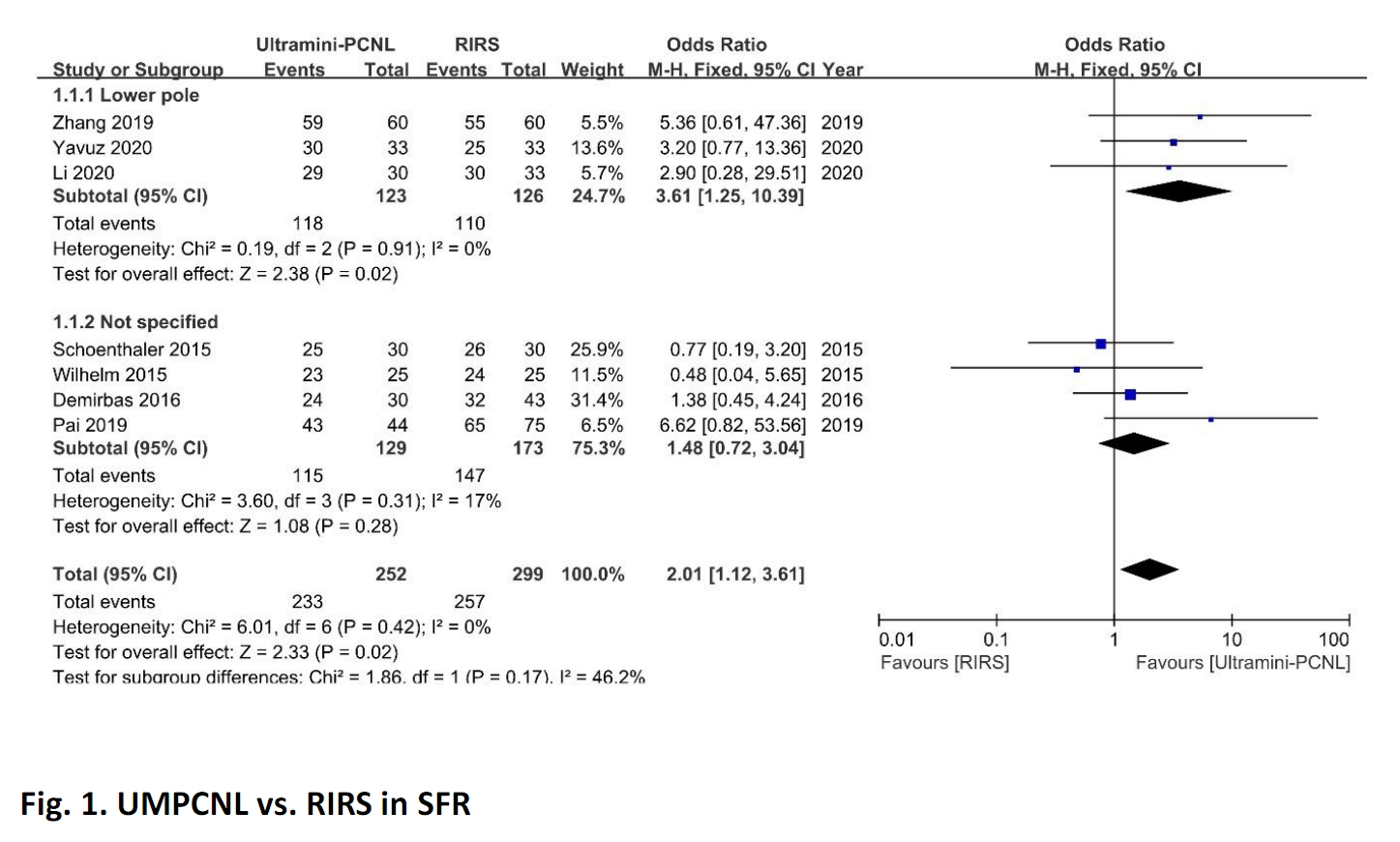
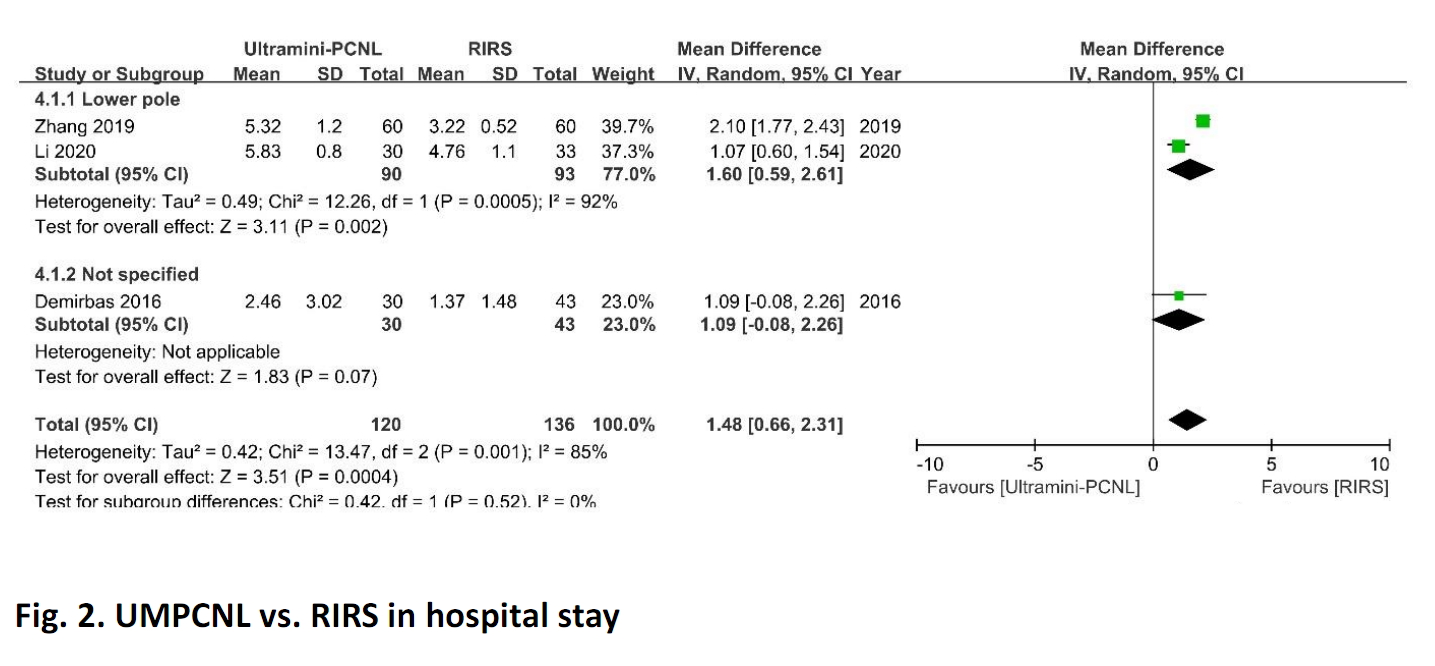
Results: Seven studies were finally included in the current study. The location of renal stones was a lower pole in three studies, not specified in four studies. The size of renal stones was 10-20 mm in three studies, 10-25 mm in one study, 10-35 mm in two studies, not specified in one study. The SFR of UMPCNL was higher in the lower pole (p=0.02, OR 3.61, 95% CI 1.25-10.39) and all location (p=0.02, OR 2.01, 95% CI 1.12-3.61) than RIRS (Fig. 1). The complication rate did not show any significant difference between UMPCNL and RIRS regardless of the location of renal stones (lower pole: p=0.31, OR 1.49, 95% CI 0.69-3.21; total: p=0.22, OR 1.52, 95% CI 0.77-2.98). In operative time, UMPCNL was shorter than RIRS in total (p=0.005, OR -15.63, 95% CI -26.60--4.67), but there was no difference in the lower pole (p=0.07, OR -20.91, 95% CI -43.87-2.06). In hospital stay, UMPCNL was significantly longer in the lower pole and total than RIRS (p=0.002, OR 1.60, 95% CI 0.59-2.61; p=0.0004, OR 1.48, 95% CI 0.66-2.31, respectively) (Fig. 2).
Conclusions: Compared to RIRS, UMPCNL has a higher SFR in the lower pole and total, shorter operative time in total. RIRS showed a shorter hospital stay in the lower pole and total. The complication rate was not different between UMPCNL and RIRS in the lower pole and total.
Source of Funding: None.
Methods: We searched clinical trials comparing UMPCNL and RIRS for renal stones from PubMed, EMBASE, and the Cochrane Library up to March 2021. Stone-free rate (SFR), complication rate, operative time, and hospital stay were analyzed. We also conducted a sub-analysis of lower pole renal stones in two groups.
Results: Seven studies were finally included in the current study. The location of renal stones was a lower pole in three studies, not specified in four studies. The size of renal stones was 10-20 mm in three studies, 10-25 mm in one study, 10-35 mm in two studies, not specified in one study. The SFR of UMPCNL was higher in the lower pole (p=0.02, OR 3.61, 95% CI 1.25-10.39) and all location (p=0.02, OR 2.01, 95% CI 1.12-3.61) than RIRS (Fig. 1). The complication rate did not show any significant difference between UMPCNL and RIRS regardless of the location of renal stones (lower pole: p=0.31, OR 1.49, 95% CI 0.69-3.21; total: p=0.22, OR 1.52, 95% CI 0.77-2.98). In operative time, UMPCNL was shorter than RIRS in total (p=0.005, OR -15.63, 95% CI -26.60--4.67), but there was no difference in the lower pole (p=0.07, OR -20.91, 95% CI -43.87-2.06). In hospital stay, UMPCNL was significantly longer in the lower pole and total than RIRS (p=0.002, OR 1.60, 95% CI 0.59-2.61; p=0.0004, OR 1.48, 95% CI 0.66-2.31, respectively) (Fig. 2).
Conclusions: Compared to RIRS, UMPCNL has a higher SFR in the lower pole and total, shorter operative time in total. RIRS showed a shorter hospital stay in the lower pole and total. The complication rate was not different between UMPCNL and RIRS in the lower pole and total.
Source of Funding: None.

.jpg)
.jpg)