Back
Poster, Podium & Video Sessions
Moderated Poster
MP49: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Basic Research & Pathophysiology
MP49-15: Overactive Bladder Medication; How Long Should It Be Continued? - Mirabegron Interferes with Central Sensitization in a Mouse Model of Overactive Bladder.
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 228
Joonbeom Kwon*, Eun-Ju Lee, Hye-Ri Park, Hyun-Jung Cho, Ji-Ae Jang, Daegu, Korea, Republic of, Donghwi Park, Ulsan, Korea, Republic of, Naoki Yoshimura, Pittsburgh, PA
Poster Presenter(s)
Introduction: The etiology of overactive bladder (OAB) is multifactorial, and bladder afferent hyperexcitability has been proposed to be one of the contributing factors. In addition, chronic afferent hyperexcitability may induce neural remodeling in the central nervous system (CNS). However, there has been no clear pathophysiologic evidence determining how long OAB treatments should be continued. We, therefore, investigated the CNS effect of mirabegron using an OAB animal model and compared the therapeutic effect between treatment cessation (CES) and continuation (CON) groups.
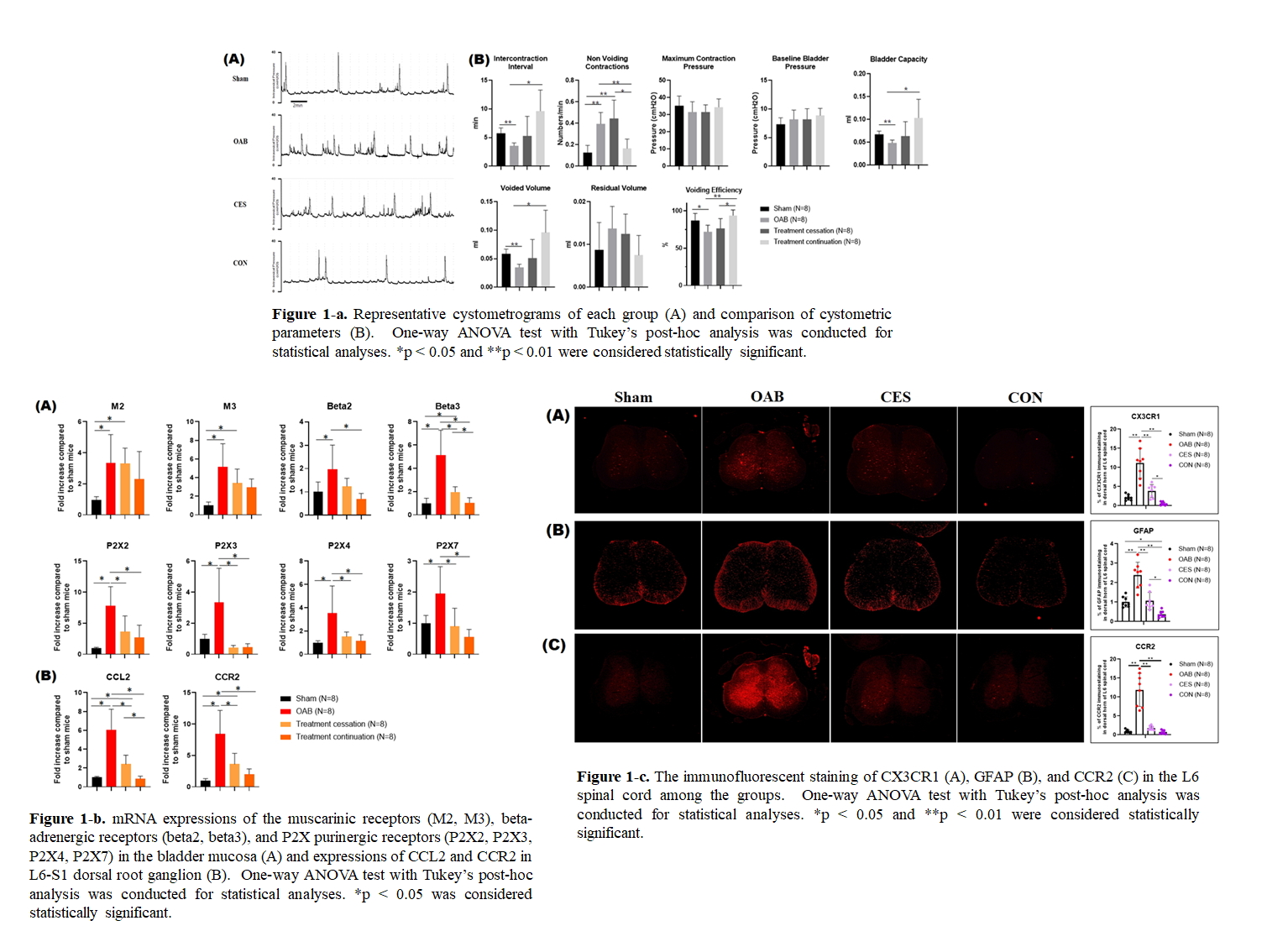
Methods: Female C57BL/6 mice were divided into 4 groups (N=8 in each): Sham, OAB, CES, and CON groups. OAB was induced by 3-times weekly intravesical instillations of KCl and hyaluronidase. Mirabegron (2mg/kg) was administered for 10 and 20 days in CES and CON groups, respectively. Cystometry was performed, and mRNA levels of bladder muscarinic, ß-adrenergic, and P2X purinergic receptors were measured. CCL2 and CCR2 in L6-S1 dorsal root ganglia (DRG), as afferent markers, and CX3CR1, GFAP, and CCR2 in the L6 spinal cord, as markers of glial activation and central sensitization, were also evaluated by RT-PCR and immunohistology.
Results: OAB mice showed bladder overactivity and inefficient voiding (Fig 1-a) with increased M2, M3, P2X2, P2X3, P2X4, and P2X7 levels in the bladder and increased CCL2 and CCR2 in DRG, indicating afferent hyperexcitability (Fig 1-b). CX3CR1, GFAP, and CCR2 in the L6 spinal cord were upregulated in the OAB group (Fig 1-c). However, CON mice exhibited improvements of all these parameters of afferent hyperexcitability and central sensitization. Also, CON mice showed better voiding efficiency and reduced CNS changes compared with CES mice.
Conclusions: Central sensitization may be an important pathophysiological mechanism of OAB. Continuous treatment of OAB with mirabegron seems to prevent the process of central sensitization via improvement of CNS neural remodeling. Therefore, continuous OAB medication may be desirable for long-term disease control.
Source of Funding: Astellas Pharma. Co.Ltd. (ISR005728)
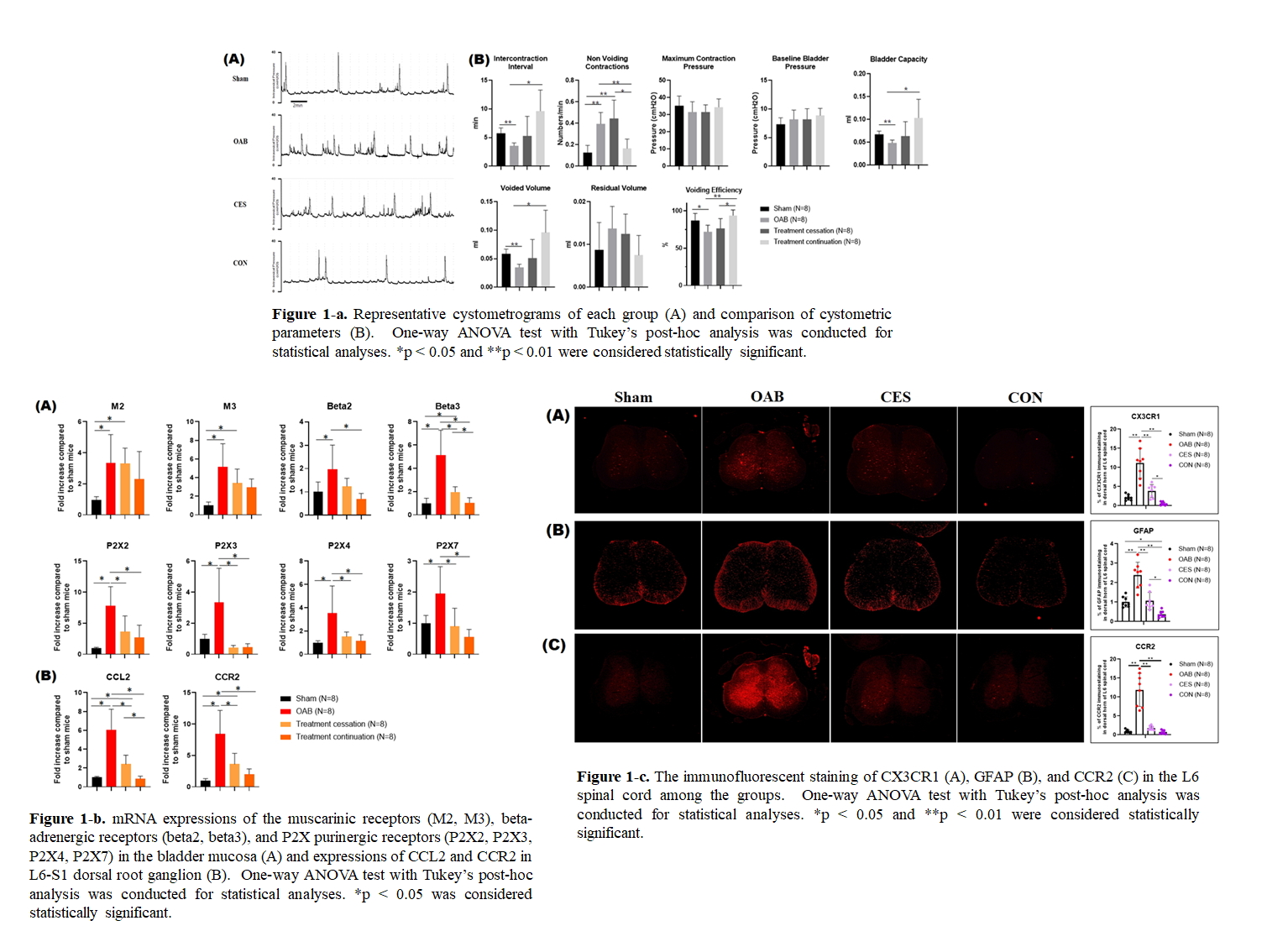
Methods: Female C57BL/6 mice were divided into 4 groups (N=8 in each): Sham, OAB, CES, and CON groups. OAB was induced by 3-times weekly intravesical instillations of KCl and hyaluronidase. Mirabegron (2mg/kg) was administered for 10 and 20 days in CES and CON groups, respectively. Cystometry was performed, and mRNA levels of bladder muscarinic, ß-adrenergic, and P2X purinergic receptors were measured. CCL2 and CCR2 in L6-S1 dorsal root ganglia (DRG), as afferent markers, and CX3CR1, GFAP, and CCR2 in the L6 spinal cord, as markers of glial activation and central sensitization, were also evaluated by RT-PCR and immunohistology.
Results: OAB mice showed bladder overactivity and inefficient voiding (Fig 1-a) with increased M2, M3, P2X2, P2X3, P2X4, and P2X7 levels in the bladder and increased CCL2 and CCR2 in DRG, indicating afferent hyperexcitability (Fig 1-b). CX3CR1, GFAP, and CCR2 in the L6 spinal cord were upregulated in the OAB group (Fig 1-c). However, CON mice exhibited improvements of all these parameters of afferent hyperexcitability and central sensitization. Also, CON mice showed better voiding efficiency and reduced CNS changes compared with CES mice.
Conclusions: Central sensitization may be an important pathophysiological mechanism of OAB. Continuous treatment of OAB with mirabegron seems to prevent the process of central sensitization via improvement of CNS neural remodeling. Therefore, continuous OAB medication may be desirable for long-term disease control.
Source of Funding: Astellas Pharma. Co.Ltd. (ISR005728)

.jpg)
.jpg)
