Back
Poster, Podium & Video Sessions
Moderated Poster
MP47: Kidney Cancer: Epidemiology & Evaluation/Staging/Surveillance III
MP47-12: Frailty status predicts worse postoperative and long-term oncologic outcomes in patients treated with partial nephrectomy for small renal masses
Sunday, May 15, 2022
2:45 PM – 4:00 PM
Location: Room 228
Giuseppe Rosiello*, Giuseppe Fallara, Daniele Cignoli, Giuseppe Basile, Gianmarco Colandrea, Gianfranco Baiamonte, Isaline Rowe, Daniela Canibus, Giacomo Musso, Federico Belladelli, Francesco Cei, Cristina Giancristofaro, Milan, Italy, Pierre I. Karakiewicz, Montreal, Canada, Alberto Briganti, Roberto Bertini, Francesco Montorsi, Andrea Salonia, Alessandro Larcher, Umberto Capitanio, Milan, Italy

Giuseppe Rosiello, MD
Resident
San Raffaele Hospital
Poster Presenter(s)
Introduction: Partial nephrectomy (PN) represents the gold standard treatment of cT1a renal masses. However, most cT1a renal cell carcinomas (RCCs) are indolent and demonstrate excellent prognosis. Indicators of suboptimal outcomes after surgery, toghether with age or comorbidities, appears warranted. Thus, we investigated the impact of frailty status on postoperative and oncologic outcomes in patients undergoing PN for RCC.
Methods: Within a prospective maintained database, we identified 987 patients treated with PN for cT1aN0M0 RCC at a single tertiary centre between 2000-2021. The Modified Frailty Index was adopted to identify frail patients. Clavien-Dindo (CD) classification assessed postoperative complications. Cumulative incidence plots were used to test the effect of frailty on cancer-specific mortality (CSM) and other-cause mortality (OCM). Multivariable competing-risk analyses accounted for the effect of OCM on CSM, to provide the most unbiased estimates of CSM and OCM after adjusting for patient and tumor characteristics.
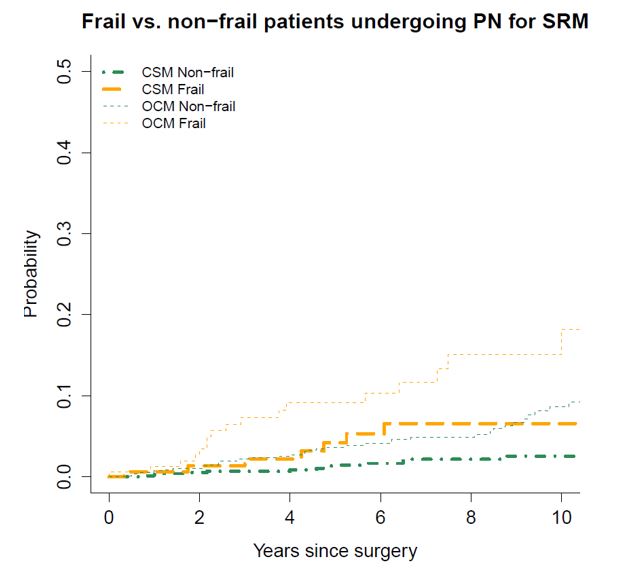
Results: Overall, 987 patients were treated with PN for cT1aN0M0 RCC. Of these, 17% patients were frail. Frail patients were older (70 vs. 60; p<0.01) and more frequently male (79 vs. 67%; p<0.01). Median tumor size did not differ between the two groups (p=0.1). Frailty status was associated with increased risk of CD >=3 complications (7 vs. 3%; p=0.01). Median follow-up was 67 (35-108) months. 22 patients died due to RCC while 68 died due to OCM. The 5- and 10-year CSM was 2.6 vs. 4.2% vs. 1.4 and 2.5% for frail vs. non-frail patients. Moreover, the 5- and 10-year OCM was 9.1 and 19% vs. 4.2 and 6.5% in frail vs. non-frail patients (Figure 1). At multivariable competing-risk analyses, frailty status predicted higher risk of CSM [HR: 1.78, 95%CI 1.05-3.0] and OCM (HR: 2.6, 95%CI 1.02-6.7; p=0.03).
Conclusions: Approximately, one out of five patients undergoing PN for small renal mass is frail. Frailty status is associated with increased risk of overall and major complications after PN. Moreover, the risk of OCM significantly overcomes the risk of dying due to RCC in frail patients. Thus, renal surgery should be weighted against the risk of suboptimal surgical outcomes and less invasive treatment modalities may be advocated in this population
Source of Funding: no
Methods: Within a prospective maintained database, we identified 987 patients treated with PN for cT1aN0M0 RCC at a single tertiary centre between 2000-2021. The Modified Frailty Index was adopted to identify frail patients. Clavien-Dindo (CD) classification assessed postoperative complications. Cumulative incidence plots were used to test the effect of frailty on cancer-specific mortality (CSM) and other-cause mortality (OCM). Multivariable competing-risk analyses accounted for the effect of OCM on CSM, to provide the most unbiased estimates of CSM and OCM after adjusting for patient and tumor characteristics.
Results: Overall, 987 patients were treated with PN for cT1aN0M0 RCC. Of these, 17% patients were frail. Frail patients were older (70 vs. 60; p<0.01) and more frequently male (79 vs. 67%; p<0.01). Median tumor size did not differ between the two groups (p=0.1). Frailty status was associated with increased risk of CD >=3 complications (7 vs. 3%; p=0.01). Median follow-up was 67 (35-108) months. 22 patients died due to RCC while 68 died due to OCM. The 5- and 10-year CSM was 2.6 vs. 4.2% vs. 1.4 and 2.5% for frail vs. non-frail patients. Moreover, the 5- and 10-year OCM was 9.1 and 19% vs. 4.2 and 6.5% in frail vs. non-frail patients (Figure 1). At multivariable competing-risk analyses, frailty status predicted higher risk of CSM [HR: 1.78, 95%CI 1.05-3.0] and OCM (HR: 2.6, 95%CI 1.02-6.7; p=0.03).
Conclusions: Approximately, one out of five patients undergoing PN for small renal mass is frail. Frailty status is associated with increased risk of overall and major complications after PN. Moreover, the risk of OCM significantly overcomes the risk of dying due to RCC in frail patients. Thus, renal surgery should be weighted against the risk of suboptimal surgical outcomes and less invasive treatment modalities may be advocated in this population
Source of Funding: no

.jpg)
.jpg)