Back
Poster, Podium & Video Sessions
Best Poster Award
MP47: Kidney Cancer: Epidemiology & Evaluation/Staging/Surveillance III
MP47-04: Validation of a 22-Gene Epithelial-Mesenchymal Transition (EMT) Prognostic Signature in Clear Cell Renal Cell Carcinoma
Sunday, May 15, 2022
2:45 PM – 4:00 PM
Location: Room 228
Brittney Cotta*, Srinivas Nallandhighal, Ann Arbor, MI, Judith Stangl-Kremser, Vienna, Austria, Trinh Pham, Ann Arbor, MI, Jeffrey Tosoian, Nashville, TN, Kathryn Marchetti, Joel Berends, Mahir Maruf, Scott Tomlins, Todd Morgan, Ganesh Palapattu, Eman Abdulfatah, Aaron Udager, Simpa Salami, Ann Arbor, MI
- BC
Poster Presenter(s)
Introduction: Current predictors of metastatic progression after radical nephrectomy for localized clear cell renal cell carcinoma (ccRCC) include clinicopathologic features such as tumor stage and grade. The addition of molecular tumor characteristics in a prognostic score may improve risk stratification and patient selection for enhanced follow up strategies or adjuvant therapies.
Methods: We retrospectively identified consecutive patients with ccRCC who underwent radical nephrectomy (RNx) for localized disease. Those who developed metastasis were identified. Whole-transcriptome mRNA sequencing of primary tumors was performed followed by gene set enrichment analysis (GSEA) for the most significant cancer hallmark pathways enriched in patients who did or did not develop metastasis. For each patient, the 22-gene epithelial mesenchymal transition (EMT) score was calculated (high vs. low), using cut-offs from a prior study using TCGA data. The prognostic impact of the EMT score was evaluated by performing multivariable cox-proportional hazard testing and Kaplan-Meier (KM) survival analysis.
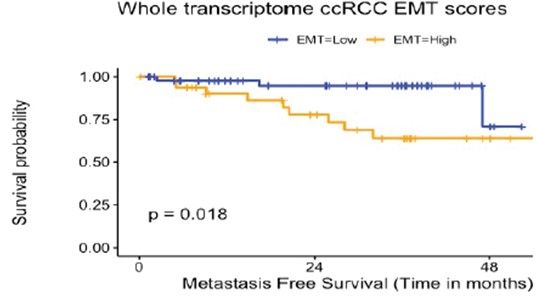
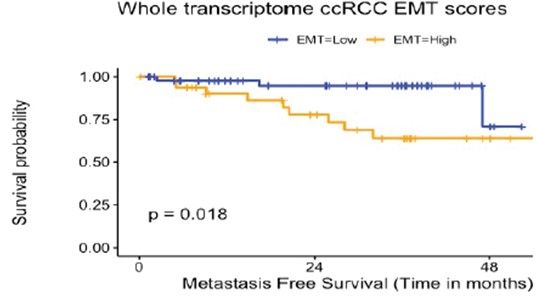
Results: We analyzed 82 patients with median age 62 years and median tumor size 6 ±2.9 cm. The median time to metastasis after radical nephrectomy for patients who developed metastasis (n=12) was 18.2 months and median follow up 31.1 months for patients who did not develop metastasis (n=70). We observed a significant enrichment of EMT, myogenesis, inflammatory response and hypoxia hallmark pathways in patients with metastasis vs. those without metastasis. Kaplan-Meier survival analysis showed a significant decrease in metastasis-free survival in patients with a high EMT score (p=0.018). Multivariable analysis controlling for relevant clinicopathologic features such as age, sex, tumor size, tumor stage etc. revealed high EMT score to be significantly associated with development of metastasis [hazard ratio (HR) 7.2; 95% CI 1.15-44.8; p=0.035].
Conclusions: We validated a prognostic 22-gene epithelial mesenchymal transition (EMT) score in patients treated with radical nephrectomy for localized ccRCC. Pending further studies, the EMT score may improve risk stratification and select patients for adjuvant therapy.
Source of Funding: UM-Peking University Joint Institute, NCI T32
Methods: We retrospectively identified consecutive patients with ccRCC who underwent radical nephrectomy (RNx) for localized disease. Those who developed metastasis were identified. Whole-transcriptome mRNA sequencing of primary tumors was performed followed by gene set enrichment analysis (GSEA) for the most significant cancer hallmark pathways enriched in patients who did or did not develop metastasis. For each patient, the 22-gene epithelial mesenchymal transition (EMT) score was calculated (high vs. low), using cut-offs from a prior study using TCGA data. The prognostic impact of the EMT score was evaluated by performing multivariable cox-proportional hazard testing and Kaplan-Meier (KM) survival analysis.
Results: We analyzed 82 patients with median age 62 years and median tumor size 6 ±2.9 cm. The median time to metastasis after radical nephrectomy for patients who developed metastasis (n=12) was 18.2 months and median follow up 31.1 months for patients who did not develop metastasis (n=70). We observed a significant enrichment of EMT, myogenesis, inflammatory response and hypoxia hallmark pathways in patients with metastasis vs. those without metastasis. Kaplan-Meier survival analysis showed a significant decrease in metastasis-free survival in patients with a high EMT score (p=0.018). Multivariable analysis controlling for relevant clinicopathologic features such as age, sex, tumor size, tumor stage etc. revealed high EMT score to be significantly associated with development of metastasis [hazard ratio (HR) 7.2; 95% CI 1.15-44.8; p=0.035].
Conclusions: We validated a prognostic 22-gene epithelial mesenchymal transition (EMT) score in patients treated with radical nephrectomy for localized ccRCC. Pending further studies, the EMT score may improve risk stratification and select patients for adjuvant therapy.
Source of Funding: UM-Peking University Joint Institute, NCI T32

.jpg)
.jpg)