Back
Poster, Podium & Video Sessions
Moderated Poster
MP46: Penile & Testicular Cancer I
MP46-12: Declines in Skeletal Muscle Mass and Quality During Cytotoxic Chemotherapy Predict Increased Risk of Chemotherapy-Associated Adverse Events in Men with Testis Cancer
Sunday, May 15, 2022
1:00 PM – 2:15 PM
Location: Room 222
Anthea Phuong*, Seattle, WA, J. Peter Marquardt, Florian J. Fintelmann, Boston, MA, Ryan O'Malley, Grace Laidlaw, Zachary Eagle, Steven Ngo, Sarah Holt, Delaney Orcutt, George R. Schade, Daniel W. Lin, Michael T. Schweizer, Todd Yezefski, Evan Y. Yu, Bruce Montgomery, Petros Grivas, Sarah Psutka, Seattle, WA
- AP
Anthea Phuong, BS
University of Washington
Poster Presenter(s)
Introduction: Baseline muscle mass (skeletal muscle index, SMI) is associated with therapeutic response across malignancies. The novel concept of skeletal muscle gauge (SMG= SMI*skeletal muscle density (SMD)) has been proposed as a surrogate for muscle quality and quantity. To date, the impact of cytotoxic chemotherapy (CC) on SMI and SMG in germ cell carcinoma of testis (GCT) remains undescribed. Herein, our objective was to measure changes in SMI and SMG in men with testis cancer undergoing CC and evaluate potential association between these measures and chemotherapy-associated adverse events (AE).
Methods: All consecutive men undergoing CC for GCT (2005-18) were retrospectively reviewed. Third Lumbar SMI (cm2/m2) and SMD (HU) were obtained using validated methodology on axial computed tomography (CT) images within 75 days prior to the start (T1) and after the end (T2) of CC from which SMG was calculated. Changes in SMI, SMD, and SMG were quantified and associations with grade 1-5 AEs (CTCAE v.5) were estimated with multivariable logistic regression adjusted for age, ECOG performance status, Charlson Comorbidity Index, CC regimen, GCT stage.
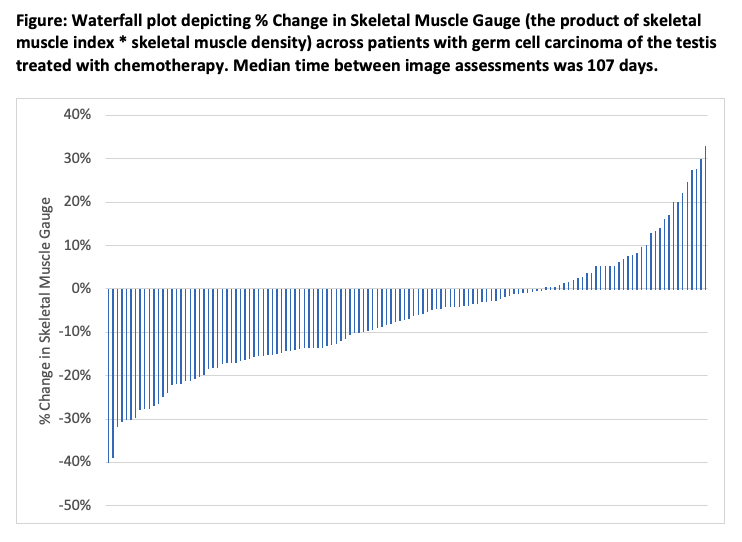
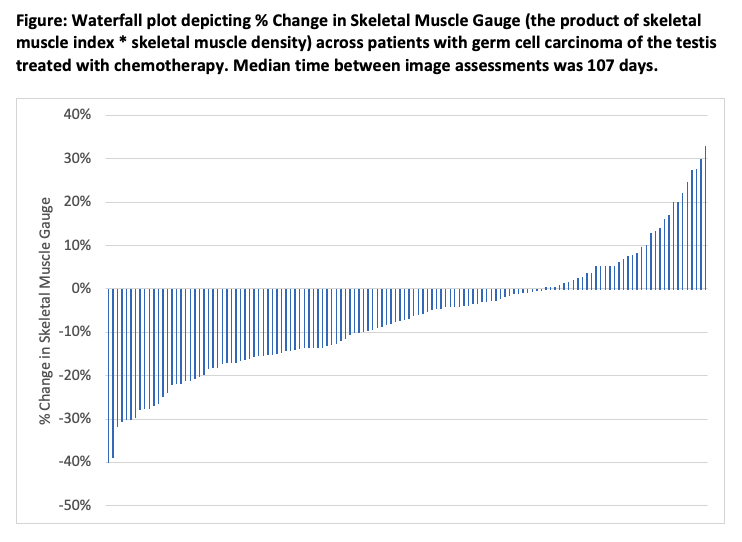
Results: This study of 141 men with median age of 30 years (IQR 25-39) included 61% with nonseminomatous GCT. Tumors were classified as Stage IS, II, and III GCT in 21%, 41%, and 38%, respectively. CC regimens included BEP (68%), EP (17%), VIP (8%), and other (6%) with median of 3-cycles; 90% of patients completed planned CC. Median time between CTs was 107 days. Median SMI-T1 and -T2 were 57.9 and 55.3 cm2/m2 (?SMI -6%), median SMD-T1 and -T2 were 57 and 54 HU (?SMD -2%), and median SMG-T1 and -T2 were 3256 and 3059 (?SMG -6%, Figure). Overall, 120 men (85%) experienced at least one AE. While T1 and T2 SMI, SMD, and SMG were not significantly associated with AEs (p>0.05 for all), ?SMI (p=0.002) and ?SMG (p=0.02) were independently associated with higher AE incidence.
Conclusions: Changes in muscle mass and quality following CC were associated with higher risk of AE in men with GCT undergoing CC. This association may represent evidence of toxicity. Further work is needed to understand the risk factors for loss of muscle mass and quality during CC, implications for AEs and clinical outcomes following subsequent surgery. Limitations include retrospective nature, selection and confounding bias.
Source of Funding: none
Methods: All consecutive men undergoing CC for GCT (2005-18) were retrospectively reviewed. Third Lumbar SMI (cm2/m2) and SMD (HU) were obtained using validated methodology on axial computed tomography (CT) images within 75 days prior to the start (T1) and after the end (T2) of CC from which SMG was calculated. Changes in SMI, SMD, and SMG were quantified and associations with grade 1-5 AEs (CTCAE v.5) were estimated with multivariable logistic regression adjusted for age, ECOG performance status, Charlson Comorbidity Index, CC regimen, GCT stage.
Results: This study of 141 men with median age of 30 years (IQR 25-39) included 61% with nonseminomatous GCT. Tumors were classified as Stage IS, II, and III GCT in 21%, 41%, and 38%, respectively. CC regimens included BEP (68%), EP (17%), VIP (8%), and other (6%) with median of 3-cycles; 90% of patients completed planned CC. Median time between CTs was 107 days. Median SMI-T1 and -T2 were 57.9 and 55.3 cm2/m2 (?SMI -6%), median SMD-T1 and -T2 were 57 and 54 HU (?SMD -2%), and median SMG-T1 and -T2 were 3256 and 3059 (?SMG -6%, Figure). Overall, 120 men (85%) experienced at least one AE. While T1 and T2 SMI, SMD, and SMG were not significantly associated with AEs (p>0.05 for all), ?SMI (p=0.002) and ?SMG (p=0.02) were independently associated with higher AE incidence.
Conclusions: Changes in muscle mass and quality following CC were associated with higher risk of AE in men with GCT undergoing CC. This association may represent evidence of toxicity. Further work is needed to understand the risk factors for loss of muscle mass and quality during CC, implications for AEs and clinical outcomes following subsequent surgery. Limitations include retrospective nature, selection and confounding bias.
Source of Funding: none

.jpg)
.jpg)