Back
Poster, Podium & Video Sessions
Moderated Poster
MP49: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Basic Research & Pathophysiology
MP49-07: Autonomic symptom score is greater in interstitial cystitis patients exhibiting a non-bladder-centric phenotype
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 228
Dylan T. Wolff*, Peyton Lee, Robert J. Evans, Gopal Badlani, Catherine A. Matthews, Stephen J. Walker, Winston-Salem, NC

Dylan T. Wolff, MD
Atrium Health Wake Forest Baptist
Poster Presenter(s)
Introduction: Symptoms of autonomic system dysfunction may be more common in patients with interstitial cystitis/bladder pain syndrome (IC/BPS). The purpose of this study was to examine the association between autonomic symptom severity and co-occurring symptoms/syndromes in a cohort of IC/BPS patients.
Methods: The Composite Autonomic Symptom Score (COMPASS-31) questionnaire, a validated self-assessment instrument for autonomic symptoms and function, was administered to 86 patients diagnosed with IC/BPS. All the patients have undergone therapeutic hydrodistension (HOD). Data collected include anesthetic bladder capacity (BC), Hunner’s lesion (HL) status, results for validated IC/BPS symptom questionnaires including pain and urgency/frequency symptom scale (PUF) and O’Leary Sant Interstitial Cystitis Symptom and Problem Indices (ICSI/ICPI), and a ‘yes/no’ answer for comorbid non-urologic associated syndromes (NUAS) known to co-occur with IC/BPS. The median COMPASS-31 score (scale of 0-100; higher scores show more severe dysautonomia) was 34.5, therefore patients were divided into two groups: (1) those with COMPASS score >34.5 (N=43), and (2) those with a score <34.5 (N=43). Clinical data were compared to autonomic symptom severity using Fisher’s Exact (categorical) and Wilcoxon Rank Sum (continuous) tests.
Results: Patients with more severe dysautonomia (COMPASS-31 score >34.5) were younger (47.95 vs 55.28; p=0.035), more likely to be female (95.3% vs 79.1%; p=0.049), less likely to have Hunner’s lesions (4.7% vs 19%; p=0.049), had a higher PUF score (25.89 vs 21.82; p=0.001), and had a higher number of NUAS (5.39 vs 3.05; p<0.001). These included a significantly higher incidence of pelvic floor dysfunction (52.6% vs 26.2%; p=0.022), fibromyalgia (52.6% vs 16.7%; p<0.001), chronic fatigue syndrome (26.3% vs 7.1%; p=0.032), migraines (50% vs 26.2%; p=0.038), and allergies (65.8% vs 42.9%; p=0.046). Additionally, both endometriosis and chronic pelvic pain approached, but did not reach significance (39.5% vs 21.4%; p=0.092 and 50% vs 28.6%; p=0.067, respectively).
Conclusions: A COMPASS-31 score >34.5 (i.e., higher degree of autonomic symptom severity) was found to correlate with a non-bladder centric phenotype (e.g., HL-, multiple comorbidities) in patients with IC/BPS.
Source of Funding: 1R01DK124599-01, R21DK106554-01
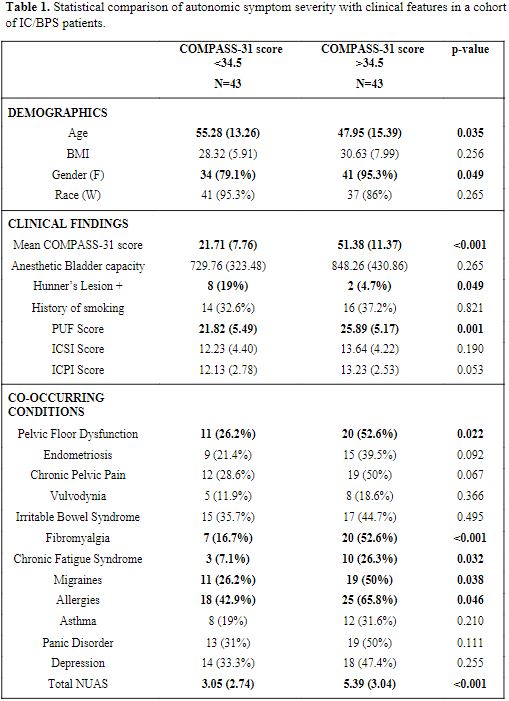
Methods: The Composite Autonomic Symptom Score (COMPASS-31) questionnaire, a validated self-assessment instrument for autonomic symptoms and function, was administered to 86 patients diagnosed with IC/BPS. All the patients have undergone therapeutic hydrodistension (HOD). Data collected include anesthetic bladder capacity (BC), Hunner’s lesion (HL) status, results for validated IC/BPS symptom questionnaires including pain and urgency/frequency symptom scale (PUF) and O’Leary Sant Interstitial Cystitis Symptom and Problem Indices (ICSI/ICPI), and a ‘yes/no’ answer for comorbid non-urologic associated syndromes (NUAS) known to co-occur with IC/BPS. The median COMPASS-31 score (scale of 0-100; higher scores show more severe dysautonomia) was 34.5, therefore patients were divided into two groups: (1) those with COMPASS score >34.5 (N=43), and (2) those with a score <34.5 (N=43). Clinical data were compared to autonomic symptom severity using Fisher’s Exact (categorical) and Wilcoxon Rank Sum (continuous) tests.
Results: Patients with more severe dysautonomia (COMPASS-31 score >34.5) were younger (47.95 vs 55.28; p=0.035), more likely to be female (95.3% vs 79.1%; p=0.049), less likely to have Hunner’s lesions (4.7% vs 19%; p=0.049), had a higher PUF score (25.89 vs 21.82; p=0.001), and had a higher number of NUAS (5.39 vs 3.05; p<0.001). These included a significantly higher incidence of pelvic floor dysfunction (52.6% vs 26.2%; p=0.022), fibromyalgia (52.6% vs 16.7%; p<0.001), chronic fatigue syndrome (26.3% vs 7.1%; p=0.032), migraines (50% vs 26.2%; p=0.038), and allergies (65.8% vs 42.9%; p=0.046). Additionally, both endometriosis and chronic pelvic pain approached, but did not reach significance (39.5% vs 21.4%; p=0.092 and 50% vs 28.6%; p=0.067, respectively).
Conclusions: A COMPASS-31 score >34.5 (i.e., higher degree of autonomic symptom severity) was found to correlate with a non-bladder centric phenotype (e.g., HL-, multiple comorbidities) in patients with IC/BPS.
Source of Funding: 1R01DK124599-01, R21DK106554-01

.jpg)
.jpg)