Back
Poster, Podium & Video Sessions
Moderated Poster
MP47: Kidney Cancer: Epidemiology & Evaluation/Staging/Surveillance III
MP47-17: Impact of Patient and Lifestyle Factors in Patients with Stage III & IV Renal Cancer: A Danish Nationwide Study
Sunday, May 15, 2022
2:45 PM – 4:00 PM
Location: Room 228
Freja Ebbestad, Copenhagen , Denmark, Louise Geertsen, Odense, Denmark, Naomi Nadler, Roskilde, Denmark, Sofie Axelsen, Hjørring, Denmark, Trine Horsbøll, Odense, Denmark, Susanne Dalton, Copenhagen , Denmark, Jane Christensen, Copenhagen, Denmark, Frede Donskov, Aarhus, Denmark, Lars Lund, Odense, Denmark, Nessn Azawi*, Roskilde, Denmark
- NA
Poster Presenter(s)
Introduction: In this nationwide study, we investigated the effect of patient-related and lifestyle factors, and the use of multidisciplinary team meetings (MDT) in patient decision making, with overall and cancer-specific death, risk of recurrence and risk of death after recurrence as endpoints.
Methods: The study population included 949 patients with stage III and IV renal cancer, registered in the Danish Renal Cancer Database between 2014 and 2016 and followed until January 2021. Data sources were national registries supplemented with manual extraction of information from patient medical records. The hazard ratio (HR) with corresponding 95 % confidence intervals (CI) over overall death, cancer-specific death and recurrence were estimated using Cox proportional hazards regression with multivariate adjustment.
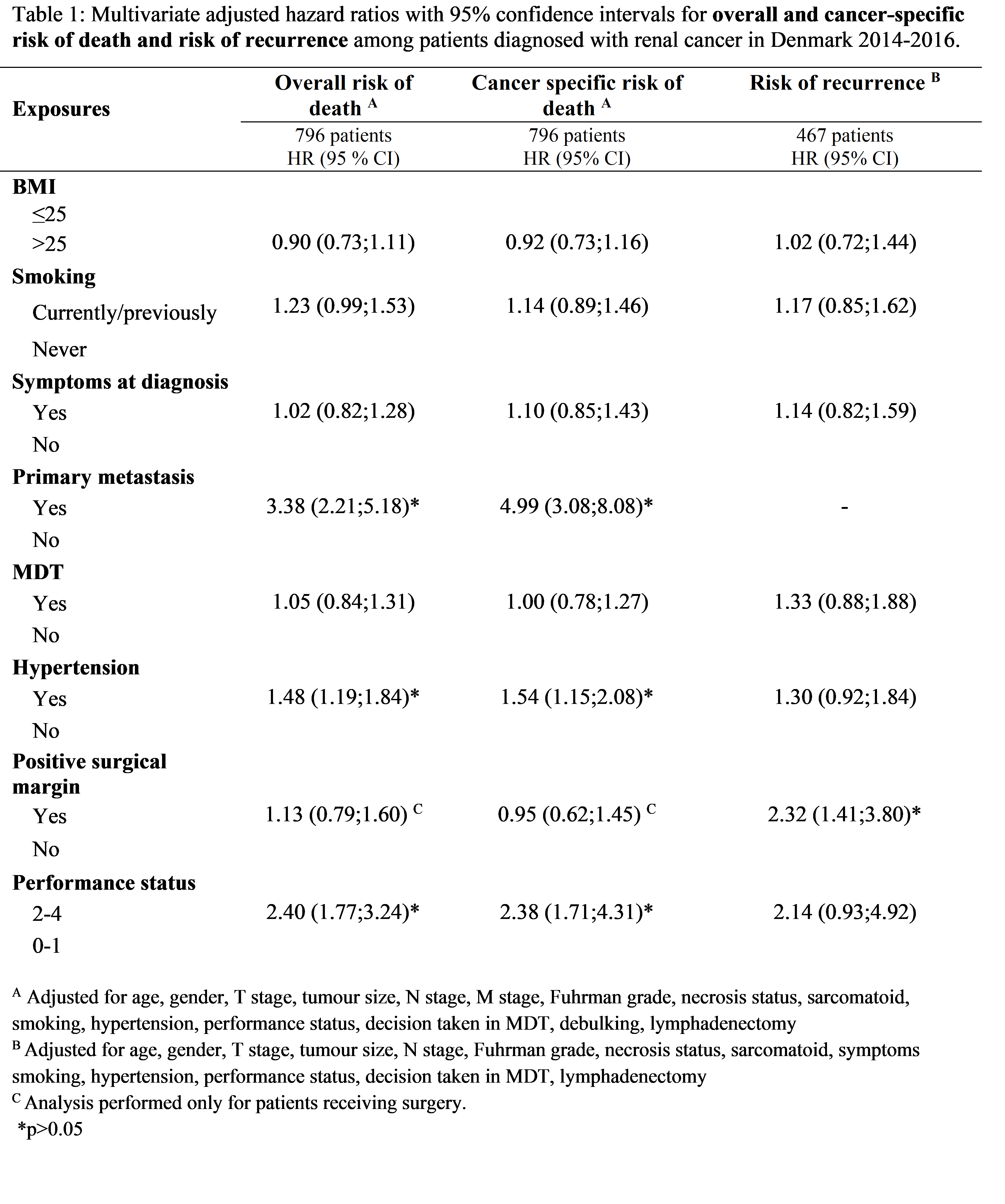
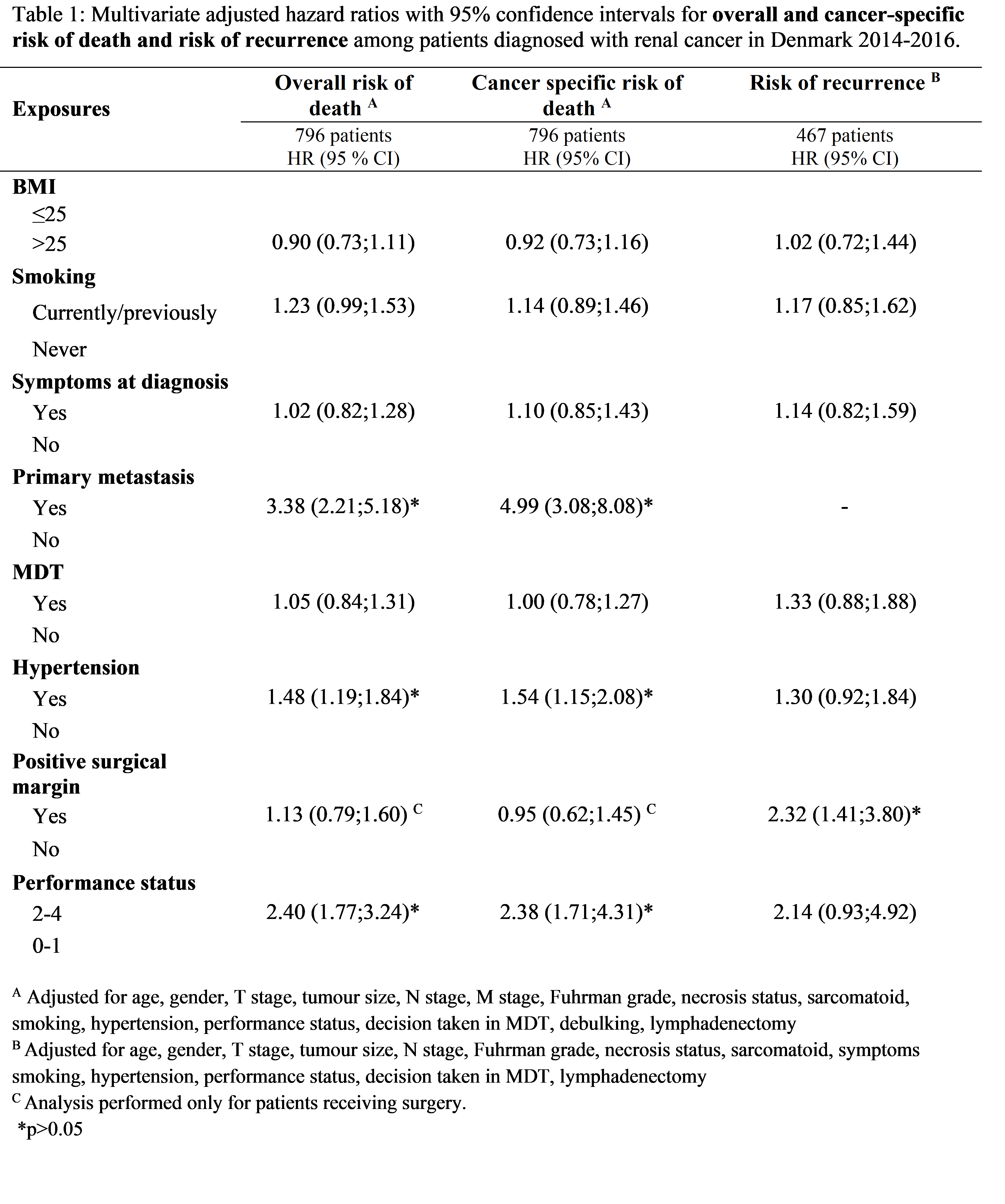
Results: Of 949 patients included, 502 (53 %) had localized disease only and 447 (47%) had stage IV at diagnosis; 625 (73%) had nephrectomy, 464 (49%) had treatment decisions made in MDT, and 526 (55%) had hypertension at diagnosis. Hypertension, poor performance status and primary metastasis increased the HR of both overall and cancer-specific death, while smoking was associated with a borderline increased HR of overall death (table 1). 167 of 500 patients (33%) had recurrence after nephrectomy; only positive surgical margin (HR: 2.32, CI: 1.41;3.80) was statistically significant for risk of recurrence. HR of overall death after recurrence was 0.63 (CI: 0.47;0.84) per year from primary diagnosis to the diagnosis of recurrence. When treatment of recurrence was solely oncological (HR: 4.02, CI: 1.52;10.59), or no treatment was given (HR: 3.57, CI: 1.11;11.44), patients had a higher risk of overall death compared to patients treated with surgery.
Conclusions: Patient-related factors such as hypertension and performance status were associated with survival and warrant attention in patient risk stratification. A longer time to recurrence reduced the risk of death after recurrence. Patients whose recurrence was treated without surgery had worse survival, confirming the role of surgery in treating advanced renal cancer.
Source of Funding: None
Methods: The study population included 949 patients with stage III and IV renal cancer, registered in the Danish Renal Cancer Database between 2014 and 2016 and followed until January 2021. Data sources were national registries supplemented with manual extraction of information from patient medical records. The hazard ratio (HR) with corresponding 95 % confidence intervals (CI) over overall death, cancer-specific death and recurrence were estimated using Cox proportional hazards regression with multivariate adjustment.
Results: Of 949 patients included, 502 (53 %) had localized disease only and 447 (47%) had stage IV at diagnosis; 625 (73%) had nephrectomy, 464 (49%) had treatment decisions made in MDT, and 526 (55%) had hypertension at diagnosis. Hypertension, poor performance status and primary metastasis increased the HR of both overall and cancer-specific death, while smoking was associated with a borderline increased HR of overall death (table 1). 167 of 500 patients (33%) had recurrence after nephrectomy; only positive surgical margin (HR: 2.32, CI: 1.41;3.80) was statistically significant for risk of recurrence. HR of overall death after recurrence was 0.63 (CI: 0.47;0.84) per year from primary diagnosis to the diagnosis of recurrence. When treatment of recurrence was solely oncological (HR: 4.02, CI: 1.52;10.59), or no treatment was given (HR: 3.57, CI: 1.11;11.44), patients had a higher risk of overall death compared to patients treated with surgery.
Conclusions: Patient-related factors such as hypertension and performance status were associated with survival and warrant attention in patient risk stratification. A longer time to recurrence reduced the risk of death after recurrence. Patients whose recurrence was treated without surgery had worse survival, confirming the role of surgery in treating advanced renal cancer.
Source of Funding: None

.jpg)
.jpg)