Back
Poster, Podium & Video Sessions
Moderated Poster
MP47: Kidney Cancer: Epidemiology & Evaluation/Staging/Surveillance III
MP47-06: Assessing renal mass management of patients with increased comorbidities: Results from a statewide registry
Sunday, May 15, 2022
2:45 PM – 4:00 PM
Location: Room 228
Mohit Butaney, Amit Patel, Detroit, MI, Ji Qi, Karandeep Singh, Anna Johnson, Ann Arbor, MI, Alison Levy*, Detroit, MI, Sabrina Noyes, Grand Rapids, MI, Khurshid Ghani, Ann Arbor, MI, Craig Rogers, Detroit, MI, Brian Lane, Grand Rapids, MI, for the Michigan Urological Surgery Improvement Collaborative, Ann Arbor, MI
Alison C. Levy, MD
MD
Henry Ford Hospital
Poster Presenter(s)
Introduction: Partial nephrectomy (PN) has been associated with a higher risk of perioperative complications and morbidity than radical nephrectomy (RN). Based on MUSIC’s experience with Notable Outcomes and Trackable Events after Surgery (NOTES) after prostatectomy, we developed a tool to define an uncomplicated recovery after radical nephrectomy (RN) or PN. In this study, we sought to evaluate the impact of comorbidities on peri-operative outcomes based on this tool.
Methods: MUSIC KIDNEY commenced data collection in June 2017. Data abstractors recorded clinical, radiographic, pathologic, and follow-up data for patients with newly diagnosed clinical T1 renal masses (cT1RMs) at 16 MUSIC practices with >90 physicians. Based on the newly developed KIDNEY NOTES tool, a prolonged length of stay (LOS>3 days after MIS, >5 days after open), prolonged warm ischemia time (WIT), extensive estimated blood loss (EBL), positive surgical margin (PSM), or an ED visit/readmission were considered deviations from an otherwise uncomplicated recovery after nephrectomy. Initial management decision and associated perioperative deviations were analyzed based on Charlson Comorbidity Index (CCI).
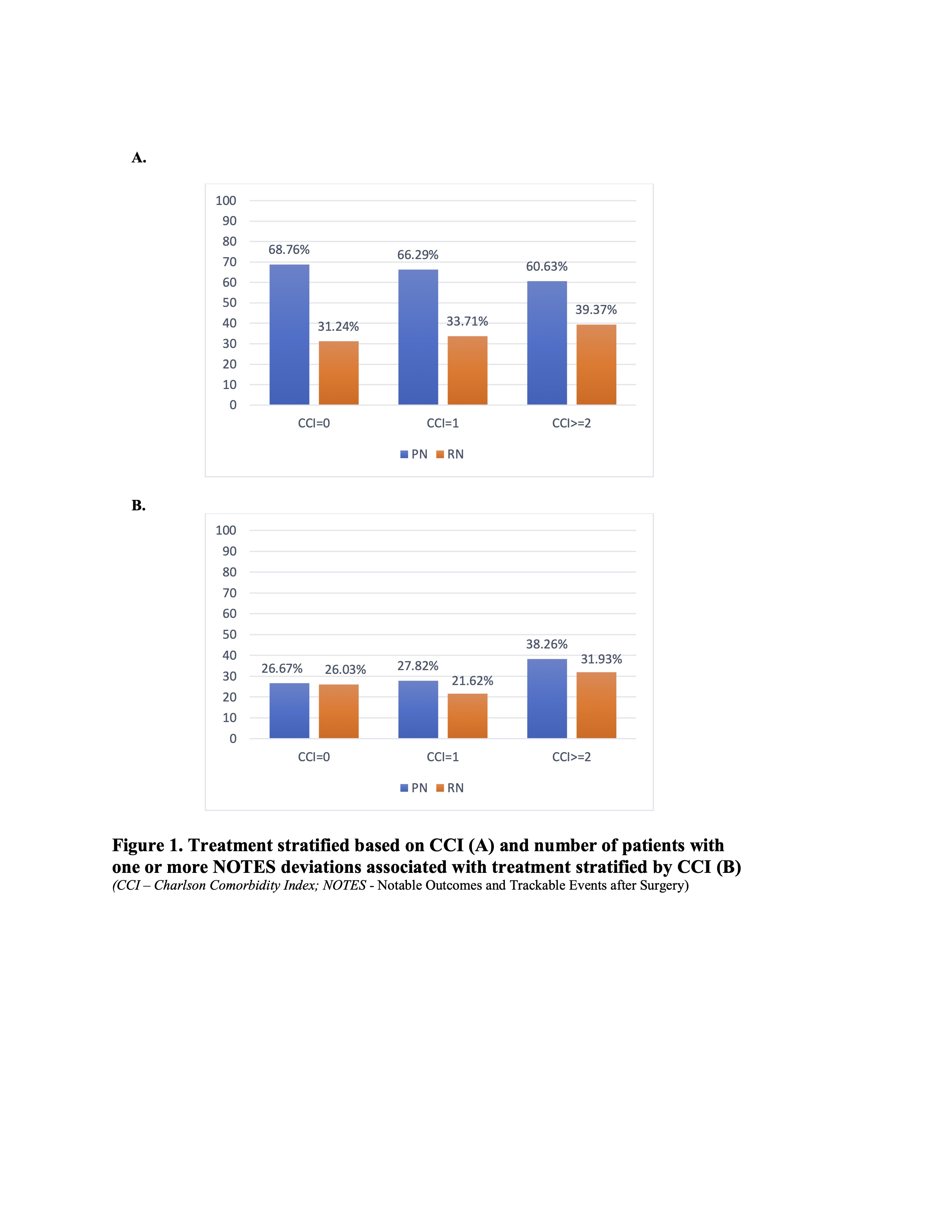
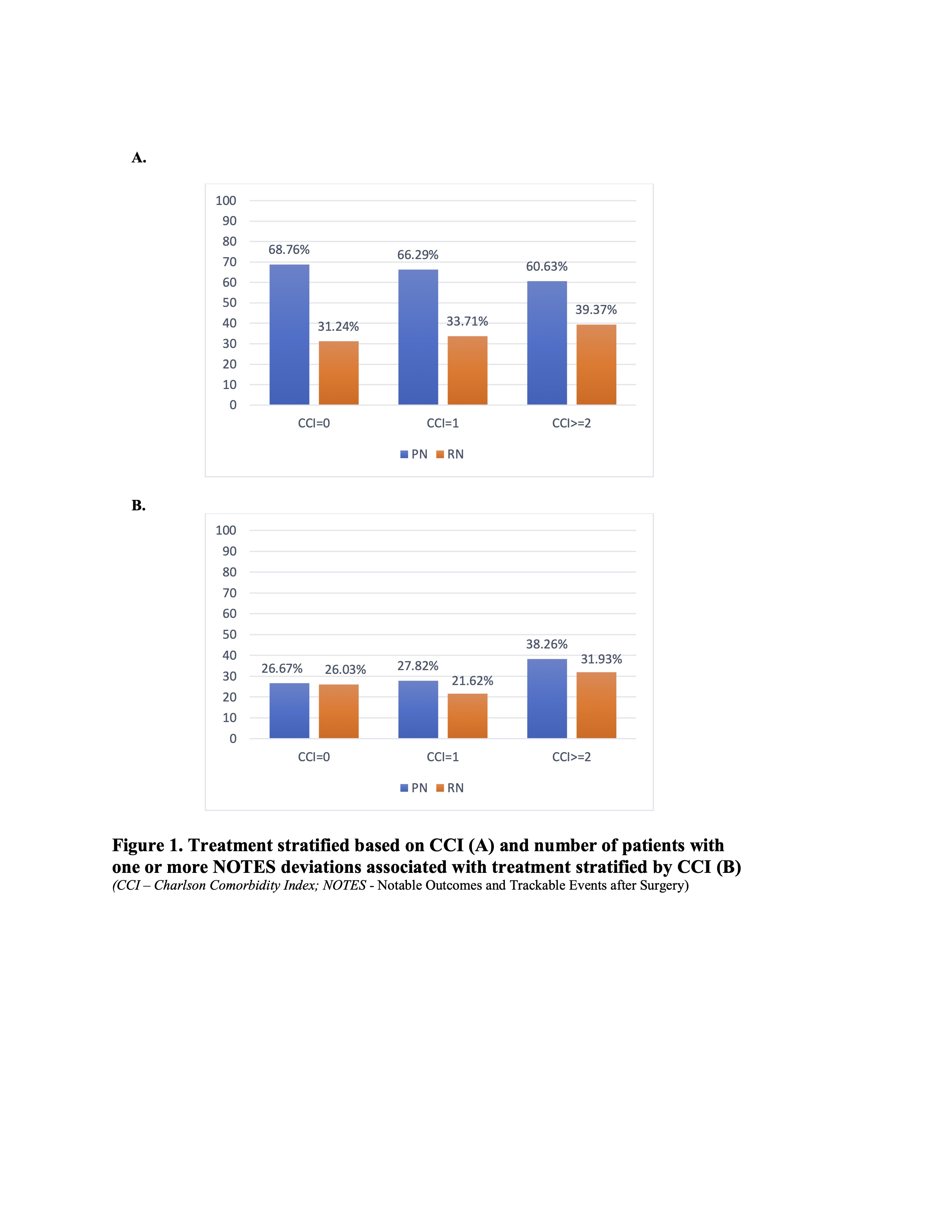
Results: Our study cohort consisted of 1395 patients including 927 patients who underwent PN and 468 who underwent a RN. 58.3%, 19.1% and 22.6% of patients fell into the CCI=0, CCI=1, and CCI>=2 groups. A higher CCI was associated with an increasing likelihood of the patient undergoing a RN (p=0.011) (Fig 1a). The proportion of patients with one or more NOTES deviation was found to be significantly higher with increasing CCI in PN (p=0.01 for PN, p=0.31 for RN, fig 1b).
Conclusions: The lower rate of PN in patients with increased comorbidities could be driven by patients more appropriately being treated on surveillance or RN as our data shows. Based on the NOTES deviations analysis, this is likely appropriate as patients treated with a PN have a higher number of deviations with increasing CCI. Specific comorbidities and factors driving these deviations need further investigation. As comorbidities and life expectancy are clearly an important variable to consider, the MUSIC-KIDNEY group developed a novel life expectancy calculator which is now live to aid treatment decision-making.
Source of Funding: Blue Cross Blue Shield of Michigan
Methods: MUSIC KIDNEY commenced data collection in June 2017. Data abstractors recorded clinical, radiographic, pathologic, and follow-up data for patients with newly diagnosed clinical T1 renal masses (cT1RMs) at 16 MUSIC practices with >90 physicians. Based on the newly developed KIDNEY NOTES tool, a prolonged length of stay (LOS>3 days after MIS, >5 days after open), prolonged warm ischemia time (WIT), extensive estimated blood loss (EBL), positive surgical margin (PSM), or an ED visit/readmission were considered deviations from an otherwise uncomplicated recovery after nephrectomy. Initial management decision and associated perioperative deviations were analyzed based on Charlson Comorbidity Index (CCI).
Results: Our study cohort consisted of 1395 patients including 927 patients who underwent PN and 468 who underwent a RN. 58.3%, 19.1% and 22.6% of patients fell into the CCI=0, CCI=1, and CCI>=2 groups. A higher CCI was associated with an increasing likelihood of the patient undergoing a RN (p=0.011) (Fig 1a). The proportion of patients with one or more NOTES deviation was found to be significantly higher with increasing CCI in PN (p=0.01 for PN, p=0.31 for RN, fig 1b).
Conclusions: The lower rate of PN in patients with increased comorbidities could be driven by patients more appropriately being treated on surveillance or RN as our data shows. Based on the NOTES deviations analysis, this is likely appropriate as patients treated with a PN have a higher number of deviations with increasing CCI. Specific comorbidities and factors driving these deviations need further investigation. As comorbidities and life expectancy are clearly an important variable to consider, the MUSIC-KIDNEY group developed a novel life expectancy calculator which is now live to aid treatment decision-making.
Source of Funding: Blue Cross Blue Shield of Michigan

.jpg)
.jpg)