Back
Poster, Podium & Video Sessions
Moderated Poster
MP48: Prostate Cancer: Advanced (including Drug Therapy) III
MP48-10: Androgen Deprivation Therapy for Node-Positive Prostate Cancer at Radical Prostatectomy and Pelvic Lymph Node Dissection: Contemporary Practice Patterns and Associated Factors
Sunday, May 15, 2022
2:45 PM – 4:00 PM
Location: Room 225
Leilei Xia, Ruchika Talwar, Raju Chelluri*, Daniel Lee, Thomas Guzzo, Philadelphia, PA
- RC
Poster Presenter(s)
Introduction: Current guidelines recommend observation or adjuvant androgen deprivation therapy (ADT) with or without external beam radiation therapy (EBRT) for node-positive prostate cancer at radical prostatectomy (RP) and pelvic lymph node dissection (PLND). There is limited data on contemporary practice patterns and factors associated with the usage of ADT at the national level.
Methods: Patients with cT1-2N0M0 prostate cancer diagnosed between 2006 and 2015 who underwent RP and PLND and then were found to have pathologically positive lymph node (LN) were identified from National Cancer Database (NCDB). Patients were stratified into 3 cohorts based on the number of positive LNs (1 LN vs. 2 LNs vs. = 3 LNs). Some of the covariables included hospital volume of RP (low vs. medium vs. high), more extended PLND (=11 nodes vs. <11 nodes removed), positive surgical margin (PSM), and pT stage (pT3-4 vs. pT2). Primary outcome was ADT usage (with or without the EBRT).
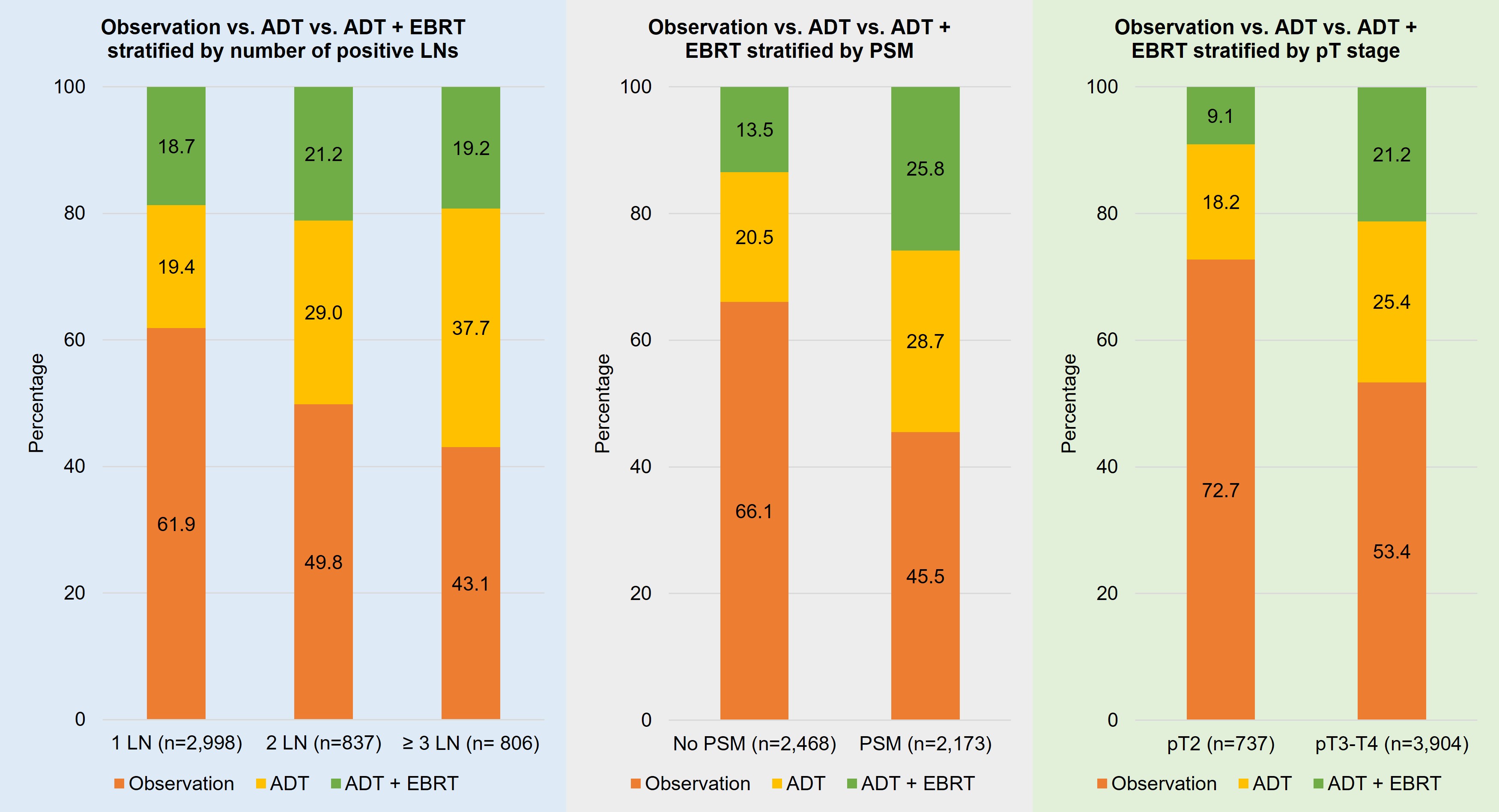
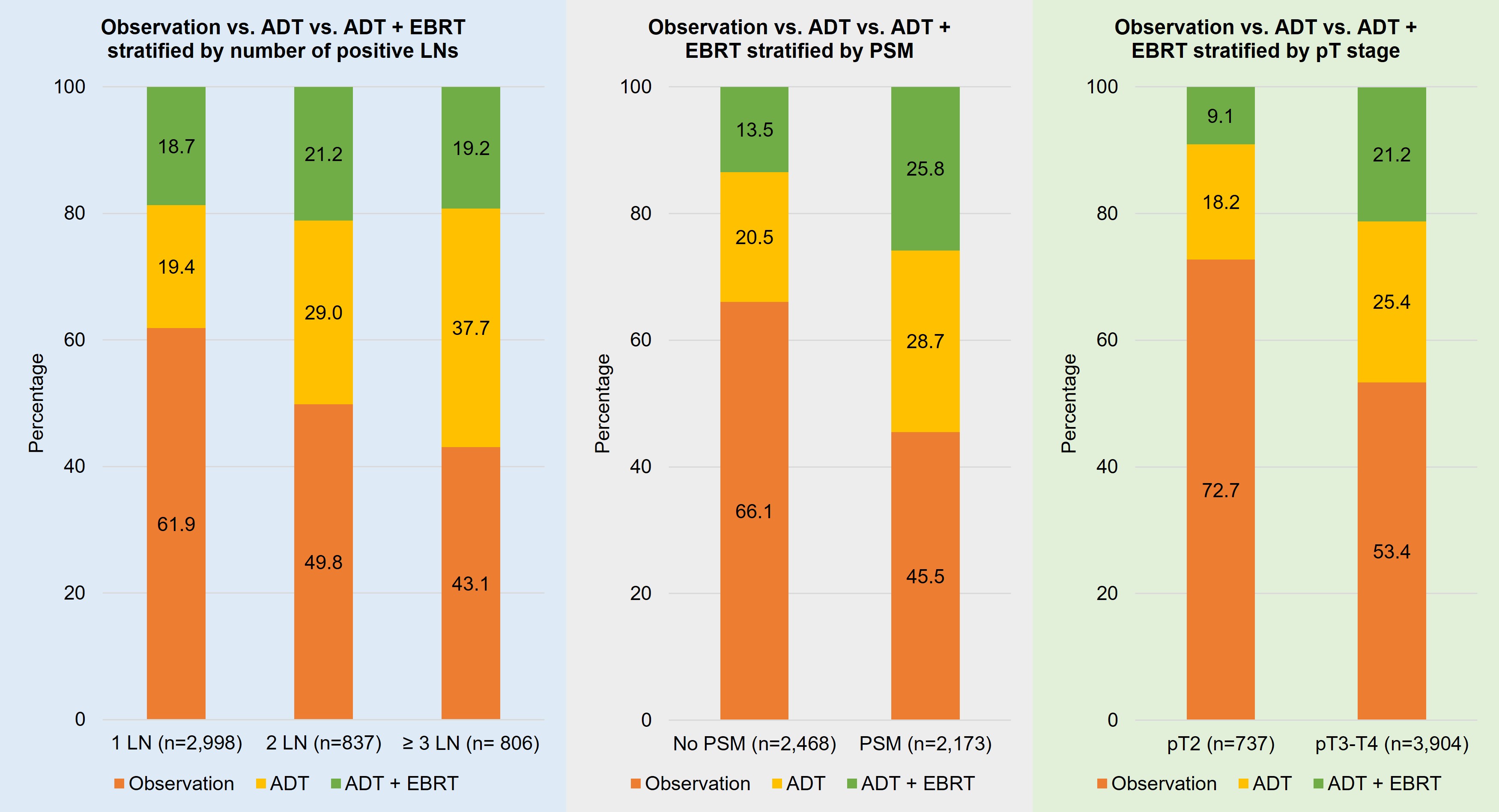
Results: A total of 4,641 patients were included: 2,998 patients with 1 positive LN, 837 with 2 positive LNs, and 806 with =3 positive LNs. In the overall cohort, 56.4% did not receive ADT, 24.3% received ADT only, and 19.2% received ADT+EBRT. The distributions of observation vs. ADT vs. ADT+EBRT stratified by positive LNs, PSM, and pT stage are shown in the Figure. Multivariable logistic regressions showed that compared with 1 LN, 2 LNs (odds ratio [OR]=1.49, P<0.001) and = 3 LNs (OR=1.83, P<0.001) were associated with higher odds of receiving ADT. Patients with PSM (OR=1.81, P<0.001) and pT3-4 cancer (OR=1.65, P<0.001) were significantly more likely to receive ADT. More extended PLND was associated with lower odds of receiving ADT (OR=0.76, P<0.001). Compared with low RP volume, patients who had RP at medium volume (OR=0.80, P=0.005) and high volume (OR=0.66, P<0.001) hospitals were less likely to receive ADT.
Conclusions: This NCDB study suggests that clinicians have been selectively offering ADT based on adverse pathological features and extension of PLND. Variations of ADT usage among hospitals may be related to RP surgical volumes. These findings have implications for patient counseling, policymaking, and further trial design for these groups of aggressive and heterogeneous cancers.
Source of Funding: NA
Methods: Patients with cT1-2N0M0 prostate cancer diagnosed between 2006 and 2015 who underwent RP and PLND and then were found to have pathologically positive lymph node (LN) were identified from National Cancer Database (NCDB). Patients were stratified into 3 cohorts based on the number of positive LNs (1 LN vs. 2 LNs vs. = 3 LNs). Some of the covariables included hospital volume of RP (low vs. medium vs. high), more extended PLND (=11 nodes vs. <11 nodes removed), positive surgical margin (PSM), and pT stage (pT3-4 vs. pT2). Primary outcome was ADT usage (with or without the EBRT).
Results: A total of 4,641 patients were included: 2,998 patients with 1 positive LN, 837 with 2 positive LNs, and 806 with =3 positive LNs. In the overall cohort, 56.4% did not receive ADT, 24.3% received ADT only, and 19.2% received ADT+EBRT. The distributions of observation vs. ADT vs. ADT+EBRT stratified by positive LNs, PSM, and pT stage are shown in the Figure. Multivariable logistic regressions showed that compared with 1 LN, 2 LNs (odds ratio [OR]=1.49, P<0.001) and = 3 LNs (OR=1.83, P<0.001) were associated with higher odds of receiving ADT. Patients with PSM (OR=1.81, P<0.001) and pT3-4 cancer (OR=1.65, P<0.001) were significantly more likely to receive ADT. More extended PLND was associated with lower odds of receiving ADT (OR=0.76, P<0.001). Compared with low RP volume, patients who had RP at medium volume (OR=0.80, P=0.005) and high volume (OR=0.66, P<0.001) hospitals were less likely to receive ADT.
Conclusions: This NCDB study suggests that clinicians have been selectively offering ADT based on adverse pathological features and extension of PLND. Variations of ADT usage among hospitals may be related to RP surgical volumes. These findings have implications for patient counseling, policymaking, and further trial design for these groups of aggressive and heterogeneous cancers.
Source of Funding: NA

.jpg)
.jpg)