Back
Poster, Podium & Video Sessions
Moderated Poster
MP46: Penile & Testicular Cancer I
MP46-06: Trends in Perioperative Outcomes Following Midline Extraperitoneal Retroperitoneal Lymph Node Dissection: Single Tertiary Center Experience
Sunday, May 15, 2022
1:00 PM – 2:15 PM
Location: Room 222
Hamed Ahmadi, Muhannad Alsyouf*, Madeleine Burg, Arman Ashrafi, Sidney Roberts, Sanam Ladi Seyedian, Alireza Ghoreifi, Antoin Douglawi, Sumeet Bhanvadia, Hooman Djaladat, Anne Schuckman, Siamak Daneshmand, Los Angeles, CA
- MA
Muhannad Alsyouf, MD
University of Southern California
Poster Presenter(s)
Introduction: Median length of hospital stay (LOS) following transperitoneal retroperitoneal lymph node dissection is 3-4 days at centers of excellence. The midline extraperitoneal approach for retroperitoneal lymph node dissection (EP-RPLND) has been associated with reduced morbidity including shorter LOS compared to transperitoneal approach. The objective of the study was to evaluate the characteristics and outcomes of patients who underwent EP-RPLND and discharged after an overnight hospital stay.
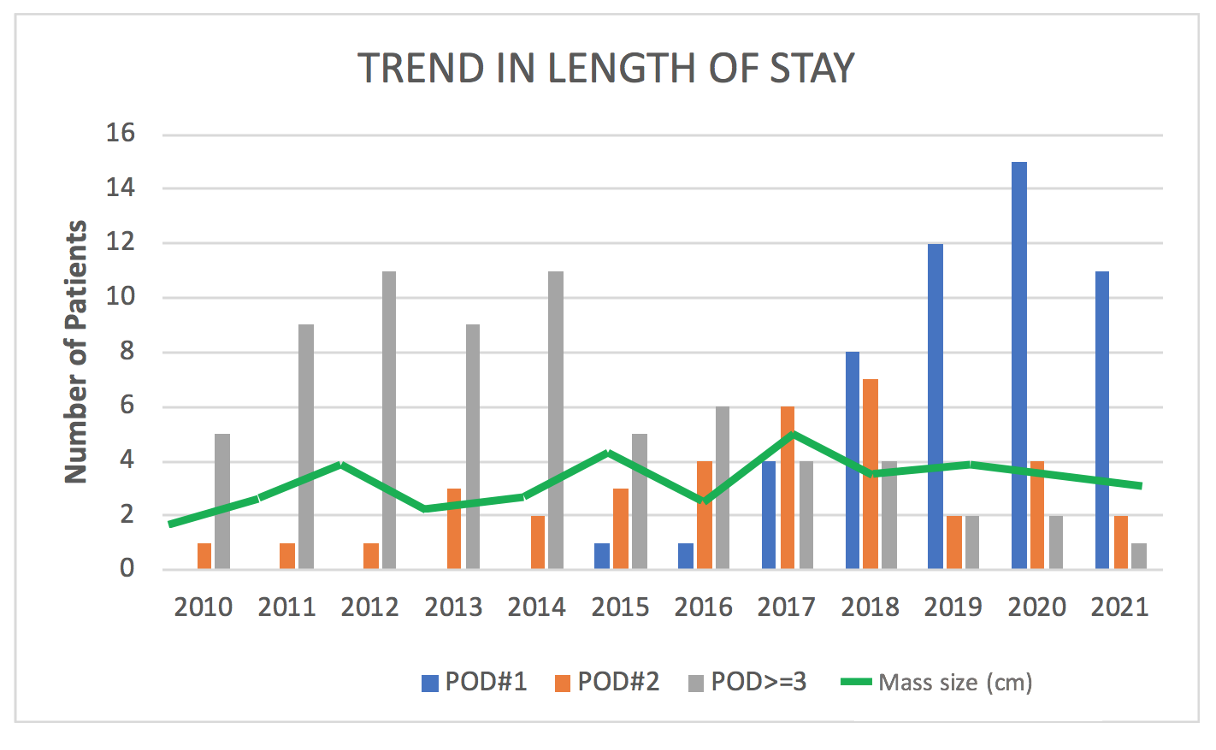
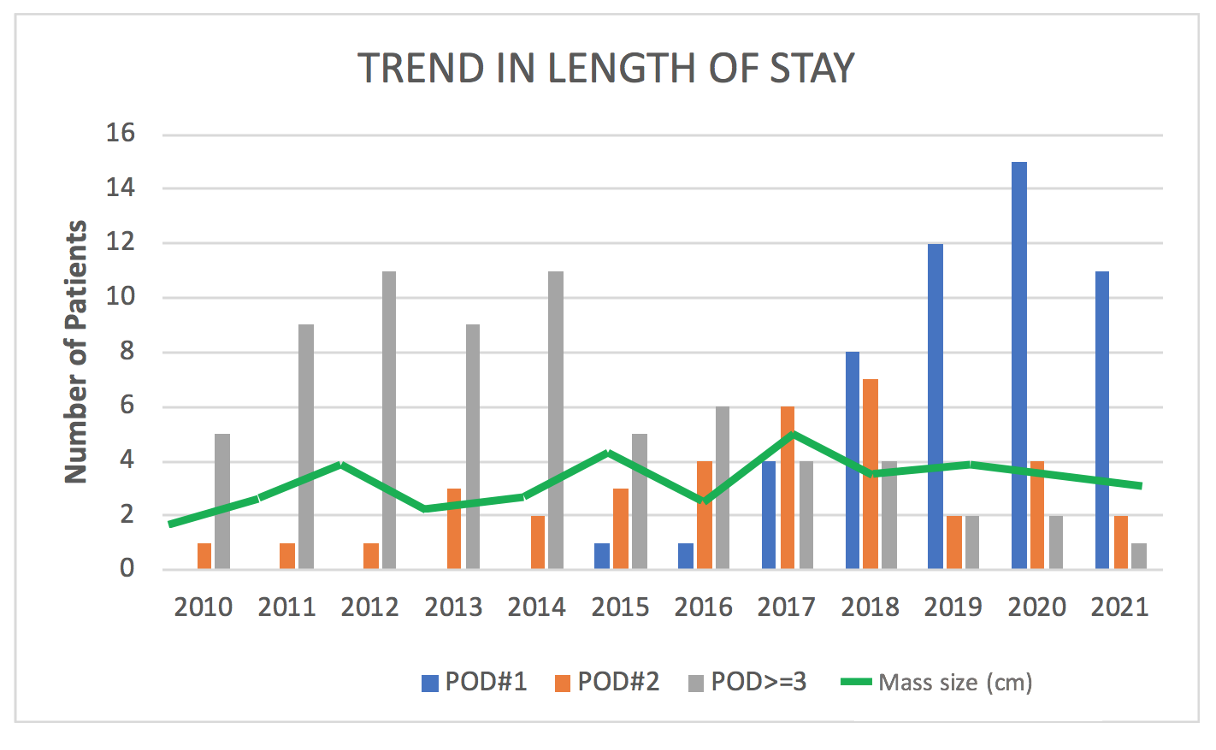
Methods: A retrospective review of all patients with GCT who underwent EP-RPLND between 2010 to 2021 were reviewed. Trends in LOS, retroperitoneal mass size, and complications overtime were assessed. Perioperative and functional outcome of patients who were discharged on POD #1 after EP-RPLND were described and compared to patients with >2 day hospital stay. Univariate & multivariate analysis were performed, with p<0.05 considered significant.
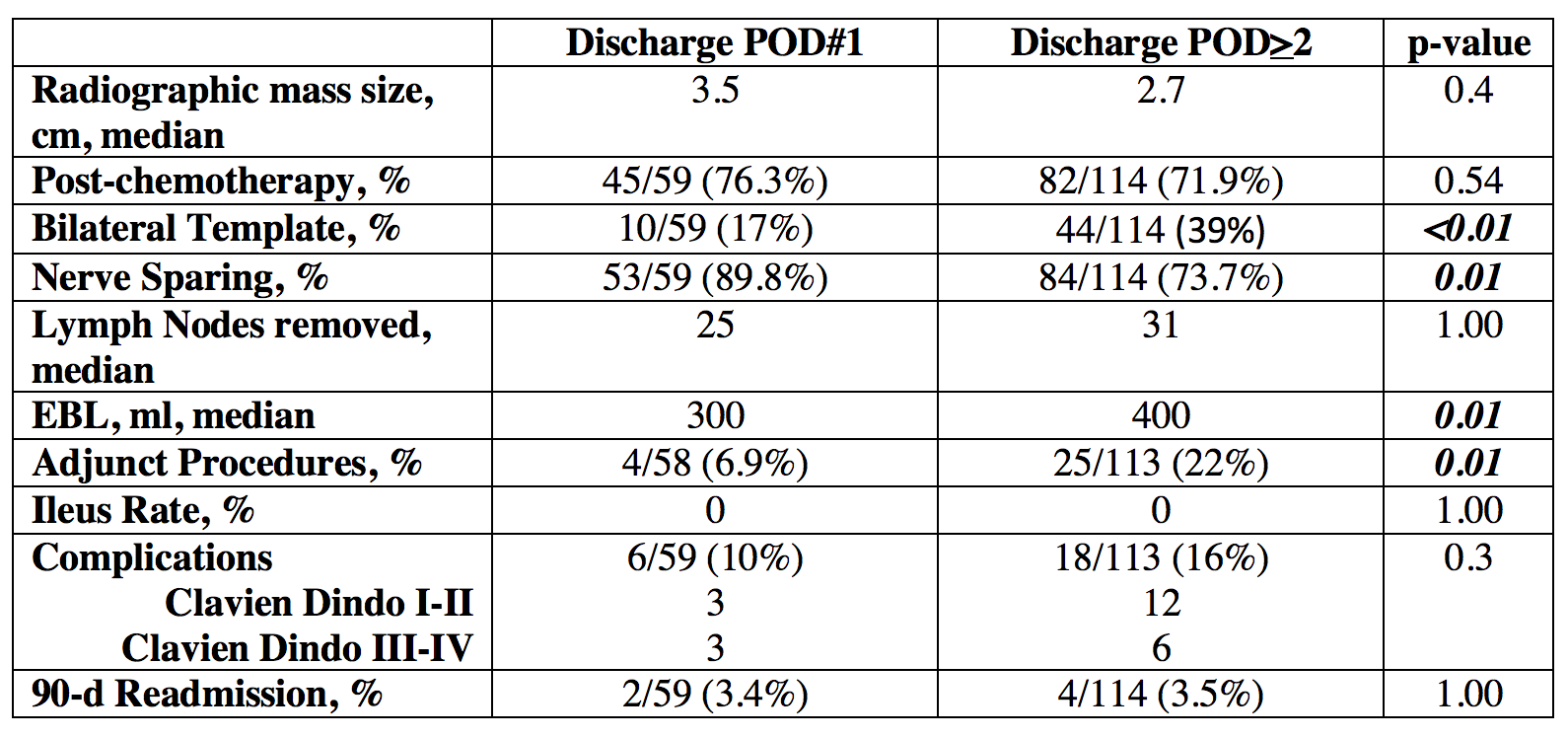
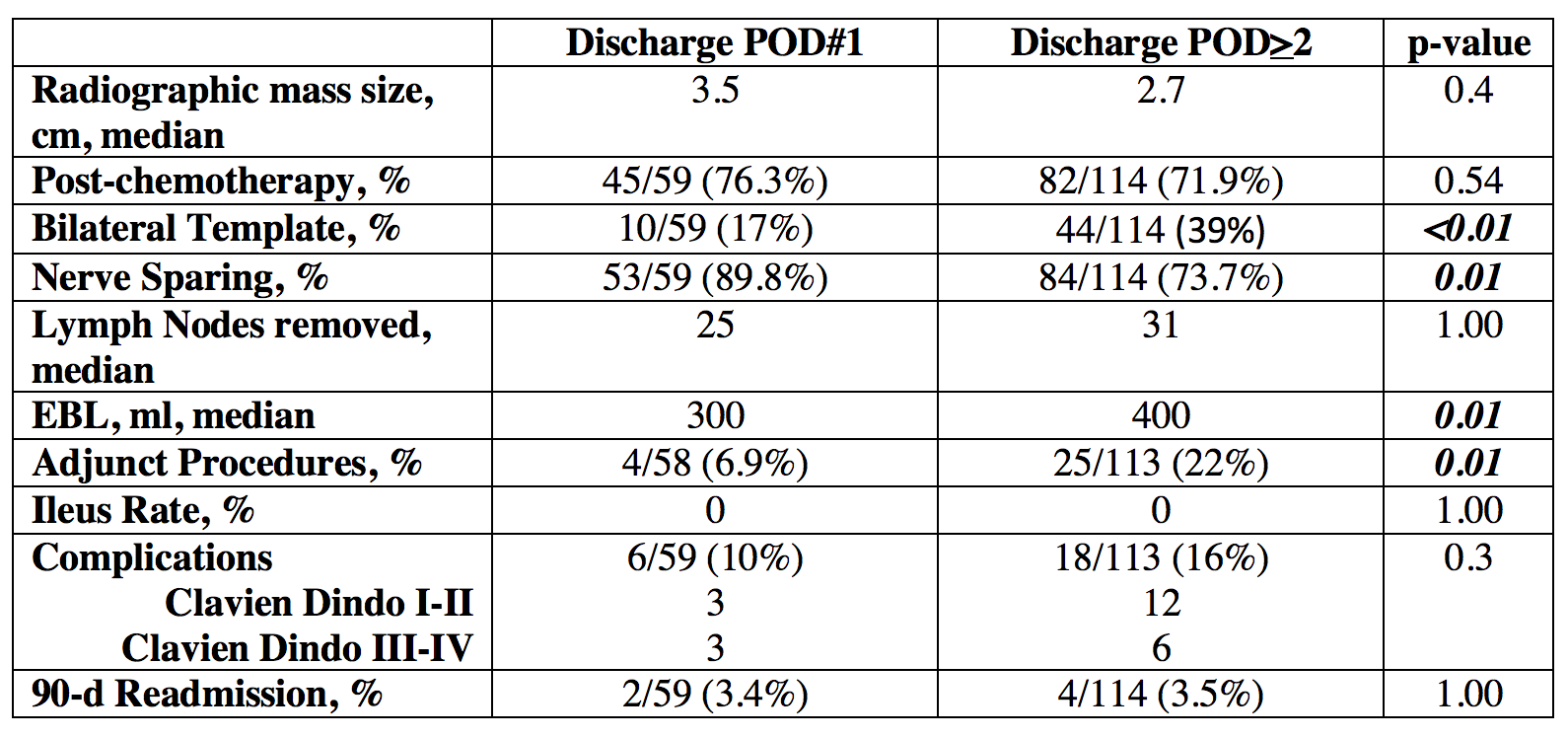
Results: Overall, 172 patients underwent EP-RPLND with a median LOS of 2 (IQR, 1 – 3) days and retroperitoneal mass size of 3.2 (IQR, 2 – 5.4) cm. Overall, 59/172 (34%) of patients were discharged on POD#1 including 45/59 patients who underwent post-chemotherapy EP-RPLND. A significantly higher proportion of EP-RPLND patients were discharged on POD#1 from 2015-2021 compared to 2010-2015 (53 vs 1.6%; p<0.01) (Figure). No patient who underwent EP-RPLND developed post-operative ileus. There was no difference in mass size, post-chemotherapy RPLND rates, number of lymph nodes removed, complications, or readmissions between patients who were discharged on POD#1 compared to patients discharged on POD#>2 (Table). On multivariate analysis, year of surgery (HR 2.1, CI 1.6-2.7) and unilateral template RPLND (HR 5.8, CI 2-16.4) were predictive of hospital discharge on POD#1.
Conclusions: Evolving experience with EP-RPLND demonstrates that overnight stay is feasible. In well-selected patients, overnight stay following EP-RPLND is associated with low complication and readmission rates.
Source of Funding: None
Methods: A retrospective review of all patients with GCT who underwent EP-RPLND between 2010 to 2021 were reviewed. Trends in LOS, retroperitoneal mass size, and complications overtime were assessed. Perioperative and functional outcome of patients who were discharged on POD #1 after EP-RPLND were described and compared to patients with >2 day hospital stay. Univariate & multivariate analysis were performed, with p<0.05 considered significant.
Results: Overall, 172 patients underwent EP-RPLND with a median LOS of 2 (IQR, 1 – 3) days and retroperitoneal mass size of 3.2 (IQR, 2 – 5.4) cm. Overall, 59/172 (34%) of patients were discharged on POD#1 including 45/59 patients who underwent post-chemotherapy EP-RPLND. A significantly higher proportion of EP-RPLND patients were discharged on POD#1 from 2015-2021 compared to 2010-2015 (53 vs 1.6%; p<0.01) (Figure). No patient who underwent EP-RPLND developed post-operative ileus. There was no difference in mass size, post-chemotherapy RPLND rates, number of lymph nodes removed, complications, or readmissions between patients who were discharged on POD#1 compared to patients discharged on POD#>2 (Table). On multivariate analysis, year of surgery (HR 2.1, CI 1.6-2.7) and unilateral template RPLND (HR 5.8, CI 2-16.4) were predictive of hospital discharge on POD#1.
Conclusions: Evolving experience with EP-RPLND demonstrates that overnight stay is feasible. In well-selected patients, overnight stay following EP-RPLND is associated with low complication and readmission rates.
Source of Funding: None

.jpg)
.jpg)