Back
Poster, Podium & Video Sessions
Moderated Poster
MP48: Prostate Cancer: Advanced (including Drug Therapy) III
MP48-18: The impact of locoregional treatments for metastatic castration resistant prostate cancer on disease progression: real life experience from a multicenter cohort
Sunday, May 15, 2022
2:45 PM – 4:00 PM
Location: Room 225
Mariaconsiglia Ferriero*, Gabriele Tuderti, Umberto Anceschi, Alfredo Maria Bove, Aldo Brassetti, Leonardo Misuraca, Salvatore Guaglianone, Riccardo Mastroianni, Cosimo De Nunzio, Silvana Giacinti, Giorgia Tema, Rome, Italy, Luca Cindolo, Vasto, Italy, Andrea Tubaro, Michele Gallucci, Rome, Italy, Luigi Schips, Vasto, Italy, Fabio Calabrò, Giuseppe Simone, Rome, Italy

Mariaconsiglia Ferriero, MD, PHD
Consultant Urologist
Sapienza University of Rome, Italy
Poster Presenter(s)
Introduction: Available evidences on medical treatment of metastatic castration resistant prostate cancer (mCRPC), support the use of more than one therapy line to delay chemotherapy. In this study, we evaluate the role of locoregional treatments on disease progression of patients with mCRPC treated with Abiraterone Acetate (AA), and Enzalutamide (EZ) in a chemo-naïve setting from a longitudinal real life multicenter cohort.
Methods: We prospectively collected data on chemo-naïve mCRPC patients, who received either AA or EZ as first or second line treatment between Oct-2012 and Nov-2020 at 4 centers. Survival probabilities were computed at 12, 24, 48 and 60 months after treatment start. The impact of loco-regional treatments on progression free survival (PFS) were assessed with the Kaplan Meier method and the log-rank test was applied to assess statistical significance between groups.
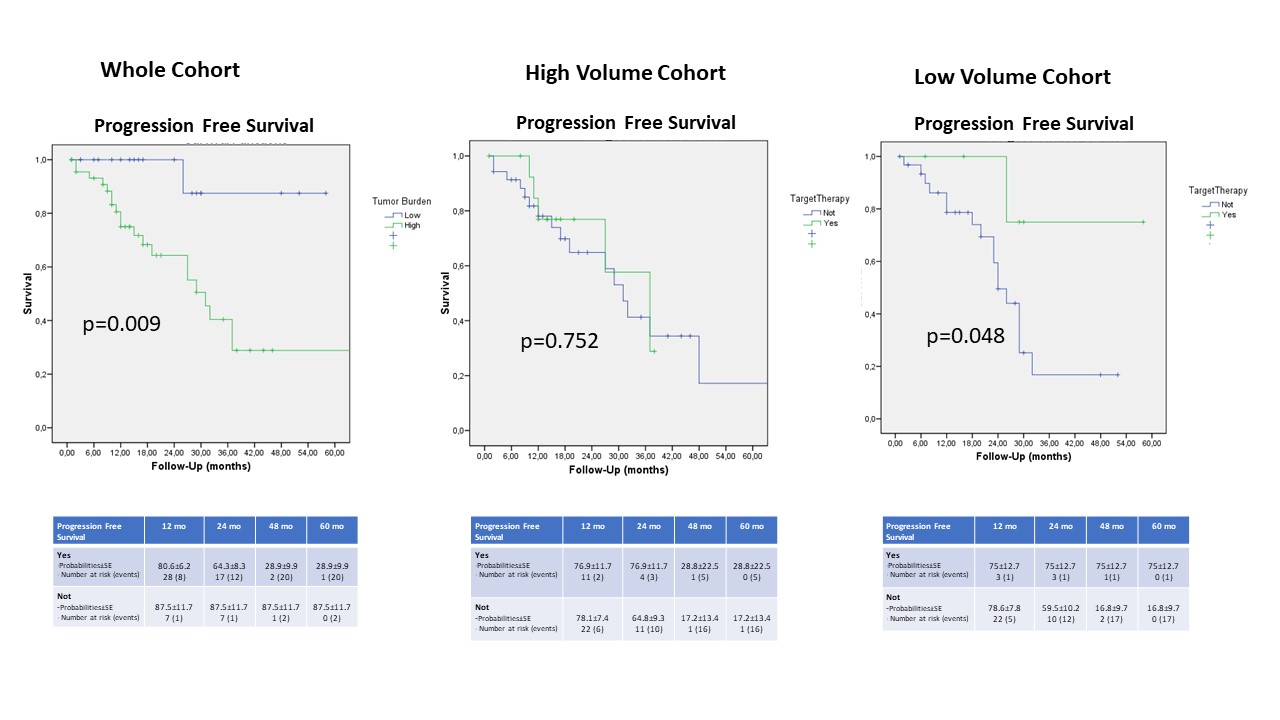
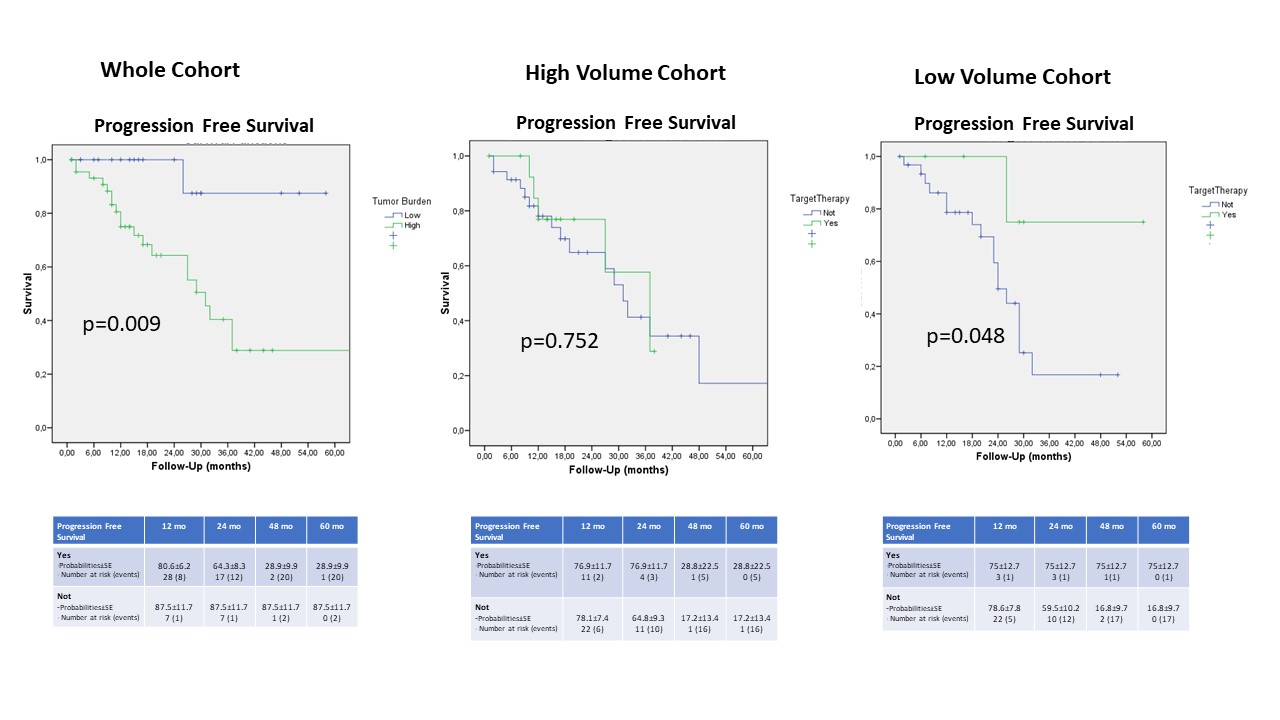
Results: Overall, 117 chemo-naive mCRPC patients received a first line therapy. Clinical features of the cohort are reported in Table 1. Fifty-seven (48.7%) patients received AA and 60 (51.3%) received EZ. Eight (6.7%) patients underwent salvage chemotherapy after first line failure. Overall, 28 patients shifted to a second line therapy. Two-yr progression-free, cancer-specific and overall survival probabilities were 65.5%, 82.2% and 78.4% respectively. Since diagnosis of mCRPC, oligo progression occurred in 25 patients who received stereotactic radiation therapy ( 23/25, 92%) focused on metastasis (4 nodal sites and 19 bones) or salvage lymph node dissection (2/25, 8%). At Kaplan Meier analysis, high volume disease was significant predictors of lower PFS probabilities (log rank p=0.009). Loco-regional treatments did not impact significantly in PFS of the whole cohort and in patients with high volume disease (p=0.605 and p=0.752), while improved significantly PFS in patients with low volume disease (p=0.048). (Fig. 1)
Conclusions: Loco-regional therapies significantly impact on PFS in patients with low volume mCRPC disease and are useful treatments option to delay next line of therapy.
Source of Funding: None
Methods: We prospectively collected data on chemo-naïve mCRPC patients, who received either AA or EZ as first or second line treatment between Oct-2012 and Nov-2020 at 4 centers. Survival probabilities were computed at 12, 24, 48 and 60 months after treatment start. The impact of loco-regional treatments on progression free survival (PFS) were assessed with the Kaplan Meier method and the log-rank test was applied to assess statistical significance between groups.
Results: Overall, 117 chemo-naive mCRPC patients received a first line therapy. Clinical features of the cohort are reported in Table 1. Fifty-seven (48.7%) patients received AA and 60 (51.3%) received EZ. Eight (6.7%) patients underwent salvage chemotherapy after first line failure. Overall, 28 patients shifted to a second line therapy. Two-yr progression-free, cancer-specific and overall survival probabilities were 65.5%, 82.2% and 78.4% respectively. Since diagnosis of mCRPC, oligo progression occurred in 25 patients who received stereotactic radiation therapy ( 23/25, 92%) focused on metastasis (4 nodal sites and 19 bones) or salvage lymph node dissection (2/25, 8%). At Kaplan Meier analysis, high volume disease was significant predictors of lower PFS probabilities (log rank p=0.009). Loco-regional treatments did not impact significantly in PFS of the whole cohort and in patients with high volume disease (p=0.605 and p=0.752), while improved significantly PFS in patients with low volume disease (p=0.048). (Fig. 1)
Conclusions: Loco-regional therapies significantly impact on PFS in patients with low volume mCRPC disease and are useful treatments option to delay next line of therapy.
Source of Funding: None

.jpg)
.jpg)