Back
Poster, Podium & Video Sessions
Moderated Poster
MP48: Prostate Cancer: Advanced (including Drug Therapy) III
MP48-01: How to optimize patient selection before salvage lymph node dissection for nodal recurrent prostate cancer: a novel risk stratification tool
Sunday, May 15, 2022
2:45 PM – 4:00 PM
Location: Room 225
Nicola Fossati*, Lugano, Switzerland, Jeffrey R. Karnes, Rochester, MN, David Pfister, Munich, Germany, Axel Heidenreich, Cologne, Germany, Alexander Kretschmer, Alexander Buchner, Christian Stief, Munich, Germany, Steven Joniau, Hendrik van Poppel, Leuven, Belgium, Daniar Osmonov, Klaus-Peter Juenemann, Kiel, Germany, Shahrokh Shariat, Vienna, Austria, Andreas Hiester, Peter Albers, Düsseldorf, Germany, Derya Tilki, Markus Graefen, Hamburg, Germany, Inderbir S. Gill, Los Angeles, CA, Elio Mazzone, Armando Stabile, Milan, Italy, Alexander Mottrie, Melle, Belgium, Giorgio Gandaglia, Milan, Italy, Andrea Gallina, Lugano, Switzerland, Francesco Montorsi, Alberto Briganti, Milano, Italy
- NF
Poster Presenter(s)
Introduction: Nodal recurrences represent the first and most frequent site of relapse after primary treatment for prostate cancer. Salvage lymph node dissection (SLND) is considered a possible treatment option for these patients as part of a multimodal approach. However, the outcome of SLND is highly heterogeneous, and patient selection is fundamental. As such, we aimed at developing a risk stratification tool, using a large multi-institutional series of patients treated with SLND.
Methods: We included 757 patients who received SLND at eleven tertiary referral centres. All patients were diagnosed with nodal recurrence after RP by PET/CT scan using either 11C-choline (n=579; 76%) or 68Ga-PSMA (n=178; 24%). The primary outcome measured was clinical recurrence (CR) after SLND, defined as positive PET/CT scan during follow-up. Regression tree analysis was used to develop a risk-stratification tool. The following variables were included in the regression tree: Gleason grade group, time from RP to SLND, hormonal therapy (HT) administration before SLND, retroperitoneum involvement at PET/CT, number of positive spots, and PSA level at SLND.
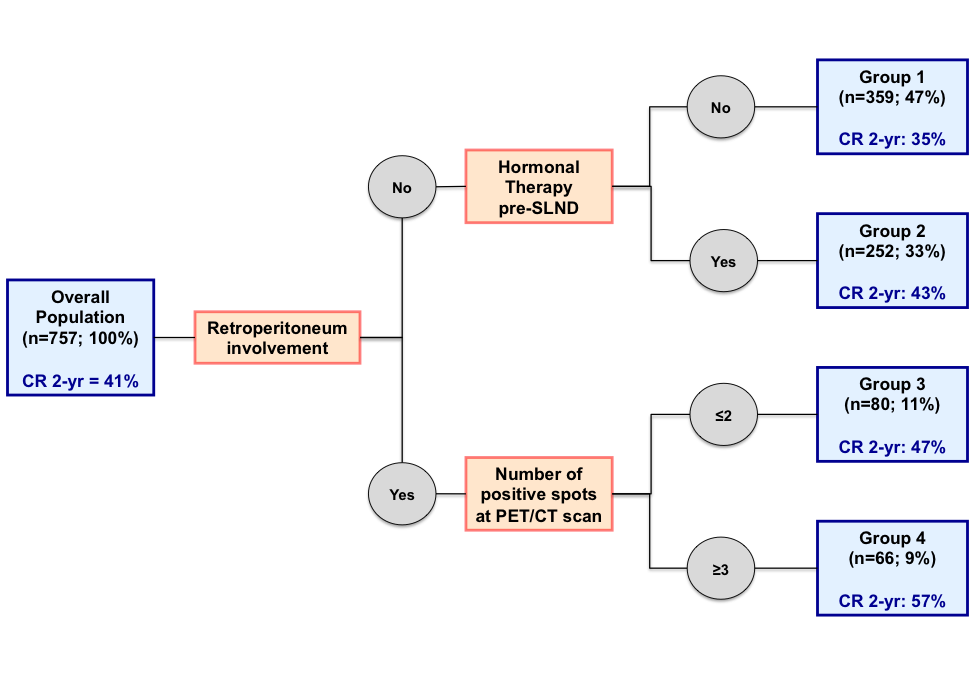
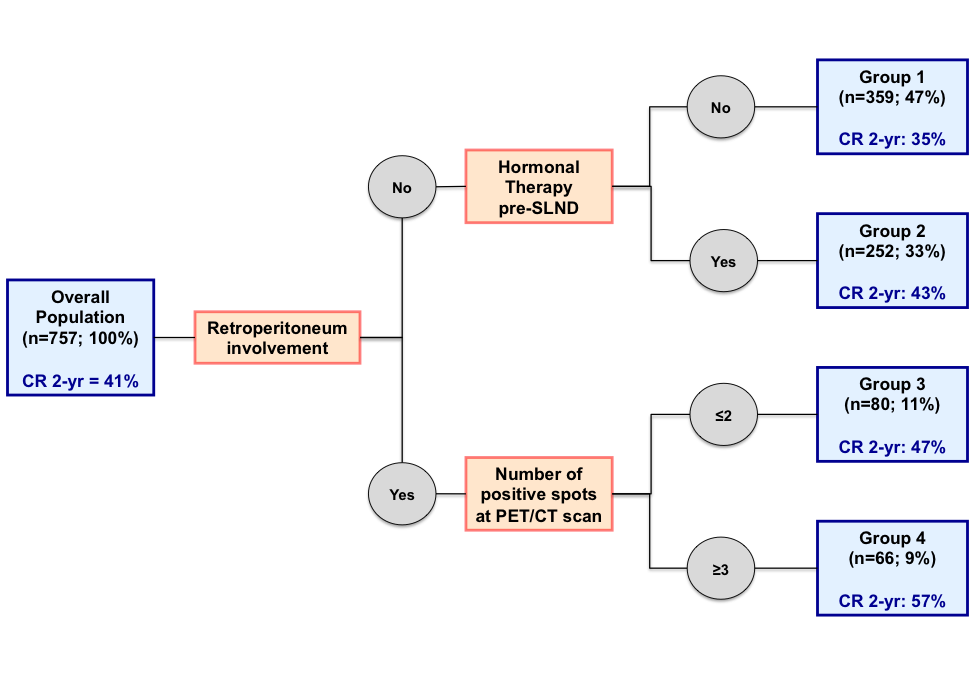
Results: At a median follow-up of 24 months, 428 (56%) patients experienced CR. Regression-tree analysis identified 4 prognostic risk groups (AUC: 77%) (Figure 1). Retroperitoneum involvement at PET/CT scan was the most significant predictor of CR. When retroperitoneum was not involved, patients were stratified by previous HT administration: no (Group 1: n=359; 47%) vs. yes (Group 2: n=252; 33%). On the other hand, when retroperitoneum was involved, patients were stratified according to the number of positive spots at PET/CT scan: =2 (Group 3: n=80; 11%) vs. =3 (Group 4: n=66; 94%). At Kaplan-Meier analysis, 2-yr CR rate was significantly different among groups: 35%, 43%, 47%, and 57%, respectively (p < 0.0001).
Conclusions: We developed an accurate risk stratification tool to facilitate the individualized recommendation for SLND based on tumour characteristics. This stratification tool may also be useful for trial design in the setting of nodal recurrent prostate cancer.
Source of Funding: none.
Methods: We included 757 patients who received SLND at eleven tertiary referral centres. All patients were diagnosed with nodal recurrence after RP by PET/CT scan using either 11C-choline (n=579; 76%) or 68Ga-PSMA (n=178; 24%). The primary outcome measured was clinical recurrence (CR) after SLND, defined as positive PET/CT scan during follow-up. Regression tree analysis was used to develop a risk-stratification tool. The following variables were included in the regression tree: Gleason grade group, time from RP to SLND, hormonal therapy (HT) administration before SLND, retroperitoneum involvement at PET/CT, number of positive spots, and PSA level at SLND.
Results: At a median follow-up of 24 months, 428 (56%) patients experienced CR. Regression-tree analysis identified 4 prognostic risk groups (AUC: 77%) (Figure 1). Retroperitoneum involvement at PET/CT scan was the most significant predictor of CR. When retroperitoneum was not involved, patients were stratified by previous HT administration: no (Group 1: n=359; 47%) vs. yes (Group 2: n=252; 33%). On the other hand, when retroperitoneum was involved, patients were stratified according to the number of positive spots at PET/CT scan: =2 (Group 3: n=80; 11%) vs. =3 (Group 4: n=66; 94%). At Kaplan-Meier analysis, 2-yr CR rate was significantly different among groups: 35%, 43%, 47%, and 57%, respectively (p < 0.0001).
Conclusions: We developed an accurate risk stratification tool to facilitate the individualized recommendation for SLND based on tumour characteristics. This stratification tool may also be useful for trial design in the setting of nodal recurrent prostate cancer.
Source of Funding: none.

.jpg)
.jpg)